Abstract
Ductal carcinoma in situ (DCIS) of the breast represents 15–20 % of new breast cancer diagnoses in the US annually. However, long-term competing risks of mortality, as well as racial differences in outcomes among US women with DCIS, are unknown. Case data from the years 1978–2010 were obtained using SEER*Stat software available through the National Cancer Institute from the 2010 SEER registries. Included were all women aged 40 and over with newly diagnosed DCIS. There were 67,514 women in the analysis, including 54,518 white women and 6,113 black women. A total of 12,173 deaths were observed over 607,287 person-years of follow-up. The 20-year cumulative incidence of all-cause death among women with DCIS was 39.6 % (CI 38.9–40.3). The corresponding 20-year rates for breast cancer death and CVD death were 3.2 % (CI 3.0–3.4) and 13.2 % (CI 12.8–13.7), respectively. Black women with DCIS had a higher risk of death compared to white women, with these hazard ratios elevated throughout the entire study period. For example, between 1990 and 2010, black women had a higher risk of all-cause death (HR 3.06, CI 2.39–3.91), breast cancer death (HR 5.78, CI 3.16–10.57), and CVD death (HR 6.43, CI 3.61–11.45) compared to white women diagnosed between 50 and 59 years of age. The risk of all-cause and CVD death was greater than breast cancer death among women diagnosed with DCIS over 20 years. Black women had higher risks of dying from all-causes compared to white women. These differences persisted into the modern treatment era.
Similar content being viewed by others
Introduction
The incidence of ductal carcinoma in situ (DCIS) of the breast has been escalating since the 1970s [1], with DCIS representing 15–20 % of all new breast cancer diagnoses [2]. While DCIS cases have been increasing, the percentage of patients dying from breast cancer after a DCIS diagnosis has remained low. The rate of breast cancer death among DCIS patients diagnosed between 1978 and 1989 based on the National Cancer Institute’s surveillance, epidemiology, and end results (SEER) registry was 0.9 and 2.3 % at 5 and 10 years of follow-up [3]. More recent data have demonstrated a similar breast cancer mortality of 1 % over 12 years of follow-up among those treated with breast-conservation therapies [4]. While these results demonstrate favorable breast cancer outcomes for DCIS patients, there is increasing concern that women after a DCIS diagnosis are at competing risk for cardiovascular disease (CVD) mortality. Ernster et al. found that among women diagnosed with DCIS, 11 % of deaths were due to breast cancer, while 32 % were due to CVD, with the percentage of breast cancer deaths declining and the percentage of CVD deaths increasing with advancing age [3]. Similarly, Schonberg et al. determined that 7 and 27 % of deaths were due to breast cancer and CVD, respectively, among 67–79 year old women with a DCIS diagnosis [5]. However, no study to date has explored these relationships over a 20-year follow-up period and assessed CVD risk among DCIS patients in the modern treatment era (1990—present).
The etiology of higher CVD risk among women with DCIS is not well understood nor is it known whether these competing risks are race-specific. Evidence suggests that racial differences in breast cancer and overall mortality exist among women with DCIS. Specifically, Shairer et al. found that among women with a DCIS diagnosis, blacks had a greater probability of dying from both breast cancer and combined other causes at up to 27 years of follow-up [6]. In addition, Nasser et al. showed that survival in women with DCIS was greater in whites compared to blacks [7]. To date, however, no study has determined whether CVD mortality outcomes differ among white and black DCIS patients. Importantly, a change in CVD risk factors (e.g., weight gain, smoking cessation) [8] has been demonstrated in women after a DCIS diagnosis that may impact competing causes of death. This is one potential contributor to the increased risk of CVD death in the DCIS population, especially among black women who have a higher risk factor burden compared to whites in the general population [9–12]. Long-term follow-up of competing mortality outcomes, as well as racial differences specific to risk of CVD mortality, is needed to establish this possible link.
To this end, we utilized data reported to the population-based registries of the SEER program from 1978 to 2010 to assess rates of all-cause, breast cancer, and CVD death among women with DCIS aged 40 years and older at 1, 5, 10, and 20 years post-diagnosis. We also compared cause-specific mortality outcomes in black and white women with a DCIS diagnosis and examined changes in breast cancer and CVD death with advancing age of DCIS diagnosis. This is the first study to assess incidence of breast cancer and CVD death in both blacks and whites with a DCIS diagnosis as well as include cases diagnosed in the current treatment era (1990–2010).
Methods
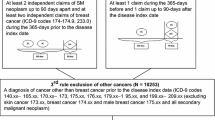
Data case listings were obtained using SEER*Stat software publically available from the National Cancer Institute [13]. We obtained case data from the 2010 SEER incidence database [14]. Included were all white and black women aged 40 years and older with newly diagnosed DCIS from 1978 to 2010 reported to SEER for the nine original registry areas. The definition of DCIS corresponds to that used in the most recent SEER reports [15]. Excluded were cases with any prior breast cancer (invasive or noninvasive) or any diagnosis of invasive breast cancer within the 2 months following the initial DCIS diagnosis. Also excluded were cases diagnosed at autopsy or identified solely on the basis of a death certificate report.
A total of 68,015 cases of histologically confirmed DCIS diagnosed between 1978 and 2010 among women aged 40 years and older and with no prior history of breast cancer were abstracted from the nine original SEER registries. Nineteen cases were excluded because they were based only on autopsy or death certificate records, leaving 67,996 cases. There were 482 women excluded due to diagnosis of invasive breast cancer within 2 months following the DCIS diagnosis. After all exclusions, a total of 67,514 DCIS cases were available for analysis.
Cause of death information was obtained from the SEER registry. We defined CVD death as any of the following causes of death as coded in the SEER database [International Classification of Diseases, Tenth Revision (ICD-10) codes]: diseases of heart (I00–I09, I11, I13, I20–I51), cerebrovascular diseases (I60–I69), atherosclerosis (I70), and other diseases of arteries, arterioles, capillaries (I72–I78).
We used the Kaplan–Meier product-limit method to determine survival rates at 1, 5, 10, and 20 years post-DCIS diagnosis. Estimates for the cumulative incidence of breast cancer death and CVD death were obtained using methods for competing-risks analysis. We computed hazard ratios and 95 % confidence intervals based on the log-rank test statistic and its variance.
Results
Of the 67,514 women included in the analysis, 54,518 were white, 6,117 were black, 6,487 were other races, and 401 were of unknown race. Distribution of DCIS cases by age at diagnosis and subsequent deaths due to breast cancer, CVD, and other causes are shown in Table 1. A total of 12,173 deaths were observed over 607,287 person-years of follow-up. The median follow-up time was 9.2 years. The percentage of deaths attributed to breast cancer and CVD were 8 and 33 %, respectively. Among women aged 40–49 years at diagnosis, the percentage of deaths attributed to breast cancer (27 %) was greater than that of CVD (12 %); however, CVD was the more prominent cause of death for all other age groups (Fig. 1).
The cumulative incidence of death at 1, 5, 10, and 20 years following DCIS diagnosis according to year of diagnosis is shown in Table 2. The 20-year cumulative incidence of all-cause death was 39.6 % (CI 38.9–40.3); this percentage was highest between 1978 and 1983 (47.9 %, CI 45.3–50.4) and lowest between 1990 and 2010 (38.8 %, CI 37.6–39.9). The corresponding overall 20-year cumulative incidence rates for breast cancer death and CVD death were 3.2 % (CI 3.0–3.4) and 13.2 % (CI 12.8–13.7), respectively. We next evaluated the cumulative incidence of death at each time point according to age of DCIS diagnosis (Table 3). The 20-year cumulative incidence of all-cause death was 9.9 % (CI 9.0–10.8) among women diagnosed at age 40–49 and increased to 83.4 % (CI 82.1–84.6) among women diagnosed at age ≥70. The corresponding 20-year cumulative incidence rates among women 40–49 and ≥70 years of age were 2.6 % (CI 2.2–3.0) and 4.2 % (CI 3.7–4.7) for breast cancer death and 1.4 % (CI 1.0–1.8) and 13.2 % (CI 12.8–13.7) for CVD death, respectively.
We next determined whether the risk of all-cause death, breast cancer death, and CVD death differed between black and white women with DCIS. Combining all years of diagnosis, black women had a higher risk of all-cause mortality compared to white women; this disparity tended to decrease with increased age at diagnosis (Fig. 2; Supplemental Table 1a). Specifically, the hazard ratio comparing black women to white women aged 40–49 years at diagnosis was 2.71 (CI 2.06–3.57), while among those aged ≥70 years at diagnosis the corresponding hazard ratio was 1.14 (CI 1.05–1.25). In the most recent diagnosis period (1990–2010), the hazard ratios of all-cause mortality comparing black women to white women were 2.74 (CI 1.96–3.82), 3.06 (CI 2.39–3.91), 1.81 (CI 1.54–2.14), and 1.22 (CI 1.10–1.35) for age-at-diagnosis groups of 40–49, 50–59, 60–69, and ≥70 years, respectively. Supplemental Table 1a demonstrates that the racial disparity persisted, and in some cases increased, over time.
Hazard ratios for breast cancer death comparing black women and white women in the DCIS cohort are shown in Fig. 2 and Supplemental Table 1b. The small numbers of breast cancer deaths among black women diagnosed prior to 1990 limited our ability to compare trends over time. However, in the most recent diagnosis period (1990–2010), the risk of breast cancer death among black women with a DCIS diagnosis was higher than that of white women, with the hazard ratios tending to decrease with increasing age at diagnosis. Among women diagnosed in 1990–2010, the hazard ratios (comparing black vs. white women) were 5.11 (CI 2.83–9.23), 5.78 (CI 3.16–10.57), 2.24 (CI 1.29–3.89), and 1.56 (CI 1.03–2.36) for women of ages 40–49, 50–59, 60–69, and ≥70 years, respectively.
For CVD death, there was also evidence of increased risk for black women with DCIS as compared to white women (Fig. 2; Supplemental Table 1c). In the most recent diagnosis period (1990–2010), the hazard ratios of CVD death in black women compared to white women with DCIS at ages 40–49, 50–59, 60–69, and ≥70 years were 14.99 (CI 5.39–41.67), 6.43 (CI 3.61–11.46), 2.26 (CI 1.63–3.14), and 1.17 (CI 0.99–1.38), respectively.
Discussion
In the current study, we found that women with DCIS were more likely to die of all-causes or CVD than breast cancer, with the proportion of women dying from CVD highest among women diagnosed at older ages. Black women with DCIS had a higher risk of dying from all-causes, breast cancer, and CVD compared to white women, with this risk persisting into the current treatment era (1990–2010). As women aged, this racial disparity decreased.
Among women with DCIS, there was a greater incidence of CVD death than breast cancer death, and this was most pronounced in women diagnosed with DCIS at age 70 years or greater. Specifically, 40 % of deaths in this group were due to CVD, and 5 % were due to breast cancer. This is consistent with U.S. mortality data, which shows an increasing prevalence of CVD death as women age [16], with the current study expanding these trends to women with DCIS. The higher incidence of CVD mortality may be due to a greater burden of behavioral risk factors [9, 17, 18] and comorbidities complicating or limiting treatment in women with DCIS, especially among older women [19, 20]. Importantly, as women with DCIS are aggressively screened and treated with surgery and adjuvant therapy [21], the risk of disease progression and thus breast cancer mortality is minimized. However, certain treatments associated with DCIS have the potential to cause cardiotoxicity, thus increasing the risk of CVD death. Specifically, 64 % of DCIS patients undergo surgical treatment and among those 52 % received radiation therapy after surgery, [22] with radiation therapy known to be associated with several cardiotoxic effects [23–25]. Interestingly, our results show higher CVD mortality among women diagnosed with DCIS between 1978 and 1983, when radiation doses were higher and cardiac sparing techniques were less frequent [26, 27]. In addition to the increased risk of CVD posed by the cardiotoxic effects of DCIS treatment, women after a DCIS diagnosis are likely to gain weight [8], thus adding a behavioral component to their increased risk of CVD mortality [28]. Taken together, these factors suggest that, while it is important to manage the possibility of DCIS progressing to more advanced breast cancer, focus must also be placed on optimizing CVD risk factor modification, especially as women with DCIS get older and further from diagnosis.
Racial differences in mortality outcomes among DCIS patients were found in all age groups with black women having a higher risk of CVD death than white women even at 20 years of follow-up. Importantly, these disparities showed no sign of decreasing over time with the greatest excess risk for black women in the most recent diagnosis period of 1990–2010. Possible explanations for the higher CVD mortality risk among blacks include disparities in screening, health care quality and access, and risk factor burden. Regular screening and health visits are key in early diagnosis of risk factors that could lead to CVD progression [29] with white women more likely than blacks to have a continuous, usual source of care [30] and to obtain earlier diagnoses for CVD [31]. Moreover, racial disparities persist after a CVD diagnosis with whites more likely than blacks to be treated with invasive procedures even after adjusting for disease severity [32]. In addition to differences in disease treatment, blacks are also less likely to be educated and treated for risk factors such as hypertension, hypercholesterolemia, and diabetes [33]. Behavioral risk factor burden is another potential contributor to racial disparities in CVD mortality with several studies showing that blacks have a greater prevalence of behavioral risk factors including physical inactivity, smoking, and obesity [10–12]. Finally, socioeconomic status, by impacting access to care and as well as access to recreational facility sites and healthy food options [34, 35], may exacerbate the risk factor burden in blacks, and thus further contribute to racial disparities in CVD mortality.
While racial differences in mortality among women with DCIS were found across all age categories, these disparities decreased with increasing age category. This is consistent with previous data from Mensah et al. that demonstrated reduced racial disparities in CVD death among older women [36]. Notably, age itself is a risk factor for both CVD [37] and breast cancer mortality [38]. Other factors, including treatment disparities and risk factor prevalence also act to elevate the risk of CVD mortality in older patients. Notably, treatment disparities among older (≥80 years) patients with coronary artery disease or congestive heart failure have been found, with treatments under prescribed in this population due to age alone [39]. Additionally, CVD and cancer risk factor burden increase with increasing age [9], as time spent in physical activity declines [17], weight gain occurs [18], and comorbidities develop [40]. Taken together, in older age, racial disparities in mortality may be diminished by these collective age-related factors exerting a greater influence on mortality risk.
Factors responsible for racial disparities in CVD death among DCIS patients may similarly contribute to the increased risk of breast cancer mortality among black women. There has been a marked increase in detected cases of DCIS since the early 1980s due to the increased use of screening mammography [41]. Despite the overall increase in breast cancer screening, black women are more likely than white women to receive inadequate mammographic screening, including underuse and reduced frequency [42]. This could lead to delayed diagnosis or undetected disease progression, and thus higher risks of breast cancer mortality among blacks. Equalizing mammographic screening use and frequency is particularly important given recent findings that breast cancer tumors in blacks grow faster and have a higher likelihood of metastasizing earlier than breast tumors in whites [43]. Similar to CVD treatment, racial differences in breast cancer treatment exist as well with a recent analysis utilizing the SEER registries finding that black women were less likely to receive radiation therapy after surgery than white women, despite the positive outcome associated with this treatment course [44]. Taken together, these factors as well as other potential unknown contributors may explain the racial disparities demonstrated in this study.
There are several limitations of this study that should be noted. We cannot exclude the possibility for misclassification of DCIS diagnosis. While the degree of misclassification is unknown, it is likely small, as the SEER registries are recognized nationally as a definitive source of U.S. cancer data. Additionally, not all DCIS cases reported to SEER contain information on tumor size and histological type or treatment, factors that could affect survival but were not included in this analysis. A strength of this study is the large sample size which permitted analysis of age subgroups and thus broadened our understanding of competing risks of mortality in the DCIS population throughout the lifespan.
In summary, women with DCIS are more likely to die from all-causes and CVD compared to breast cancer. Additionally, racial disparities in mortality risks among DCIS patients were apparent. Black women have greater risks of all-cause, breast cancer, and CVD mortality compared to white women, with these differences persisting into the current treatment era. These results provide important information to patients and health care providers regarding the competing risk for CVD mortality among women with DCIS. This is especially important for black women who traditionally have had a higher risk factor burden, though further research is required to delineate the etiology of these racial differences.
References
Virnig BA et al (2009) Diagnosis and management of ductal carcinoma in situ (DCIS). Evid Rep Technol Assess (Full Rep) 185:1–549
Sprague B (2010) In situ breast cancer. In: Li S (ed) Breast cancer epidemiology. Springer, New York, pp 47–72
Ernster VL et al (2000) Mortality among women with ductal carcinoma in situ of the breast in the population-based surveillance, epidemiology and end results program. Arch Intern Med 160(7):953–958
Lee LA et al (2006) Breast cancer-specific mortality after invasive local recurrence in patients with ductal carcinoma-in situ of the breast. Am J Surg 192(4):416–419
Schonberg MA et al (2011) Causes of death and relative survival of older women after a breast cancer diagnosis. J Clin Oncol 29(12):1570–1577
Schairer C et al (2004) Probabilities of death from breast cancer and other causes among female breast cancer patients. J Natl Cancer Inst 96(17):1311–1321
Nassar H et al (2009) Ductal carcinoma in situ in African American versus Caucasian American women: analysis of clinicopathologic features and outcome. Cancer 115(14):3181–3188
Sprague BL et al (2010) Change in lifestyle behaviors and medication use after a diagnosis of ductal carcinoma in situ. Breast Cancer Res Treat 124(2):487–495
Sundaram AA et al (2005) Differences in the prevalence of self-reported risk factors for coronary heart disease among American women by race/ethnicity and age: behavioral risk factor surveillance system, 2001. Am J Prev Med 29(5 Suppl 1):25–30
Crespo CJ et al (2000) Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the third national health and nutrition examination survey, 1988–1994. Am J Prev Med 18(1):46–53
Escobedo LG et al (1995) Educational attainment and racial differences in cigarette smoking. J Natl Cancer Inst 87(20):1552–1553
Wang Y, Beydoun MA (2007) The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 29:6–28
Surveillance Research Program, National Cancer Institute SEER*Stat Software.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence—SEER 9 Regs Research Data, Nov 2011 Sub (1973–2010) < Katrina/Rita Population Adjustment > Linked To County attributes–Total U.S., 1969–2010 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2013, based on the November 2012 submission
Howlader N, N.A., Krapcho M, Garshell J, Neyman N, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) (2013) SEER Cancer Statistics Review 1975–2010, N.C. Institute, Editor, Bethesda, MD
Compressed Mortality File 1999–2000 on CDC WONDER Online Database (2013)
Caspersen CJ, Pereira MA, Curran KM (2000) Changes in physical activity patterns in the United States, by sex and cross-sectional age. Med Sci Sports Exerc 32(9):1601–1609
Lewis CE et al (2000) Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary artery risk development in young adults. Am J Epidemiol 151(12):1172–1181
Boyd CM et al (2005) Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA 294(6):716–724
Turner BJ et al (2008) Effect of unrelated comorbid conditions on hypertension management. Ann Intern Med 148(8):578–586
Virnig BA et al (2010) Ductal carcinoma in situ of the breast: a systematic review of incidence, treatment, and outcomes. J Natl Cancer Inst 102(3):170–178
Baxter NN et al (2004) Trends in the treatment of ductal carcinoma in situ of the breast. J Natl Cancer Inst 96(6):443–448
Brosius III FC, Waller BF, Roberts WC (1981) Radiation heart disease. Analysis of 16 young (aged 15 to 33 years) necropsy patients who received over 3,500 rads to the heart. Am J Med 70(3):519–530
Orzan F et al (1993) Severe coronary artery disease after radiation therapy of the chest and mediastinum: clinical presentation and treatment. Br Heart J 69(6):496–500
Cheng SW et al (2000) Carotid stenosis after radiotherapy for nasopharyngeal carcinoma. Arch Otolaryngol Head Neck Surg 126(4):517–521
Darby SC et al (2005) Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol 6(8):557–565
Darby S et al (2003) Mortality from cardiovascular disease more than 10 years after radiotherapy for breast cancer: nationwide cohort study of 90,000 Swedish women. BMJ 326(7383):256–257
Poirier P et al (2006) Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American heart association scientific statement on obesity and heart disease from the obesity committee of the council on nutrition, physical activity, and metabolism. Circulation 113(6):898–918
American Heart A (2013) Heart-health screening. http://www.heart.org/HEARTORG/Conditions/Heart-Health-Screenings_UCM_428687_Article.jsp. Accessed 16 April 2014
Williams DR (2002) Racial/ethnic variations in women’s health: the social embeddedness of health. Am J Pub Health 92(4):588–597
Winkleby MA et al (1998) Ethnic and socioeconomic differences in cardiovascular disease risk factors: findings for women from the third national health and nutrition examination survey, 1988–1994. JAMA 280(4):356–362
Kressin NR, Petersen LA (2001) Racial differences in the use of invasive cardiovascular procedures: review of the literature and prescription for future research. Ann Intern Med 135(5):352–366
Finkelstein EA et al (2004) Racial/ethnic disparities in coronary heart disease risk factors among WISEWOMAN enrollees. J Womens Health (Larchmt) 13(5):503–518
Cheadle A et al (1991) Community-level comparisons between the grocery store environment and individual dietary practices. Prev Med 20(2):250–261
Williams DR, Collins C (2001) Racial residential segregation: a fundamental cause of racial disparities in health. Pub Health Rep 116(5):404–416
Mensah GA et al (2005) State of disparities in cardiovascular health in the United States. Circulation 111(10):1233–1241
National Institutes for Health, National Heart, Lung, and Blood Institute (2012) Morbidity and mortality: chart book on cardiovascular, lung, and blood diseases. http://www.nhlbi.nih.gov/files/docs/research/2012_ChartBook.pdf. Accessed 31 Jan 2014
Chu KC et al (1996) Recent trends in U.S. breast cancer incidence, survival, and mortality rates. J Natl Cancer Inst 88(21):1571–1579
Moubarak G et al (2013) Impact of comorbidity on medication use in elderly patients with cardiovascular diseases: the OCTOCARDIO study. Eur J Prev Cardiol 20(4):524–530
de SSMV et al (2013) Aging, obesity, and multimorbidity in women 50 years or older: a population-based study. Menopause 20(8):818–824
Ernster VL, Barclay J (1997) Increases in ductal carcinoma in situ (DCIS) of the breast in relation to mammography: a dilemma. J Natl Cancer Inst Monogr 22:151–156
Smith-Bindman R et al (2006) Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Ann Intern Med 144(8):541–553
Batina NG et al (2013) Variation in tumor natural history contributes to racial disparities in breast cancer stage at diagnosis. Breast Cancer Res Treat 138(2):519–528
Joslyn SA (2006) Ductal carcinoma in situ: trends in geographic, temporal, and demographic patterns of care and survival. Breast J 12(1):20–27
Acknowledgments
This research was supported in part by a Grant from Vermont Center on Behavior and Health. NIH, NIGMS Award # 1P20GM103644-01A1, PROSPR: NIH NCI U54 CA 163303.
Conflicts of interest
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Berkman, A., F. Cole, B., Ades, P.A. et al. Racial differences in breast cancer, cardiovascular disease, and all-cause mortality among women with ductal carcinoma in situ of the breast. Breast Cancer Res Treat 148, 407–413 (2014). https://doi.org/10.1007/s10549-014-3168-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-3168-3