Abstract
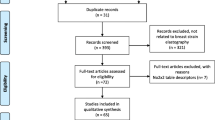
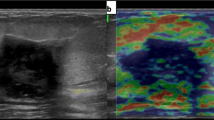
The purpose of this study was to systematically review recent literature on diagnostic performance of strain ratio and length ratio, two different strain measurements in ultrasound elastography, for differentiating benign and malignant breast masses. A literature search of PubMed and other medical and general purpose databases from inception through January 2012 was conducted. Published studies that evaluated the diagnostic performance of ultrasound elastography alone reporting either strain ratio or length ratio for characterization of focal breast lesions and using cytology (fine needle aspiration) or histology (core biopsy) as a reference standard were included. Summary diagnostic performance measures were assessed using bivariate generalized linear mixed modeling. Nine studies reported strain ratio for 2,087 breast masses (667 cancers, 1,420 benign lesions). Summary sensitivity and specificity were 88 % (95 % Credible Interval (CrI), 84–91 %), and 83 % (95 % CrI, 78–88 %), respectively. The positive and negative likelihood ratios (LR) were 5.57 (95 % CrI, 3.85–8.01) and 0.14 (95 % CrI, 0.09–0.20), respectively. The inconsistency index for heterogeneity was 6 % (95 % CrI, 1–22 %) for sensitivity and 8 % (95 % CrI, 3–24 %) for specificity. Analysis of three studies reporting length ratio for 450 breast masses demonstrated sensitivity and specificity of 98 % (95 % CrI, 93–99 %) and 72 % (95 % CrI, 31–96 %), respectively. Strain ratio and length ratio have good diagnostic performance for distinguishing benign from malignant breast masses. Although, this performance may not be incrementally superior to that of breast imaging reporting and data system (BIRADS) in B-mode ultrasound, the application of USE using strain ratio or length ratio in combination with USB may have the potential to benefit the patients, and this requires further comparative effectiveness and cost-effectiveness analyses.






Similar content being viewed by others
Abbreviations
- USB:
-
B-mode ultrasound
- USE:
-
Breast ultrasound elastography
- BIRADS:
-
Breast imaging reporting and data system
- CrI:
-
Credible interval
- FN:
-
False negatives
- FP:
-
False positives
- I 2 :
-
Inconsistency index
- LR:
-
Likelihood ratios
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- QUADAS:
-
Quality Assessment of Diagnostic Accuracy Studies
- STARD:
-
Standards for Reporting of Diagnostic Accuracy checklist
- SROC:
-
Summary receiver operating characteristic
- TN:
-
True negatives
- TP:
-
True positives
References
Hatzung G, Grunwald S, Zygmunt M et al (2010) Sonoelastography in the diagnosis of malignant and benign breast lesions: initial clinical experiences. Ultraschall Med 31:596–603
Garra BS (2007) Imaging and estimation of tissue elasticity by ultrasound. Ultrasound Q 23:255–268
Wells PN, Liang HD (2011) Medical ultrasound: imaging of soft tissue strain and elasticity. J R Soc Interface 8:1521–1549
Regini E, Bagnera S, Tota D et al (2010) Role of sonoelastography in characterising breast nodules. Preliminary experience with 120 lesions. Radiol Med 115:551–562
Itoh A, Ueno E, Tohno E et al (2006) Breast disease: clinical application of US elastography for diagnosis. Radiology 239:341–350
Chang JM, Moon WK, Cho N, Kim SJ (2011) Breast mass evaluation: factors influencing the quality of US elastography. Radiology 259:59–64
Thomas A, Degenhardt F, Farrokh A et al (2010) Significant differentiation of focal breast lesions: calculation of strain ratio in breast sonoelastography. Acad Radiol 17:558–563
Fischer T, Peisker U, Fiedor S et al (2011) Significant differentiation of focal breast lesions: raw data-based calculation of strain ratio. Ultraschall Med. doi:10.1055/s-0031-1273222
Leong LC, Sim LS, Lee YS et al (2010) A prospective study to compare the diagnostic performance of breast elastography versus conventional breast ultrasound. Clin Radiol 65:887–894
Sadigh G, Carlos RC, Neal CH, Dwamena BA (2011) Ultrasonographic differentiation of malignant from benign breast lesions: a meta-analytic comparison of elasticity and BIRADS scoring. Breast Cancer Res Treat. doi:10.1007/s10549-011-1857-8
Yerli H, Yilmaz T, Kaskati T, Gulay H (2011) Qualitative and semiquantitative evaluations of solid breast lesions by sonoelastography. J Ultrasound Med 30:179–186
Lee JH, Kim SH, Kang BJ et al (2011) Role and clinical usefulness of elastography in small breast masses. Acad Radiol 18:74–80
Barr RG (2010) Real-time ultrasound elasticity of the breast: initial clinical results. Ultrasound Q 26:61–66
Kumm TR, Szabunio MM (2010) Elastography for the characterization of breast lesions: initial clinical experience. Cancer Control 17:156–161
Zhi H, Xiao XY, Yang HY et al (2010) Ultrasonic elastography in breast cancer diagnosis: strain ratio vs 5-point scale. Acad Radiol 17:1227–1233
Cho N, Moon WK, Kim HY et al (2010) Sonoelastographic strain index for differentiation of benign and malignant nonpalpable breast masses. J Ultrasound Med 29:1–7
Farrokh A, Wojcinski S, Degenhardt F (2010) Diagnostic value of strain ratio measurement in the differentiation of malignant and benign breast lesions. Ultraschall Med 32:400–405
Moon WK, Huang CS, Shen WC et al (2009) Analysis of elastographic and B-mode features at sonoelastography for breast tumor classification. Ultrasound Med Biol 35:1794–1802
Regner DM, Hesley GK, Hangiandreou NJ et al (2006) Breast lesions: evaluation with US strain imaging—clinical experience of multiple observers. Radiology 238:425–437
Cochrane Diagnostic Test Accuracy Review Working Group. http://srdta.cochrane.org/handbook-dta-reviews. Accessed 15 Aug 2011
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(264–269):W264
Landoni V, Francione V, Marzi S et al (2011) Quantitative analysis of elastography images in the detection of breast cancer. Eur J Radiol. doi:10.1016/j.ejrad.2011.04.012
Whiting P, Rutjes AW, Reitsma JB et al (2003) The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 3:25
Chu H, Cole SR (2006) Bivariate meta-analysis of sensitivity and specificity with sparse data: a generalized linear mixed model approach. J Clin Epidemiol 59:1331–1332 author reply 1332-1333
Arends LR, Hamza TH, van Houwelingen JC et al (2008) Bivariate random effects meta-analysis of ROC curves. Med Decis Making 28:621–638
Macaskill P, Gatsonis C, Deeks JJ, Harbord RM, Takwoingi Y (2010) Chapter 10: Analysing and presenting results. In: Deeks JJ, Bossuyt PM, Gatsonis C (eds) Cochrane handbook for systematic reviews of diagnostic test accuracy version 1.0. The Cochrane Collaboration. http://srdta.cochrane.org/
Gatsonis C, Paliwal P (2006) Meta-analysis of diagnostic and screening test accuracy evaluations: methodologic primer. AJR Am J Roentgenol 187:271–281
Chappell FM, Raab GM, Wardlaw JM (2009) When are summary ROC curves appropriate for diagnostic meta-analyses? Stat Med 28:2653–2668
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58:882–893
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Dwamena BA (2007) MIDAS: Stata module for meta-analytical integration of diagnostic test accuracy studies. Statistical Software Components S456880. Boston College Department of Economics, Boston. http://ideas.repec.org/c/boc/bocode/s456880.html
Ikeda K, Ogawa Y, Takii M et al (2012) A role for elastography in the diagnosis of breast lesions by measuring the maximum fat lesion ratio (max-FLR) by tissue Doppler imaging. Breast Cancer 19:71–76
Wang Z, Yang T, Wu Z et al (2010) Correlation between elastography score and strain rate ratio in breast small tumor. Zhong Nan Da Xue Xue Bao Yi Xue Ban 35:928–932
Yoon JH, Kim MH, Kim EK et al (2011) Interobserver variability of ultrasound elastography: how it affects the diagnosis of breast lesions. AJR Am J Roentgenol 196:730–736
Meng W, Zhang G, Wu C et al (2011) Preliminary results of acoustic radiation force impulse (ARFI) ultrasound imaging of breast lesions. Ultrasound Med Biol 37:1436–1443
Jones CM, Athanasiou T (2009) Diagnostic accuracy meta-analysis: review of an important tool in radiological research and decision making. Br J Radiol 82:441–446
Ament A, Hasman A (1993) Optimal test strategy in the case of two tests and one disease. Int J Biomed Comput 33:179–197
Thomas A, Kummel S, Fritzsche F et al (2006) Real-time sonoelastography performed in addition to B-mode ultrasound and mammography: improved differentiation of breast lesions? Acad Radiol 13:1496–1504
Athanasiou A, Tardivon A, Tanter M et al (2010) Breast lesions: quantitative elastography with supersonic shear imaging–preliminary results. Radiology 256:297–303
Chung SY, Moon WK, Choi JW et al (2010) Differentiation of benign from malignant nonpalpable breast masses: a comparison of computer-assisted quantification and visual assessment of lesion stiffness with the use of sonographic elastography. Acta Radiol 51:9–14
Sohn YM, Kim MJ, Kim EK et al (2009) Sonographic elastography combined with conventional sonography: how much is it helpful for diagnostic performance? J Ultrasound Med 28:413–420
Thomas A, Fischer T, Frey H et al (2006) Real-time elastography—an advanced method of ultrasound: first results in 108 patients with breast lesions. Ultrasound Obstet Gynecol 28:335–340
Raza S, Odulate A, Ong EM et al (2010) Using real-time tissue elastography for breast lesion evaluation: our initial experience. J Ultrasound Med 29:551–563
Ciurea AI, Bolboaca SD, Ciortea CA et al (2011) The influence of technical factors on sonoelastographic assessment of solid breast nodules. Ultraschall Med 32(Suppl 1):S27–S34
Bossuyt PM, Reitsma JB, Bruns DE et al (2003) Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. Radiology 226:24–28
Schuetz GM, Zacharopoulou NM, Schlattmann P, Dewey M (2010) Meta-analysis: noninvasive coronary angiography using computed tomography versus magnetic resonance imaging. Ann Intern Med 152:167–177
Conflict of interest
Ruth Carlos is a member of physician’s advisory board of Philips. Gelareh Sadigh, Colleen Neal and Ben Dwamena have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sadigh, G., Carlos, R.C., Neal, C.H. et al. Accuracy of quantitative ultrasound elastography for differentiation of malignant and benign breast abnormalities: a meta-analysis. Breast Cancer Res Treat 134, 923–931 (2012). https://doi.org/10.1007/s10549-012-2020-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2020-x