Abstract
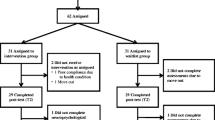
The purpose of this study was to evaluate the preliminary efficacy and satisfaction/acceptability of training in memory or speed of processing versus wait-list control for improving cognitive function in breast cancer survivors. 82 breast cancer survivors completed a three-group randomized, controlled trial. Primary outcomes were objective neuropsychological tests of memory and speed of processing. Secondary outcomes were perceived cognitive functioning, symptom distress (mood disturbance, anxiety, and fatigue), quality of life, and intervention satisfaction/acceptability. Data were collected at baseline, post-intervention, and 2-month follow-up. Using repeated-measures mixed-linear ANCOVA models, each intervention was compared to wait-list control while adjusting for age, education, and baseline measures. The effect sizes for differences in means and the reliable improvement percentage were reported. The results show that domain-specific effects were seen for both interventions: memory training improved memory performance at 2-month follow-up (p = 0.036, d = 0.59); speed of processing training improved processing speed post-intervention (p = 0.040, d = 0.55) and 2-month follow-up (p = 0.016; d = 0.67). Transfer effects to non-trained domains were seen for speed of processing training with improved memory post-intervention (p = 0.007, d = 0.75) and 2-month follow-up (p = 0.004, d = 0.82). Both interventions were associated with improvements in perceived cognitive functioning, symptom distress, and quality of life. Ratings of satisfaction/acceptability were high for both interventions. It was concluded that while both interventions appeared promising, speed of processing training resulted in immediate and durable improvements in objective measures of processing speed and verbal memory. Speed of processing training may have broader benefits in this clinical population.



Similar content being viewed by others
References
Hess LM, Insel KC (2007) Chemotherapy-related change in cognitive function: a conceptual model. Oncol Nurs Forum 34(5):981–994
Jansen CE, Miaskowski C, Dodd M, Dowling G, Kramer J (2005) A metaanalysis of studies of the effects of cancer chemotherapy on various domains of cognitive function. Cancer 104(10):2222–2233
Stewart A, Bielajew C, Collins B, Parkinson M, Tomiak E (2006) A meta-analysis of the neuropsychological effects of adjuvant chemotherapy treatment in women treated for breast cancer. Clin Neuropsychol 20(1):76–89
Falleti MG, Sanfilippo A, Maruff P, Weih L, Phillips KA (2005) The nature and severity of cognitive impairment associated with adjuvant chemotherapy in women with breast cancer: a meta-analysis of the current literature. Brain Cogn 59(1):60–70
Anderson-hanley C, Sherman M, Riggs R, Agocha V, Compas B (2003) Neuropsychological effects of treatments for adults with cancer: a meta-analysis and review of the literature. J Int Neuropsychol Soc 9(7):967–982
Von Ah D, Russell KM, Storniolo AM, Carpenter JS (2009) Cognitive dysfunction and its relationship to quality of life in breast cancer survivors. Oncol Nurs Forum 36(3):326–336
Mehnert A, Scherwath A, Schirmer L, Schleimer B, Petersen C, Schultz-Kindermann F, Zander AR, Koch U (2007) The association between neuropsychological impairment, self-perceived cognitive deficits, fatigue, and quality of life in breast cancer survivors following standard adjuvant versus high-dose chemotherapy. Patient Educ Couns 66(1):108–118
Von Ah D, Jansen C, Allen DH, Schiavone RM, Wulff J (2011) Putting evidence into practice: evidence-based interventions for cancer and cancer treatment-related cognitive impairment. Clin J Oncol Nurs 15(6):607–615
Fardell JE, Vardy J, Johnston IN, Winocur G (2011) Chemotherapy and cognitive impairment: treatment options. Clin Pharmacol Ther 90(3):366–376
Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, Marsiske M, Morris JN, Rebok GW, Smith DM, Tennstedt SL et al (2002) Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA 288(18):2271–2281
Willis SL, Tennstedt SL, Marsiske M, Ball K, Elias J, Koepke KM, Morris JN, Rebok GW, Unverzagt FW, Stoddard AM et al (2006) Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA 296(23):2805–2814
Smith GE, Housen P, Yaffe K, Ruff R, Kennison RF, Mahncke HW, Zelinski EM (2009) A cognitive training program based on principles of brain plasticity: results from the Improvement in Memory with Plasticity-based Adaptive Cognitive Training (IMPACT) study. J Am Geriatr Soc 57(4):594–603
Zelinski EM, Spina LM, Yaffe K, Ruff R, Kennison RF, Mahncke HW, Smith GE (2011) Improvement in memory with plasticity-based adaptive cognitive training: results of the 3-month follow-up. J Am Geriatr Soc 59(2):258–265
Ferguson RJ, McDonald BC, Rocque MA, Furstenberg CT, Horrigan S, Ahles TA, Saykin AJ (2012) Development of CBT for chemotherapy-related cognitive change: results of a waitlist control trial. Psychooncology 21(2):176–186
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Jobe JB, Smith DM, Ball K, Tennstedt SL, Marsiske M, Willis SL, Rebok GW, Morris JN, Helmers KF, Leveck MD et al (2001) Active: a cognitive intervention trial to promote independence in older adults. Control Clin Trials 22(4):453–479
Mahncke HW, Conner BB, Appelman J, Ahsanuddin ON, Hardy JL, Wood RA, Joyce NM, Boniske T, Atkins SM, Merzenich MM (2006) Memory enhancement in healthy older adults using a brain plasticity-based training program: a randomized, controlled study. Proc Natl Acad Sci USA 103(33):12523–12538
Rey A (1941) L’examen psychologique dans les cas d’encephalopathie traumatique. Archives de Psychologie 28:286–340
Wilson B, Cockburn J, Baddeley A (1985) The rivermead behavioral memory test. Thames Valley Test Co., Reading and National Rehabilitation Services, Gaylord
Owsley C, Ball K, McGwin G Jr, Sloane ME, Roenker DE, White MF, Overley ET (1998) Visual processing impairment and risk of motor vehicle crash among older adults. JAMA 279(14):1083–1088
Ball K, Owsley C (1993) The useful field of view test: a new technique for evaluating age-related declines in visual function. J Am Optom Assoc 64:71–79
Edwards JD, Ross LA, Wadley VG, Clay OJ, Crowe M, Roenker DL, Ball KK (2006) The useful field of view test: normative data for older adults. Arch Clin Neuropsychol 21(4):275–286
Jacobs SR, Jacobsen PB, Booth-Jones M, Wagner LI, Anasetti C (2007) Evaluation of the functional assessment of cancer therapy cognitive scale with hematopoietic stem cell transplant patients. J Pain Symptom Manage 33(1):13–23
Squire LR, Wetzel CD, Slater PC (1979) Memory complaint after electroconvulsive therapy: assessment with a new self-rating instrument. Biol Psychiatry 14:791–801
Spielberger CD, Gorsuch RI, Lushene RG (1971) Manual for the state-trait anxiety inventory. Consulting Press, Palo Alto
Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E (1997) Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage 13(2):63–74
Ferrell BR, Dow KH, Leigh S, Ly J, Gulasekaram P (1995) Quality of life in long-term cancer survivors. Oncol Nurs Forum 22(6):915–922
Ferrans CE, Powers MJ (1985) Quality of life index: development and psychometric properties. ANS Adv Nurs Sci 8(1):15–24
Ware JE Jr, Snow KK, Kosinski M, Gandek B (1993) SF-36 health survey manual and interpretation guide. The Health Institute, The New England Medical Center, Boston
Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD (1979) Assessment of client/patient satisfaction: development of a general scale. Eval Program Plan 2(3):197–207
Carpenter JS, Neal JG, Payne J, Kimmick G, Storniolo AM (2007) Cognitive-behavioral intervention for hot flashes. Oncol Nurs Forum 34(1):E1–E8
Blom G (1958) Statistical estimates and transformed beta variables. Wiley, New York
Dudek FJ (1979) The continuing misinterpretation of the standard error of measurement. Psychol Bull 86(2):335–337
Uchiyama CL, D’Elia LF, Dellinger AM, Becker JT, Seines DA, Wescln JE, Chen BB, Satz P, van Gorp WG, Miller EN (1995) Alternate forms of the auditory-verbal learning test: issues of test comparability, longitudinal reliability and moderating demographic variables. Arch Clin Neuropsychol 10(2):133–145
Von Ah D, Harvison K, Monahan P, Moser L, Zhao Q, Carpenter J, Sledge G Jr, Champion V, Unverzagt F (2009) Cognitive function in breast cancer survivors compared to healthy age- and education-matched women. Clin Neuropsychol 23(4):661–674
Valenzuela M, Sachdev P (2009) Can cognitive exercise prevent the onset of dementia? Systematic review of randomized clinical trials with longitudinal follow-up. Am J Geriatr Psychiatry 17(3):179–187
Boykoff N, Moieni M, Subramanian SK (2009) Confronting chemobrain: an in-depth look at survivors’ reports of impact on work, social networks, and health care response. J Cancer Surviv 3(4):223–232
Calvio L, Peugeot M, Bruns GL, Todd BL, Feuerstein M (2010) Measures of cognitive function and work in occupationally active breast cancer survivors. J Occup Environ Med 52(2):219–227
Munir F, Burrows J, Yarker J, Kalawsky K, Bains M (2010) Women’s perceptions of chemotherapy-induced cognitive side affects on work ability: a focus group. J Clin Nurs 19(9–10):1362–1370
Acknowledgments
This study was supported by Robert Wood Johnson Foundation Nurse Faculty Scholar Program (#64194), American Cancer Society Institutional Research Grant (#84-002-25), Indiana University School of Nursing Center for Enhancing Quality of Life in Chronic Illness and the Mary Margaret Walther Program of the Walther Cancer Institute (#0097.01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Robert Wood Johnson Foundation, which funded this trial. The funding agency had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. Dr. Patrick Monahan had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
The authors declare that they have no conflict of interest. Posit Science Corporation is the developer of the speed of processing (Insight®) program used in this study. Posit Science Corporation holds the patent for and a proprietary interest in this software. The software was provided at cost of the CD by Posit Science. Dr. Karlene Ball is on the Board of Directors of Posit Science and has stock in the company. Dr. Unverzagt has received support for training for an investigator initiated research from Posit Science.
Ethical approval
This study was conducted in accordance with all laws of the United States and the study was approved by the Indiana University Simon Cancer Center Scientific Review Group and Institutional Review Board in which was conducted.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Von Ah, D., Carpenter, J.S., Saykin, A. et al. Advanced cognitive training for breast cancer survivors: a randomized controlled trial. Breast Cancer Res Treat 135, 799–809 (2012). https://doi.org/10.1007/s10549-012-2210-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2210-6