Abstract
Developing and deploying separate treatments for separate conditions seems ill-suited to intervening upon the co-occurring, and possibly functionally similar, psychosocial conditions facing gay and bisexual men. This article argues for the need to create transdiagnostic interventions that reduce multiple syndemic conditions facing gay and bisexual men at the level of their shared source in minority stress pathways. This article first reviews psychosocial syndemic conditions affecting gay and bisexual men, then suggests pathways that might link minority stress to psychosocial syndemics based on recent advancements in emotion science, psychiatric nosology, and cognitive-affective neuroscience, and finally suggests cross-cutting psychosocial treatment principles to reduce minority stress−syndemic pathways among gay and bisexual men. Because minority stress serves as a common basis of all psychosocial syndemic conditions reviewed here, locating the pathways through which minority stress generates psychosocial syndemics and employing overarching treatment principles capable of simultaneously alleviating these pathways will ultimately create a transdiagnostic approach to improving gay and bisexual men’s health. Clinical research and training approaches are suggested to further validate the pathways suggested here, establish the efficacy of treatment approaches tied to those pathways, and generate effective methods for disseminating a transdiagnostic minority stress treatment approach for gay and bisexual men’s psychosocial syndemic health.
Similar content being viewed by others
Parallel developments in two distinct fields are converging to suggest a novel approach to improving gay and bisexual men’s psychosocial health. On one hand, the public health field recognizes the inextricable nature of the multiple psychosocial health threats facing gay and bisexual communities and has adopted a syndemic perspective to explain these co-occurring health conditions (e.g., Egan et al., 2011; Mustanski, Garofalo, Herrick, & Donenberg, 2007; Parsons, Grov, & Golub, 2012; Stall, Friedman, & Catania, 2008). On the other hand, driven by a longstanding need for the psychosocial intervention field to achieve consensus around unified principles of change (Goldfried, 1980, 2013), intervention researchers are simultaneously becoming aware of the need to develop and deploy treatments that address the shared factors shown to underlie numerous psychosocial conditions (e.g., Barlow, Allen, & Choate, 2004). Thus, continuing down the separate problem-separate treatment path that has historically characterized psychosocial intervention research not only seems presently infeasible given the need to deliver effective interventions with constrained resources (Westen, Novotny, & Thompson-Brenner, 2004), but also unnecessary and potentially misguided in the case of gay and bisexual men’s health given that the numerous psychosocial health threats facing this group do not occur in isolation. This article argues for the need to create transdiagnostic interventions that simultaneously reduce multiple syndemic conditions facing gay and bisexual men at the level of their shared psychosocial pathways. Further, this article positions minority stress as a key driver of these shared pathways and suggests intervention principles and techniques that can address the pathways through which minority stress is argued to yield syndemic health threats for gay and bisexual men. This article first briefly reviews psychosocial syndemic conditions affecting gay and bisexual men, then suggests potential mechanisms that might link minority stress to psychosocial syndemics based on recent initiatives in the mental health field, and finally suggests cross-cutting psychosocial treatment principles to reduce minority stress−syndemic pathways among gay and bisexual men.
Minority Stress and Psychosocial Syndemic Conditions Affecting Gay and Bisexual Men
Gay, bisexual, and other men who have sex with men are disproportionately burdened by several psychosocial health problems compared to heterosexual men, including (1) depression and anxiety (Mays & Cochran, 2001), (2) substance use problems (Green & Feinstein, 2012), (3) intimate partner violence (Balsam, Rothblum, & Beauchaine, 2005; Tjaden, Thoennes, & Allison, 1999), (4) body image disturbance and eating disorders (Austin et al., 2004; Russell & Keel, 2002), and (5) sexual compulsivity (Baum & Fishman, 1994; Missildine, Feldstein, Punzalan, & Parsons, 2005). These psychosocial health disparities frequently co-occur (Parsons et al., 2012; Stall & Purcell, 2000) and additively confer risk for HIV risk behavior and infection (Brennan, Craig, & Thompson, 2012; Klostermann, Kelley, Milletich, & Mignone, 2011; West, 2012; Wilton, 2009). Given that these problems co-exist in a climate of social marginalization and that the presence of any one of these problems exacerbates the health-depleting impact of the others, these conditions have been described as forming a syndemic, or simultaneous and synergistic epidemic, surrounding gay and bisexual men (Stall & Purcell, 2000). Addressing syndemic factors has been argued to be an essential component of meaningful HIV prevention approaches for gay and bisexual men, expanding HIV prevention beyond modifying individual-level social cognitive factors (Halkitis, 2010).
Strong and continually growing evidence suggests that each of the psychosocial syndemic conditions noted above is associated with the disproportionate stigma-based stress, known as minority stress (Meyer, 2003), borne by sexual minority, compared to heterosexual, men. For instance, depression and anxiety are associated with minority stressors including gay-related victimization, discrimination, chronic expectations of gay-related rejection, internalized homophobia, and sexual orientation concealment (Feinstein, Goldfried, & Davila, 2012; Pachankis, Newcomb, Feinstein, & Bernstein, 2014c). Further, substance use problems are associated with chronic expectations of gay-related rejection and internalized homophobia (Brubaker, Garrett, & Dew, 2009; Green & Feinstein, 2012; Pachankis, Hatzenbuehler, & Starks, 2014b). Intimate partner violence among gay and bisexual men is associated with stigma-based rejection sensitivity for both victims and perpetrators (Carvalho, Lewis, Derlega, Winstead, & Viggiano, 2011) as well as internalized homophobia and concealment for perpetrators (Edwards & Sylaska, 2013). Body image disturbance and eating disorders are associated with gay-related rejection expectations, internalized homophobia, and sexual orientation-based victimization (Kimmel & Mahalik, 2005). Finally, sexual compulsivity is associated with retrospectively recalled boyhood gender nonconformity, perceived discrimination, internalized homophobia, and expectations of sexual orientation-based rejection (Pachankis et al., in press). These stressors, uniquely experienced by sexual minority individuals, additively combine with general life stress (Meyer, Schwartz, & Frost, 2008) to put gay and bisexual men at particular risk of experiencing psychosocial syndemic health conditions (Hamilton & Mahalik, 2009; Hatzenbuehler, Nolen-Hoeksema, & Erickson, 2008c).
Minority stress theory offers a comprehensive and parsimonious framework for describing the stressors through which the social environment ultimately produces poorer health for stigmatized minority groups compared to non-stigmatized groups. Rather than suggesting that minority stress arises from sexual minority individuals themselves or even primarily from homophobic individuals in the general population, minority stress theory recognizes the foremost role of stigmatizing social structures in driving stress-sensitive psychosocial disparities among sexual minorities (Meyer, 2003). These structures include discriminatory laws, policies, and institutions that deny sexual minorities the same rights and opportunities afforded to heterosexuals. They are hypothesized to operate through the psychosocial stressors described above to yield adverse health among sexual minorities (Hatzenbuehler, 2010). In addition to positing the context-dependent nature of minority stress, minority stress theory, like any theory of psychosocial risk, also recognizes that the ability of stress to generate psychosocial risk depends on psychological predispositions, biological background, and ongoing situations not tied to minority stress (e.g., Dohrenwend, 2000). Minority stress, then, adds to the psychosocial burden of general life stress to compromise psychosocial health among individuals who are otherwise predisposed to adverse psychosocial health through personal vulnerability factors. At the population level, minority stress in the form of gay-related victimization, discrimination, chronic expectations of gay-related rejection, internalized homophobia, and sexual orientation concealment translates stigmatizing social structures into poor health for sexual minorities.
While not previously considered in minority stress conceptualizations of sexual minority psychosocial health, the ways in which social structures shape the nature and experience of gay communities themselves might also serve as a form of minority stress, similar to the ways that social structures shape local cultures to ultimately jeopardize the health of other disadvantaged groups (e.g., Wilson, 2010). Specifically, the gay community can internalize societal stigma and perpetuate additional stress among its community members. In fact, the majority of gay and bisexual participants in one recent qualitative study noted that many of their unique stressors stem from other gay men and that these stressors affected their health (Pachankis, 2014). Examples of these community-driven stressors include conformity to masculine standards, permissive substance use norms, ready availability of sex partners, and excessive focus on achievement and competition, all of which have been shown to be associated with psychosocial syndemic health outcomes in recent studies. For example, the strict conformity to masculine norms perpetuated by some gay communities (Taywaditep, 2001) is associated with a composite of syndemic health risks, including substance use, body image disturbance, and HIV risk behaviors (Brennan et al., 2012; Courtenay, 2000; Hamilton & Mahalik, 2009; Pachankis, Westmaas, & Dougherty, 2011). Further, sexual orientation disparities in permissive substance use norms are associated with elevated rates of substance use in gay, compared to heterosexual, men (Cochran, Grella, & Mays, 2012; Hatzenbuehler, Corbin, & Fromme, 2008a). Also, the ready availability of sexual outlets in urban gay male communities has been proposed as one contributing factor to sexual compulsivity among gay men (Parsons, Kelly, Bimbi, Muench, & Morgenstern, 2007). Additionally, preliminary evidence suggests that the self-worth of some gay and bisexual men is particularly achievement-oriented and competition-focused, a focus which is associated with insalubrious eating behavior, interpersonal behavior, and mental health (Pachankis & Hatzenbuehler, 2013) and which contributes to some gay and bisexual men’s impression that the gay community is inaccessible to all of its potential members (Pachankis, 2014). Several studies support the unhealthy nature of these community-driven stressors by uncovering associations between gay and bisexual men’s degree of exposure to the gay community and syndemic conditions, such as eating disorders (Feldman & Meyer, 2007), substance use (Green & Feinstein, 2012), and HIV risk behavior (Egan et al., 2011).
Minority Stress−Syndemic Pathways
Because minority stress serves as a common basis of all psychosocial syndemic conditions reviewed here, intervention approaches that target the pathways through which minority stress produces these conditions could alleviate them all at once. Advancements in emotion science (e.g., Mineka, Watson, & Clark, 1998), psychiatric nosology (e.g., Krueger, Watson, & Barlow, 2005), and cognitive-affective neuroscience (e.g., Shin & Liberzon, 2010) suggest that symptoms of each psychosocial syndemic problem affecting gay and bisexual men might represent a functionally equivalent set of emotion-driven behaviors triggered by similar emotional or interpersonal contexts and maintained by similar operant processes. Locating the shared source of these syndemic conditions in minority stress and the pathways through which minority stress operates to deplete health could therefore yield efficient and cost-effective psychosocial interventions capable of simultaneously addressing gay and bisexual men’s multiple syndemic challenges.
In fact, shared genetic, neurological, and behavioral pathways underlie many stress-related psychosocial problems in the general population (Wilamowska et al., 2010). For example, depression and anxiety, substance use, intimate partner violence, body image concerns, and sexual compulsivity could be argued to represent final behavioral outcomes of the same or similar underlying neurological, cognitive, affective, and interpersonal stress pathways, such as limbic system over-responding and limited inhibitory cortical control, painful memories, myopic decision-making, and low self-efficacy for enacting effective behavior (Brady & Sinha, 2007; Etkin & Wager, 2007; Hains & Arnsten, 2008; Heim, Owens, Plotsky, & Nemeroff, 1997; Miyake et al., 2010). Consequently, psychosocial treatments that address these shared pathways have been shown to be effective across psychosocial problems (e.g., Ellard, Fairholme, Boisseau, Farchione, & Barlow 2010; Farchione et al., 2012). These advancements and the growing demand for efficacious treatments in economically constrained contexts suggest that the most valid and efficient future approach will be to create transdiagnostic interventions that draw upon cross-cutting principles and intervention techniques that intervene upon the shared pathways of overlapping, functionally equivalent symptoms.
Recent efforts in psychiatric nosology (Insel et al., 2010; Sanislow et al., 2010) provide a framework for locating the shared pathways that link minority stress with psychosocial syndemic conditions. In particular, the National Institute of Mental Health Strategic Plan (NIMH, 2008a, b) has launched an effort to improve the accurate classification and treatment of psychosocial conditions by locating the core mechanisms unifying them. The resulting framework, the Research Domain Criteria (RDoC), lists the component mechanisms underlying multiple psychosocial conditions, recognizing that there is not an exclusive one-to-one correspondence between psychosocial conditions and their pathways (Insel et al., 2010; Sanislow et al., 2010). Currently, a work-in-progress and only intended to guide the description of psychosocial problems in research studies, the RDoC is not presently intended to serve as a clinical tool (Sanislow et al., 2010). However, the RDoC’s comprehensive list of cross-cutting mechanisms can potentially spur a more focused, efficient search for those mechanisms underlying gay and bisexual men’s psychosocial syndemic conditions with the goal of developing transdiagnostic and efficient psychosocial treatments for this population.
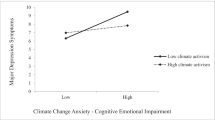
Several RDoC mechanisms might specifically operate as pathways through which minority stress generates gay and bisexual men’s psychosocial syndemic conditions in that they demonstrate associations with both minority stress and syndemic conditions, as depicted in Fig. 1, thereby meeting one necessary, although insufficient, precondition of statistical mediation (MacKinnon, 2008). Specific RDoC mechanisms possessing preliminary promise as minority stress–syndemic pathways include disruptions of negative valence systems (i.e., avoidance, hypervigilance, loss), positive valence systems (i.e., approach motivation, reward learning, habit), and social functioning (i.e., disrupted attachment, low agency, social submission, poor social communication, low self-knowledge). Preliminary evidence for these RDoC domains operating as minority stress–syndemic pathways is reviewed below with the goal of encouraging future research into the validity of these pathways and their potential to be modified by psychosocial treatment approaches that simultaneously address the multiple psychosocial conditions affecting gay and bisexual men.
Possible Negative Valence Pathways: Avoidance, Hypervigilance, and Loss
Negative valence pathways outlined in the RDoC that possess associations with both minority stress and gay and bisexual men’s psychosocial syndemics include responses to acute threat (avoidance), responses to potential harm (hypervigilance), and loss.
As noted above, gay and bisexual men are disproportionately exposed to multiple types of victimization, violence, and abuse across the lifespan, including childhood sexual abuse, peer assault, parental physical abuse, and parental rejection, compared to heterosexual men (Balsam et al., 2005; Friedman, Marshal, Stall, Cheong, & Wright, 2008; Russell, Ryan, Toomey, Diaz, & Sanchez, 2011). These acute stressors have been shown to exacerbate fear responding across the lifespan (Bremner et al., 2005; Teicher et al., 2003), including emotional, cognitive, and behavioral forms of avoidance (Foa & Kozak, 1986; Marx & Sloan, 2002). Avoidance might manifest in emotional numbing through substance abuse, compulsive or risky sexual behavior, or other forms of impulsive behavior enacted to escape painful affective experiences (Batten, Follette, & Aban, 2002; Gratz, Bornovalova, Delany-Brumsey, Nick, & Lejuez, 2007; Paul, Catania, Pollack, & Stall, 2001). Cognitive avoidance, such as rumination or worry (Fresco, Frankel, Mennin, Turk, & Heimberg, 2002), represents another avoidance strategy emerging from early and ongoing stress of the type disproportionately faced by gay and bisexual men (Hatzenbuehler, McLaughlin, & Nolen-Hoeksema, 2008b) and has been shown to mediate the relationship between minority stress experiences, such as discrimination, and depressed and anxious mood among sexual minority individuals (Hatzenbuehler, Nolen-Hoeksema, & Dovidio, 2009). Further, cognitive avoidance through mental disengagement, including fatalistic beliefs about HIV infection, has been shown to mediate the association between internalized homophobia and condomless sex (Yi, Sandfort, & Shidlo, 2010). Behavioral forms of avoidance, such as unassertive interpersonal behavior, have been shown to be closely associated with minority stress, such as parental rejection of one’s sexual orientation (Pachankis, Goldfried, & Ramrattan, 2008) and to be associated with HIV risk behavior in the form of condom use non-assertion (Hart & Heimberg, 2005). Thus, emotional, cognitive, and behavioral avoidance, rooted in early and ongoing minority stress, represents one possible pathway uniting minority stress with gay and bisexual men’s psychosocial syndemics.
Ongoing, including daily, experiences with discrimination, harassment, ambiguously stigmatizing social encounters, and sexual orientation concealment may predispose gay and bisexual men to chronic hypervigilance (Major & O’Brien, 2005; Pachankis, 2007). Hypervigilance in the form of expectations of gay-related rejection has been shown to be associated with depression, social anxiety, substance use, sexual compulsivity, and intimate partner violence among gay and bisexual men (Carvalho et al., 2011; Feinstein et al., 2012; Pachankis et al., 2008, 2014b, 2014c, in press). Emerging evidence from the social neuroscience of stigma and experimental manipulations of stigma-related threat suggests that hyper-vigilance for stigma-related threat can deplete the self-regulation necessary to stave off psychosocial difficulties (Derks, Inzlicht, Kang, 2008; Inzlicht, McKay, & Aronson, 2006). In fact, psychosocial difficulties such as depression, anxiety, substance abuse, intimate partner violence, body image disturbance and eating disorders, and sexual compulsivity have been argued to involve failures of self-regulation, particularly likely to be activated under threatening circumstances (e.g., Ayduk et al., 2000; Baumeister, 1997; Baumeister, Heatherton, & Tice, 1994; Gailliot & Baumeister, 2007; Heatherton & Wagner, 2011; Muraven & Baumeister, 2000; Strauman, 2002). Thus, threat hypervigilance represents another promising syndemic pathway related to both minority stress and multiple syndemic conditions that may be amenable to transdiagnostic intervention approaches.
The final negative valence construct potentially serving as a syndemic pathway includes loss. Loss is endemic to several accounts of gay and bisexual men’s identity development and community attachment. For example, the coming out process has been argued to involve an exit of heterosexuality (Cochran, 2001; D’Augelli, 1998) and the attendant loss of heterosexual privilege (e.g., Badgett, 1995; Tilcsik, 2011). Coming out also involves the loss of certain roles as one embarks on an uncharted life path compared to the more standard traditions, milestones, and expectations of heterosexuality (Siegel & Lowe, 1994). Further, gay and bisexual men, especially of the so-called AIDS generation, often experienced an acute loss of friends, partners, and community (Halkitis, 2013). Experiences of loss, in turn, are associated with depressive symptoms, substance use, and several other psychosocial health problems among the general population and gay and bisexual men specifically (Folkman, Chesney, Collette, Boccellari, & Cooke, 1996; Martin & Hetrick, 1988; Sikkema, Kochman, DiFranceisco, Kelly, & Hoffmann, 2003). Thus, future research might confirm that loss does, in fact, represent a shared pathway across gay and bisexual men’s syndemic conditions capable of being mitigated with cross-cutting treatment approaches.
Possible Positive Valence Pathways: Approach Motivation, Reward Learning, and Habit
The positive valence system includes approach motivation, reward learning, and habit. Approach motivation encompasses reward expectancies, effort valuation, and cost−benefit decision-making. Reward learning refers to reinforcement learning about positive outcomes. Habit refers to behaviors that do not require conscious oversight once initiated (NIMH, 2011). Strong evidence exists that stress, of the type to which gay and bisexual men are disproportionately exposed from an early age, disrupts neurobiological stress pathways, manifesting in impairments in these motivational systems (Sinha, 2008). These impairments, marked by impulsivity in the face of stress, for example, are in turn associated with substance abuse, other addictive behaviors, and eating disturbances (Dawe & Loxton, 2004; Fox, Bergquist, Gu, & Sinha, 2010; Hyman, Malenka, & Nestler, 2006). Depression and anxiety have also been argued to reflect impairments in motivational systems involving reward learning and habit (e.g., Eshel & Roisere, 2010). While studies generally have not investigated whether gay and bisexual men experience disproportionate disruptions in positive valence systems compared to heterosexual men and whether minority stress experiences in particular are associated with such disruptions, the consistent associations among stress, positive valence disruptions, and psychosocial syndemic conditions, with clearly overlapping and interacting neurological pathways in the general population (Li & Sinha, 2008), suggest that components of the positive valence system might serve as promising pathways to consider in transdiagnostic sydemic treatment approaches for gay and bisexual men.
Possible Social Pathways: Disrupted Attachment, Low Agency, Social Submission, Poor Social Communication, and Low Self-Knowledge
The social pathways outlined in the RDoC framework also represent possible common pathways that unite minority stress with syndemic conditions. Examples of social pathways outlined in the RDoC and relevant to gay and bisexual men’s stress and health include disrupted attachment, low agency, social submission, poor social communication, and low self-knowledge. As reviewed below, minority stress consistently demonstrates significant associations with each of these possible social pathways, which in turn are associated with gay and bisexual men’s syndemic conditions.
Several minority stressors are associated with disrupted attachment among gay and bisexual men. For example, research demonstrates that sexual orientation concealment (Mohr & Fassinger, 2003), internalized homophobia (Sherry, 2007), and lack of maternal support of one’s sexual orientation (Mohr & Fassinger, 2003) are associated with both avoidant and anxious attachment. Lack of acceptance from parents, peers, and social institutions, which sexual minority individuals disproportionally experience compared to heterosexuals (Balsam et al., 2005; Friedman et al., 2008; Russell et al., 2011), has also been shown to sensitize gay and bisexual men to expect rejection in ongoing relationships—a key component of insecure attachment styles (Feinstein et al., 2012; Pachankis et al., 2008; Tharinger & Wells, 2000). Insecure attachment demonstrates clear links with several of the syndemic conditions experienced by gay and bisexual men, possibly through its association with unassertive communication (Pachankis et al., 2008). Fears of rejection, for example, which represent a key component of insecure attachment (Downey & Feldman, 1996), predict low condom use assertion with clear implications for HIV infection (Hart & Heimberg, 2005). Insecure attachment is also related to depression and anxiety (Zakalik & Wei, 2006), substance abuse including substance use for stress reduction (Kassel, Wardle, & Roberts, 2007), intimate partner violence (McKenry, Serovich, Mason, & Mosack, 2006), eating disorders and body image diturbance (Ward, Ramsay, & Treasure, 2000), and sexual compulsivity (Corley & Kort, 2006; Zapf, Greiner, & Carroll, 2008). Given consistent relationships between attachment processes and minority stress, on one hand, and attachment processes and syndemic outcomes, on the other, attachment processes represent a plausible syndemic pathway. It is also possible that disrupted attachment may result from negative valence pathways (e.g., avoidance, hypervigilance, loss), forming of a sequence of syndemic pathways.
Minority stress can also erode gay and bisexual men’s sense of agency, yield poor social communication, and encourage submissive social behaviors. Because of their socially marginalized status, gay and bisexual men are particularly likely to encounter persistent and uncontrollable stressors from an early age (Balsam et al., 2005; Friedman et al., 2008; Russell et al., 2011). As mentioned above, gay and bisexual men are disproportionately subject to childhood sexual abuse, peer assault, parental physical abuse, and parental rejection. Even discovering and navigating one’s non-heterosexual sexual orientation in relative isolation from an early age can represent a persistent and uncontrollable stressor (Pachankis, 2007; Pachankis & Hatzenbuehler, 2013). Further, local and national discriminatory laws, policies, and community attitudes affecting gay and bisexual men communicate the social inferiority of gay and bisexual men by treating them as less deserving of the same rights and opportunities afforded to heterosexuals (Hatzenbuehler, 2010; Pachankis et al., 2014a). Social learning theory and research show that persistent exposure to relatively uncontrollable social stressors instills a diminished sense of agency for coping with future stressors (Chorpita & Barlow, 1998). As persistent and uncontrollable stress predicts low agency in the general population stigma-related stress, such as internalized homophobia (Huebner, Davis, Nemeroff, & Aiken, 2002; Ratti, Bakeman, & Peterson, 2000) and sexual orientation concealment (Pachankis, 2007), predict poor self-efficacy for enacting health-promoting social behaviors, such as condom use, that involve assertive social communication. In addition to associations with health-risk behavior (Bandura, 1990), low agency is related to depression and anxiety (Abramson, Seligman, & Teasdale, 1978; Mineka & Zinbarg, 2006), addictive behaviors (DiClemente, Fairhurst, Piotrowski, 1995), eating disorders and body image disturbance (Fairburn, Shafran, & Cooper, 1999), and intimate partner violence (Felson & Outlaw, 2007). While animal research shows that persistent, uncontrollable stress is also associated with socially submissive behavior (Gardner, Thrivikraman, Lightman, Plotsky, & Lowry, 2005; Williams & Lierle, 1986), potential associations between this form of stress and syndemic outcomes experiences by gay and bisexual men await future research. Given their associations with minority stress and syndemic conditions, low agency and communication deficits might represent plausible syndemic pathways, while socially submissive behavior awaits further empirical evidence supporting its role in this model.
The RDoC framework defines self-knowledge as “The ability to make judgments about one’s current cognitive or emotional internal states, traits, and/or abilities” (NIMH, 2011). While scant research exists to suggest that low self-knowledge might serve as a syndemic pathway, it is included as a plausible pathway here given (1) findings from general adolescent samples showing that social rejection confers risk for poor emotion awareness—a form of poor self-knowledge—and that the relationship between social rejection and mental health outcomes is prospectively mediated by poor emotion awareness (e.g., McLaughlin, Hatzenbuehler, & Hilt, 2009), (2) research showing that gay and bisexual adolescents demonstrate lower awareness of their emotional states compared to heterosexual adolescents (Hatzenbuehler et al., 2008b), and (3) research showing that daily experiences of minority stress are associated with more emotional suppression among sexual minority individuals (Hatzenbuehler et al., 2009). In the context of stigmatizing social climates, marked by peer or parental rejection, gay and bisexual men might develop poor emotion regulation strategies, including an inability to trust their own emotions as valid sources of their wants, needs, or desires, or to adaptively act on their emotions. For example, young gay and bisexual men might learn that emotional displays are gender atypical and therefore attempt to disavow or suppress their emotional experience or its expression (Taywaditep, 2001). Research showing that minority stress is associated with emotional suppression among sexual minority individuals provides initial support for this hypothesis (Hatzenbuehler et al., 2009). Research conducted with general population samples demonstrates that low emotional self-knowledge is associated with substance use problems (Michael, 1990), eating and body image disturbance (Bydlowski et al., 2005), intimate partner violence (Winters, Clift, & Dutton, 2004), and sexual compulsivity (Reid, Carpenter, Spackman, & Willes, 2008). In these disorders of emotion regulation, individuals avoid experiencing or expressing painful emotions, which then drives behaviors to alleviate emotional discomfort in the short-term although they yield ineffective long-term behavioral patterns. While emerging evidence suggests that sexual minority individuals might have poorer emotional self-knowledge than heterosexuals (Hatzenbuehler et al., 2008b), additional research is needed to assess additional forms of poor self-awareness among gay and bisexual men both in reaction to minority stress and as a mediator of the minority stress–syndemic relationship.
Future Research Directions on Minority Stress–Syndemic Pathways
The above list of possible pathways is neither complete nor certain. The RDoC mechanisms reviewed above are offered as examples of the type of pathways that might unite minority stress and psychosocial health outcomes. Other potential pathways outlined in the RDoC framework (e.g., working memory deficits, frustrative non-reward) might also be related to minority stress and syndemic conditions facing gay and bisexual men, although less evidence currently exists for these relationships than for the pathways reviewed above.
Further, while most of the hypothesized pathways identified above possess demonstrated relationships with both minority stress and gay and bisexual men’s psychosocial syndemic conditions, only scant evidence exists that these possible pathways in fact serve as mediators of the stress–syndemic relationship. Hatzenbuehler (2009) proposes a psychological mediation framework that includes psychological variables that statistically mediate associations between minority stress and anxiety, depression, and alcohol use problems. These variables include coping motives and positive alcohol expectancies as mediators of the minority stress—alcohol use disorder symptom relationship (Hatzenbuehler et al., 2008c) and rumination, social isolation, social support, pessimism, and self-esteem as mediators of the minority stress—depression and anxiety symptoms relationship (Diaz, Ayala, Bein, Henne, & Marin, 2001; Hatzenbuehler et al., 2009; Hershberger & D’Augelli, 1995). Most of these psychological mediators are related to those included in the RDoC’s list of possible pathways reviewed above. For example, rumination and pessimism likely represent the cognitive components of avoidance and hypervigilance (Borkovec, Ray, & Stober, 1998; Stapinski, Abbott, & Rapee, 2010), whereas social isolation likely represents a behavioral avoidance component of fear (Cacioppo et al., 2000). Positive alcohol expectancies are certainly related to reward learning (Goldman, 2002), whereas agency is central to self-esteem (Kernis, 1995). Thus, the present review extends Hatzenbuehler’s (2009) review of psychological mechanisms involved in depression, anxiety, and alcohol use problems to include a comprehensive list of theoretically plausible mechanisms, grounded in the behavioral science and neurobiological approach of the RDoC, that are implicated across all psychosocial syndemic conditions facing gay and bisexual men, including depression and anxiety, substance use, intimate partner violence, body image concerns and eating disorders, and sexual compulsivity.
Future research on minority stress–syndemic pathways should examine the presence of mediation across the pathways proposed here. The presence of mediation would suggest that treatments addressing these pathways can be expected to produce desired changes in syndemic outcomes. Future research should also test the functional equivalence of syndemic symptoms, investigating, for example, whether syndemic symptoms such as sexual compulsivity and intimate partner violence are united in being means of coping with uncomfortable emotional experiences or in being driven by maladaptive self- and other schemas. This research could apply the affective neuroscience, social neuroscience, and stress physiology research that forms much of the basis of the RDoC, to minority stressors specifically. For example, research paradigms for investigating the neural correlates of social rejection (e.g., Slavich, Way, Eisenberger, & Taylor, 2010) can be adapted to examining the neural correlates of gay and bisexual men’s minority stress and the range of cognitive, affective, and behavioral responses that minority stress neural circuitry impels. Further, existing research suggests the possibility of chronically disrupted stress and immune pathways among socially stressed gay and bisexual men by showing, for example, that gay and bisexual men who disclose their sexual orientation at work have higher levels of salivary cortisol on work days compared to non-work days (Huebner & Davis, 2005), and that HIV-positive rejection-sensitive gay men who disclose their sexual orientation have weaker HIV-related immune responses than rejection-sensitive gay men who conceal their sexual orientation (Cole, Kemeny, & Taylor, 1997). Knowing whether chronically disrupted stress and immune pathways—established correlates of psychiatric and physical health outcomes in the general population (e.g., Dantzer, O’Connor, Freund, Johnson, & Kelley, 2008; Nijm & Jonasson, 2009; Yehuda et al., 2000)—drive syndemic conditions among gay and bisexual men would further validate the stress pathways reviewed above as key treatment targets capable of generalizing across conditions. The search for underlying pathways would bring needed unity and coherence to the field of psychosocial intervention research capable of alleviating gay and bisexual men’s psychosocial syndemic health conditions.
Toward Transdiagnostic Psychosocial Syndemic Treatment Principles for Gay and Bisexual Men
The above review suggests that developing separate treatments for separate psychosocial syndemic conditions might be unduly inefficient given that syndemic conditions, by definition, co-occur, and are potentially united by the shared minority stress pathways reviewed above. Thus, deploying a core set of treatment principles capable of addressing minority stress pathways shared across these co-occurring psychosocial health problems represents a more efficient and potentially more effective strategy than deploying separate treatments for each syndemic condition. Further, this approach maximizes constrained researcher and provider resources because testing the effectiveness of transdiagnostic principles and training providers to deliver these transdiagnostic principles would significantly reduce cost and time compared to the development and training of separate treatment protocols for each syndemic condition.
The field of clinical psychology has long called for this type of approach to identifying common mechanisms across mental health problems and developing unified, principle-based treatment approaches capable of addressing these shared mechanisms (e.g., Goldfried, 1980, 2013). The suggestions offered here closely hew to that approach while extending the search for transdiagnostic mechanisms and treatment principles to the full range of syndemic conditions affecting gay and bisexual men that specifically arise from minority stress. However, given that much of the epidemiological research on syndemic conditions among gay and bisexual men relies on dimensional self-report symptom measures rather than objective diagnostic cutoffs (e.g., depressive symptoms rather than major depressive disorder, childhood sexual abuse rather than posttraumatic stress disorder secondary to childhood sexual abuse), clinical recommendations based on these findings should be implemented cautiously until the heuristic model proposed here is examined with objectively measured clinical outcomes.
Below, eight psychosocial treatment principles are offered as examples of those that could potentially be deployed to reduce the pathways through which minority stress might yield syndemic psychosocial conditions (see also Fig. 1). These example principles were garnered from expert clinician consensus and the input of gay and bisexual men who were experiencing several psychosocial syndemic factors including depression and anxiety, substance use, sexual compulsivity, and HIV risk behavior, as described elsewhere (Pachankis, 2014). These principles complement standard cognitive-behavioral treatment (CBT) principles for treating stress-driven emotional disorders in the general population and can likely be seamlessly integrated into standard CBT approaches such as cognitive restructuring, emotional and behavioral exposure, mindfulness, self-monitoring, and relapse prevention (e.g., Linehan, 1993; Marlatt & Donovan, 2005; Mennin & Farach, 2007; Roemer, Orsillo, Salters-Pedneault, 2008). The efficacy of infusing standard CBT with these potential minority stress-reducing principles to reduce minority stress–syndemic pathways is currently being tested in a randomized controlled trial (Pachankis, Hatzenbuehler, Rendina, Safren, & Parsons, 2015). Thus, these principles are offered only as examples capable of stimulating future tests of additional principles and of their ability to simultaneously reduce the multiple syndemic conditions facing gay and bisexual men.
Treatment Principles of Transdiagnostic Minority Stress Syndemic Interventions for Gay and Bisexual Men’s Syndemic Health
Normalize the Adverse Impact of Minority Stress
Stigma often operates in unseen ways to jeopardize the health of sexual minority individuals (Hatzenbuehler, 2010). Further, sexual minority individuals may not have access to the same protective attributional processes that other stigmatized individuals possess by virtue of their stigma being invisible and typically not shared by parents and other early visible role models (Crocker & Major, 1989). Thus, gay and bisexual men may not readily recognize the potential source of their psychosocial difficulties in minority stress and may instead incorrectly attribute their distress to personal failings rather than stigmatizing social forces. Consequently, one treatment principle that potentially cuts across gay and bisexual men’s psychosocial syndemic health conditions involves normalizing the adverse impact of minority stress. This principle parallels earlier developments in the women’s movement that encouraged awareness of the ways in which stigmatizing social messages keep stigmatized minorities down and away from equal access to power and resources necessary for health (Lange, Jakubowski, & McGovern, 1976). Normalizing the multiple forms of distress caused by minority stress and moving blame for this distress toward society rather than oneself provides an initial platform from which to reduce the adverse cognitive-affective and behavioral pathways reviewed above that unite minority stress with gay and bisexual men’s psychosocial syndemics.
Facilitate Emotion Awareness, Regulation, and Acceptance
Given the evidence reviewed above that gay and bisexual men might demonstrate poorer emotion regulation abilities than heterosexual men and that these difficulties are related to both minority stress and multiple psychosocial syndemic health conditions, another potentially effective principle of transdiagnostic syndemic treatments for gay and bisexual men includes the enhancement of emotion regulation skills. Emotion awareness, regulation, and acceptance form the basic components of psychosocial health (Aldao, Nolen-Hoeksema, & Schweizer, 2010). Therefore, treatment approaches that facilitate stress coping through encouraging healthy emotion regulation (e.g., Barlow et al., 2011; Greenberg & Pascual-Leone, 2006; Linehan, 1993; Webb, Miles, & Sheeran, 2012) have the potential to reduce the emotional impact of minority stress through improving the self-knowledge pathway, for example. Further, emotion regulation approaches, such as mindful acceptance and tolerance of impulsive urges (Ostafin & Marlatt, 2008) and valuing delayed rewards (Bickel & Marsch, 2001), can also reduce emotion-driven impulsive behaviors through interrupting the positive valence pathways of approach motivation, reward learning, and habit.
Reduce Avoidance
Experiential avoidance permeates poor psychosocial health (Aldao et al., 2010), including the psychosocial syndemic conditions facing gay and bisexual. As reviewed above, emotional numbing, excessive worry and rumination, and behavioral unassertiveness are all potentially related to minority stress and implicated in the syndemic conditions reviewed here. Therefore, treatment approaches that help gay and bisexual men confront painful emotions, memories, or interpersonal situations in safe contexts can potentially weaken the threat of these events, thereby reducing the avoidance pathway and improving the self-knowledge pathway to reduce the risk of syndemic conditions. Such approaches are grounded in contemporary learning models of fear exposure that show efficacy across emotion-driven behaviors (e.g., Mineka & Zinbarg, 2006).
Empower Assertive Communication
Behavioral unassertiveness represents a core component of avoidance for some gay and bisexual men and is closely related to both minority stress and syndemic outcomes (e.g., Pachankis et al., 2008). Therefore, helping gay and bisexual men systematically confront a hierarchy of feared interpersonal situations, such as open self-expression, sexual orientation disclosure, male intimacy, and acknowledgment of personal imperfection and vulnerability, can foster a healthy, assertive interpersonal stance that early and ongoing experiences with minority stress can otherwise compromise (Pachankis, 2009). The generalization of assertiveness skills across life domains has direct implications for health, for example in the case of condom use assertion (e.g., Hart & Heimberg, 2005). In addition to improving syndemic health through targeting the avoidance pathway, promoting assertive communication could also yield salubrious effects through improving the poor social communication and social submission pathways, given that assertiveness is contrary to both. Of course, the suitability of these behavioral skills heavily depends on the safety of the context; open self-expression and disclosure would be inappropriate in most hostile climates.
Restructure Minority Stress Cognitions
Early and ongoing experiences with minority stress can teach gay and bisexual men that they are weak, overly emotional, deviant, or inferior compared to heterosexual men. These biased beliefs feature prominently in internalized homophobia and rejection hypervigilance, which are associated with poor psychosocial syndemic health (e.g., Huebner et al., 2002; Kimmel & Mahalik, 2005; Newcomb & Mustanski, 2010; Pachankis et al., 2014c, in press; Ratti et al., 2000). Therefore, to treat gay and bisexual men’s psychosocial syndemics, standard cognitive restructuring approaches can be adapted to specifically reduce minority stress-fueled cognitive biases. This adapted cognitive restructuring approach could increase gay and bisexual men’s awareness of the specific ways that minority stress can become internalized and the unhealthy impact this internalization can have, while presenting contradictory evidence highlighting gay and bisexual men’s unique strengths (e.g., Lin & Israel, 2012). While the development of cognitive biases, such as fears of gay-related rejection, may have been adaptive across some gay and bisexual men’s early development because it kept them safe from harm, such biases may be presently maladaptive especially in safer contexts (Pachankis & Goldfried, 2006) and might impair healthy relationships both with heterosexuals (e.g., Pachankis et al., 2008) and other gay and bisexual men (e.g., Frost & Meyer, 2009). Therefore, discussing the ways in which minority stress-driven cognitive biases may have outlived their original utility might facilitate the eventual reworking of these cognitions. In this way, restructuring minority stress-related cognitive biases can reduce several potential syndemic pathways such as avoidance, hypervigilance, habit, disrupted attachment, and low agency. On the other hand, reducing hypervigilance may not be appropriate for all gay and bisexual men in all contexts, such as men living in pervasively discriminatory or criminalizing settings where danger represents an unfortunate and unjust reality.
Validate Sexual Minority Individuals’ Unique Strengths
Because gay and bisexual men often develop their sexual orientation in relative isolation without the early support of parents and peers, they therefore cannot benefit from early socialization regarding the strengths and protections afforded by their sexual minority status, unlike visible minorities (e.g., Crocker & Major, 1989). Thus, educating gay and bisexual men who face psychosocial syndemic conditions about the historical and contemporary strengths of sexual minority communities can provide an important, often missing, source of identity-related support. Psychosocial approaches to facilitate resilience might highlight the ways that sexual minority communities demonstrate resilience in the face of stigma, including demonstrations of pride, sexual and social creativity, community building, and social activism (e.g., Herrick, Stall, Goldhammer, Egan, & Mayer, 2014). For example, the LGBT community has demonstrated an impressive ability to create non-biological families-of-choice and advocate for itself in the face of an often indifferent mainstream society (e.g., Trapence et al., 2012; Weeks, Heaphy, & Donovan, 2001). Educating gay and bisexual men who are facing syndemic conditions—men who may be particularly unlikely to espouse such resilience—about the remarkable historical and contemporary feats shown by their communities may instill a sense of hope and optimism for alleviating minority stress. In this way, psychosocial approaches that facilitate resilience could buffer gay and bisexual men against any syndemic pathway reviewed above through which minority stress compromises health.
Build Supportive Relationships
While supportive relationships have the ability to protect sexual minorities against the adverse psychosocial effects of minority stress (e.g., Hershberger & D’Augelli, 1995; Rosario, Schrimshaw, & Hunter, 2009), sexual minorities are disproportionately less likely to experience such support compared to heterosexuals (Plöderl & Fartacek, 2005; Safren & Heimberg, 1999). As reviewed above, disrupted attachment, avoidance, loss, poor social communication, and social submission all represent pathways through which minority stress might compromise healthy relationships to produce syndemic health threats, such as depression and anxiety, substance use, intimate partner violence, and sexual compulsivity. Therefore, psychosocial treatment approaches that help gay and bisexual men identify supportive community connections and build healthy relationships can potentially reduce these pathways to improve psychosocial health. Healthy community connections and relationships can be facilitated through (1) identifying healthy and unhealthy members of one’s current social network and replacing unhealthy influences with positive influences (e.g., Marlatt & Donovan, 2005), (2) strengthening connections with parents and other natal family members when possible (e.g., LaSala, 2000), and (3) helping gay and bisexual men in primary partnerships to cope with homophobia, clarify boundaries around their commitments and relationships roles, and build strong social networks through assertiveness and other social skills training (e.g., Green & Mitchell, 2002; Greenan & Tunnell, 2003).
Affirm Healthy, Rewarding Expressions of Sexuality
Gay and bisexual men often first become aware of same-sex attractions during adolescence (Rosario et al., 2006), when they may not have the supportive resources necessary for managing sexual feelings in stigmatizing contexts. Further, given the stigmatizing nature of same-sex sexuality (Herek, 2004), sexual minority sexuality remains relatively unaddressed in mainstream sources of sex education, such as from parents and schools (e.g., Kubicek, Beyer, Weiss, Iverson, & Kipke, 2010). These developmental factors likely combine with minority stress (Zamboni & Crawford, 2007), masculine role norms (Courtenay, 2000), and the ready availability of sex partners in gay male communities (Baum & Fishman, 1994; Missildine et al., 2005) to put gay and bisexual men at risk of multiple sexual health problems compared to heterosexual men, including sexual compulsivity (Missildine et al., 2005), erectile difficulties (Bancroft, Carnes, Janssen, Goodrich, & Long, 2005), and HIV infection (Centers for Disease Control, 2013). Thus, minority stress impairs gay and bisexual men’s sexual health and may operate through several of the above-reviewed syndemic pathways, including avoidance, hypervigilance, approach motivation, reward learning, habit, submissive social behaviors, social communication, disrupted attachment, and agency, to do so.
Psychosocial intervention approaches that affirm healthy, rewarding expressions of sexuality can potentially reduce the pathways reviewed here that are argued to potentially unite minority stress with poor sexual health and other psychosocial syndemic health conditions. Sexual health as conceptualized here stems from the World Health Organization’s definition, which refers not merely to the absence of disease, but “a state of physical, emotional, mental and social well-being in relation to sexuality…a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence” (World Health Organization, 2006). Approaches to instilling sexual health might include, for example, instilling a sex-positive worldview among gay and bisexual men; fostering self-acceptance of their sexual identities, attractions, fantasies, and behaviors; helping them identify sexual goals, including sexual health goals; monitoring sexual patterns and one’s perception of control over his sexuality; cognitive restructuring of rejection-related relational and sexual schemas; and communicating assertively about sexual needs, including sexual safety. Preliminary efficacy exists for sexual health promotion interventions that adopt some of these approaches to improving sexual health (e.g., Mustanski, Greene, Ryan, & Whitton, 2014). Future research is needed to determine if such approaches specifically reduce the syndemic pathways reviewed above and whether they can improve not only sexual health but other psychosocial syndemic health conditions that gay and bisexual men face (e.g., Safren, Blashill, & O’Cleirigh, 2011; Safren, Reisner, Herrick, Mimiaga, & Stall, 2010; Walkup et al., 2008).
Barriers, Solutions, and Future Directions for Transdiagnostic Minority Stress Syndemic Treatment Approaches
The cross-cutting psychosocial treatment principles reviewed above are offered as examples of approaches to treating gay and bisexual men’s psychosocial syndemic health conditions, which by definition co-occur and, thus, would be maximally served by principles targeting not just one syndemic problem, but multiple, functionally equivalent problems at the level of their shared underlying pathways. Thus, future research is needed to identify the effectiveness of these treatment principles for reducing the proposed syndemic pathways. However, in addition to further research on pathways and the efficacy of treatment approaches tied to those pathways, the successful implementation and dissemination of a principle-based, unified minority stress treatment approach will also require principle-based approaches to clinical training and research.
Several current trends in clinical training and research will need to be overcome for a principle-based approach to succeed, including the field’s reliance on technique-focused treatment manuals and the privilege afforded randomized controlled trials over other intervention research approaches (Hershenberg & Goldfried, in press). First, clinicians will need to be trained to deliver empirically supported intervention techniques only in the context of idiographic case conceptualizations that consider the treatment principles relevant to each case. Too often, intervention manuals, originally intended to describe what takes place in research studies, are now often assumed to be prescriptive guides to real-world clinical practice (Westen et al., 2004). However, intervention manuals prescribe the rote application of techniques intended to ensure internal validity in treatment studies and allow little room for considering how overarching principles can flexibly guide case conceptualization built around the underlying mechanisms relevant to each individual and the psychosocial syndemic conditions he is experiencing (Goldfried & Wolfe, 1996).
Further, flexible treatment approaches driven by principle-driven case conceptualization are contrary to the randomized controlled trial (RCT) approach, largely considered the standard by which all psychosocial intervention research should be judged. In RCTs, whole treatment packages are compared to each other, each treatment is delivered according to the techniques specified in the treatment manual, and reductions in discrete symptoms from pre-intervention to post-intervention represent the final goal. Thus, little room is afforded to considering the principles that are best suited to treating a particular cluster of psychosocial conditions driven by a specific set of pathways. Further, the RCT approach to intervention research largely avoids the exploration of change mechanisms, given that the key research question in RCTs is typically whether the treatment reduced discrete symptoms compared to a control treatment, not understanding the mechanisms through which the treatment worked (Westen et al., 2004). However, without knowing the mechanisms through which a treatment works, it is difficult, if not impossible, to ascertain the common mechanisms shared across treatment approaches that can be coherently synthesized to treat multiple co-occurring conditions, as in the case of gay and bisexual men’s psychosocial syndemic health conditions. Further, another final product of an RCT—the intervention manual—is likely to be less-than-helpful to practicing clinicians, who are unlikely to find prescriptive manuals practical given their beliefs about (1) the complexity of their clients’ presenting issues, (2) the relative sophistication of their treatment practices compared to the presumed rote guidance offered in manuals, and (3) the relative importance of non-specific factors such as the therapeutic alliance to their clients’ improvement (Pachankis & Goldfried, 2007a).
While strong contextual factors perpetuate both the application of RCT methodology in psychosocial intervention research (e.g., Goldfried & Wolfe, 1996) and the proliferation of separate treatment manuals for separate psychosocial conditions (Goldfried, 1980), these barriers can potentially be overcome through (1) recognizing the benefit of finer-grained analyses of change mechanisms in psychosocial intervention research (e.g., Pachankis & Goldfried, 2007b) and (2) adopting a principle-based approach to training clinicians (e.g., Pachankis & Goldfried, 2007a). For example, uncovering which mechanisms are implicated in particular individuals’ presenting conditions and which principles are best suited to addressing those mechanisms can be determined by examining mediators of treatment efficacy, closely reviewing session transcripts for the application of principles, and interviewing treatment providers to determine their principle-based clinical decision-making and case conceptualization. Further, providers ought to be receive training in conceptualizing cases according to overarching pathways and principles rather than only the application of intervention techniques to reduce discrete symptoms. In this way, the field can move closer to identifying overarching principles and treatments that can address transdiagnostic pathways implicated in gay and bisexual men’s syndemic conditions.
Conclusion
Given accumulating evidence for the shared processes underlying numerous psychosocial problems among gay and bisexual men, the intervention field’s historic tendency to develop and deploy separate treatments for separate problems seems ill-suited to intervening upon the overlapping psychosocial conditions facing this population. This article reviews possible pathways that underlie gay and bisexual men’s syndemic conditions, locates their source in minority stress, and proposes overarching treatment principles that future research might identify as capable of addressing the pathways through which psychosocial syndemics operate in this population (e.g., Pachankis et al., 2015).
Given that syndemic conditions are ultimately perpetuated by structural factors, such as discriminatory institutions (Singer et al., 2006), the treatment approaches promoted here recognize that the ultimate alleviation of syndemic conditions will flow from changing social structures rather than only promoting stigma coping among gay and bisexual men themselves (Meyer, 2003). Lest social structures be seen as ironclad forces impervious to change, it should be noted that social structures are ultimately composed of individuals, with individuals holding the power to change those structures (Bourdieu, 1990). Activism on the part of stigmatized individuals has successfully abolished stigmatizing social structures throughout history, and while the minority stress treatment approach advocated here does not demand that change in stigmatizing structures solely rely on gay and bisexual men, it does empower them to challenge those structures in a way that promotes health. Promoting stigma coping can also change social structures through promoting positive intergroup contact, and greater visibility of stigmatized individuals, and encouraging stigmatized individuals to be advocates for structural change (Cook, Purdie-Vaughns, Meyer, & Busch, 2014). The treatment principles outlined here encourage all of these changes without solely placing the burden on the stigmatized themselves to change stigmatizing structures. Nonetheless, to ultimately improve conditions of social inequality, all individuals must change, including those who derive status and power from stigmatizing others (Carter & Reardon, 2014).
Cost-effective and wide-reaching delivery platforms can ensure that the type of guidance proposed here, typically disseminated through resource-intensive one-on-one or small group counseling, reaches the most disenfranchised members of the community. For example, incorporating these minority stress treatment principles into internet-based and mobile delivery counseling programs (Pachankis, Lelutiu-Weinberger, Golub, & Parsons, 2013) and into public sector health clinics (Hellman & Klein, 2004) can facilitate dissemination of these treatment principles to rural, concealed, or low-income gay and bisexual men. The evidence-based platform of this proposed treatment approach could also be incorporated into existing LGBT-affirmative psychotherapy services (e.g., Hellman & Klein, 2004), which would represent a particularly apt future direction given that the principles reviewed here largely derived from the wisdom of community practitioners and gay and bisexual men who have received their services (Pachankis, 2014). Bringing an evidence base to this clinical wisdom represents an important advance in clinical practice with gay and bisexual men.
In sum, locating the pathways through which minority stress generates psychosocial syndemics and employing treatment principles capable of alleviating these pathways will ultimately create a unified, transdiagnostic approach to improving gay and bisexual men’s health while potentially also reducing the stigmatizing social forces that impair health in the first place. Future research can validate the minority stress–syndemic pathways suggested here and the efficacy of treatments that target them so that treatments based on this novel approach can ultimately reach the broad population of gay and bisexual men who could potentially benefit from them.
References
Abramson, L. Y., Seligman, M. E., & Teasdale, J. D. (1978). Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology, 87(1), 49–74. doi:10.1037/0021-843X.87.1.49.
Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. doi:10.1016/j.cpr.2009.11.004.
Austin, S. B., Ziyadeh, N., Kahn, J. A., Camargo, C. A., Colditz, G. A., & Field, A. E. (2004). Sexual orientation, weight concerns, and eating-disordered behaviors in adolescent girls and boys. Journal of the American Academy of Child and Adolescent Psychiatry, 43(9), 1115–1123. doi:10.1097/01.chi.0000131139.93862.10.
Ayduk, O., Mendoza-Denton, R., Mischel, W., Downey, G., Peake, P. K., & Rodriguez, M. (2000). Regulating the interpersonal self: Strategic self-regulation for coping with rejection sensitivity. Journal of Personality and Social Psychology, 79(5), 776–792. doi:10.1037/0022-3514.79.5.776.
Badgett, M. L. (1995). The wage effects of sexual orientation discrimination. Industrial and Labor Relations Review, 48, 726–739. doi:10.2307/2524353.
Balsam, K. F., Rothblum, E. D., & Beauchaine, T. P. (2005). Victimizatino over the life span: A comparison of lesbian, gay, bisexual, and heterosexual siblings. Journal of Consulting and Clinical Psychology, 73(3), 477–487. doi:10.1037/0022-006X.73.3.477.
Bancroft, J., Carnes, L., Janssen, E., Goodrich, D., & Long, J. S. (2005). Erectile and ejaculatory problems in gay and heterosexual men. Archives of Sexual Behavior, 34(3), 285–297. doi:10.1007/s10508-005-3117-7.
Bandura, A. (1990). Perceived self-efficacy in the exercise of control over AIDS infection. Evaluation and Program Planning, 13(1), 9–17. doi:10.1016/0149-7189(90)90004-G.
Barlow, D. H., Allen, L. B., & Choate, M. L. (2004). Toward a unified treatment for emotional disorders. Behavior Therapy, 35(2), 205–230. doi:10.1016/S0005-7894(04)80036-4.
Barlow, D. H., Farchione, T. J., Fairholme, C. P., Ellard, K. K., Boisseau, C. L., Allen, L. B., & Ehrenreich-May, J. (2011). Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York: Oxford University Press.
Batten, S. V., Follette, V. M., & Aban, I. B. (2002). Experiential avoidance and high-risk sexual behavior in survivors of child sexual abuse. Journal of Child Sexual Abuse, 10(2), 101–120. doi:10.1300/J070v10n02_06.
Baum, M. D., & Fishman, J. M. (1994). AIDS, sexual compulsivity, and gay men: A group treatment approach. In S. A. Cadwell, R. A. Burnham Jr, & M. Forstein (Eds.), Therapists on the front line: Psychotherapy with gay men in the age of AIDS (pp. 255–274). Arlington, VA: American Psychiatric Association.
Baumeister, R. F. (1997). Esteem threat, self-regulatory breakdown, and emotional distress as factors in self-defeating behavior. Review of General Psychology, 1(2), 145–174. doi:10.1037/1089-2680.1.2.145.
Baumeister, R. F., Heatherton, T. F., & Tice, D. M. (1994). Losing control: How and why people fail at self-regulation. San Diego, CA: Academic Press.
Bickel, W. K., & Marsch, L. A. (2001). Toward a behavioral economic understanding of drug dependence: Delay discounting processes. Addiction, 96(1), 73–86. doi:10.1046/j.1360-0443.2001.961736.x.
Borkovec, T. D., Ray, W. J., & Stöber, J. (1998). Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Cognitive Therapy and Rsearch, 22(6), 561–576. doi:10.1023/A:1018790003416.
Bourdieu, P. (1990). The logic of practice. Stanford University Press.
Brady, K. T., & Sinha, R. (2007). Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. FOCUS, 5(2), 229–239.
Bremner, J. D., Vermetten, E., Schmahl, C., Vaccarino, V., Vythilingam, M., … Charney, D. (2005). Positron emission tomographic imaging of neural correlates of a fear acquisition and extinction paradigm in women with childhood sexual-abuse-related post-traumatic stress disorder. Psychological Medicine, 35(6), 791–806. doi:10.1017/S0033291704003290.
Brennan, D. J., Craig, S. L., & Thompson, D. E. A. (2012). Factors associated with a drive for muscularity among gay and bisexual men. Culture Health and Sexuality, 14(1), 1–15. doi:10.1080/13691058.2011.619578.
Brubaker, M. D., Garrett, M. T., & Dew, B. J. (2009). Examining the relationship between internalized heterosexism and substance abuse among lesbian, gay, and bisexual individuals: A critical review. Journal of LGBT Issues in Counseling, 3(1), 62–89. doi:10.1080/15538600902754494.
Bydlowski, S., Corcos, M., Jeammet, P., Paterniti, S., Berthoz, S., Laurier, C., et al. (2005). Emotion-processing deficits in eating disorders. International Journal of Eating Disorders, 37(4), 321–329. doi:10.1002/eat.20132.
Cacioppo, J. T., Ernst, J. M., Burleson, M. H., McClintock, M. K., Malarkey, W. B., Hawkley, L. C., … Berntson, G. G. (2000). Lonely traits and concomitant physiological processes: The MacArthur social neuroscience studies. International Journal of Psychophysiology, 35(2–3), 143–154. doi:10.1016/s0167-8760(99)00049-5.
Carter, P. L., & Reardon, S. F. (2014). Inequality matters: A William T. Grant Foundation inequality paper. New York, NY: William T. Grant Foundation.
Carvalho, A. F., Lewis, R. J., Derlega, V. J., Winstead, B. A., & Viggiano, C. (2011). Internalized sexual minority stressors and same-sex intimate partner violence. Journal of Family Violence, 26(7), 501–509. doi:10.1007/s10896-011-9384-2.
Centers for Disease Control and Prevention. (2013). HIV and AIDS among gay and bisexual men. Atlanta, GA: Centers for Disease Control and Prevention. doi:10.1007/978-1-4614-5283-6_17.
Chorpita, B. F., & Barlow, D. H. (1998). The development of anxiety: The role of control in the early environment. Psychological Bulletin, 124(1), 3–21. doi:10.1037/0033-2909.124.1.3.
Cochran, S. D. (2001). Emerging issues in research on lesbians’ and gay men’s mental health: Does sexual orientation really matter? The American Psychologist, 56(11), 931–947. doi:10.1037/0003-066x.56.11.931.
Cochran, S. D., Grella, C. E., Mays, V., et al. (2012). Do substance use norms and perceived drug availability mediate sexual orientation differences in patterns of substance use? Results from the California Quality of Life Survey II. Journal of Studies on Alcohol and Drugs, 73(4), 675–685.
Cole, S. W., Kemeny, M. E., & Taylor, S. E. (1997). Social identity and physical health: accelerated HIV progression in rejection-sensitive gay men. Journal of Personality and Social Psychology, 72(2), 320–335. doi:10.1037/0022-3514.72.2.320.
Cook, J. E., Purdie-Vaughns, V., Meyer, I. H., & Busch, J. T. (2014). Intervening within and across levels: A multilevel approach to stigma and public health. Social Science and Medicine, 103, 101–109. doi:10.1016/j.socscimed.2013.09.023.
Corley, M. D., & Kort, J. (2006). The sex addicted mixed-orientation marriage: Examining attachment styles, internalized homophobia, and viability of marriage after disclosure. Sexual Addiction and Compulsivity, 13, 167–193. doi:10.1080/10720160600870737.
Courtenay, W. H. (2000). Constructions of masculinity and their influence on men’s well-being: A theory of gender and health. Social Science and Medicine, 50(10), 1385–1401. doi:10.1016/s0277-9536(99)00390-1.
Crocker, J., & Major, B. (1989). Social stigma and self-esteem: The self-protective properties of stigma. Psychological Review, 96, 608–630. doi:10.1037/0033-295X.96.4.608.
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W., & Kelley, K. W. (2008). From inflammation to sickness and depression: when the immune system subjugates the brain. Nature Reviews Neuroscience, 9(1), 46–56. doi:10.1038/nrn2297.
D’Augelli, A. R. (1998). Developmental implications of victimization of lesbian, gay, and bisexual youths. In G. M. Herek (Ed.), Stigma and sexual orientation: Understanding prejudice against lesbians, gay men, and bisexuals (pp. 187–210). Thousand Oaks, CA: Sage.
Dawe, S., & Loxton, N. J. (2004). The role of impulsivity in the development of substance use and eating disorders. Neuroscience and Biobehavioral Reviews, 28(3), 343–351. doi:10.1016/j.neubiorev.2004.03.007.
Derks, B., Inzlicht, M., & Kang, S. (2008). The neuroscience of stigma and stereotype threat. Group Processes and Intergroup Relations, 11(2), 163–181. doi:10.1177/1368430207088036.
Diaz, R. M., Ayala, G., Bein, E., Henne, J., & Marin, B. V. (2001). The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: Findings from 3 U.S. cities. American Journal of Public Health, 91(6), 927–932. doi:10.2105/ajph.91.6.927.
DiClemente, C. C., Fairhurst, S. K., & Piotrowski, N. A. (1995). Self-efficacy and addictive behaviors. In J. E. Maddux (Ed.), Self-efficacy, adaptation, and adjustment: Theory, research, and application (pp. 109–141). New York, NY: Plenum Press.
Dohrenwend, B. P. (2000). The role of adversity and stress in psychopathology: Some evidence and its implications for theory and research. Journal of Health and Social Behavior, 41, 1–19.
Downey, G., & Feldman, S. I. (1996). Implications of rejection sensitivity for intimate relationships. Journal of Personality and Social Psychology, 70(6), 1327–1343. doi:10.1037/0022-3514.70.6.1327.
Edwards, K. M., & Sylaska, K. M. (2013). The perpetration of intimate partner violence among LGBTQ college youth: The role of minority stress. Journal of Youth and Adolescence, 42(11), 1721–1731. doi:10.1007/s10964-012-9880-6.
Egan, J. E., Frye, V., Kurtz, S. P., Latkin, C., Chen, M., Tobin, K., … Koblin, B. A. (2011). Migration, neihborhoods, and networks: Approaches to understanding how urban environmental conditions affect syndemic adverse health outcomes among gay, bisexual, and other men who have sex with men. AIDS and Behavior, 15(Suppl. 1), S35–S50. doi:10.1007/s10461-011-9902-5.
Ellard, K. K., Fairholme, C. P., Boisseau, C. L., Farchione, T. J., & Barlow, D. H. (2010). Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice, 17(1), 88–101. doi:10.1016/j.cbpra.2009.06.002.
Eshel, N., & Roisere, J. P. (2010). Reward and punishment processing in depression. Biological Psychiatry, 68(2), 118–124. doi:10.1016/j.biopsych.2010.01.027.
Etkin, A., & Wager, T. D. (2007). Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. American Journal of Psychiatry, 164(10), 1476–1488. doi:10.1176/appi.ajp.2007.07030504.
Fairburn, C. G., Shafran, R., & Cooper, Z. (1999). A cognitive behavioural theory of anorexia nervosa. Behaviour Research and Therapy, 37(1), 1–13. doi:10.1016/s0005-7967(98)00102-8.
Farchione, T. J., Fairholme, C. P., Ellard, K. K., Boisseau, C. L., Thompson-Hollands, J., Carl, J. R., … Barlow, D. H. (2012). Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behavior Therapy, 43(3), 666–678. doi:10.1016/j.beth.2012.01.001.
Feinstein, B. A., Goldfried, M. R., & Davila, J. (2012). The relationship between experiences of discrimination and mental health among lesbians and gay men: An examination of internalized homonegativity and rejection sensitivity as potential mechanisms. Journal of Consulting and Clinical Psychology, 80(5), 917–927. doi:10.1037/a0029425.
Feldman, M. B., & Meyer, I. H. (2007). Eating disorders in diverse lesbian, gay, and bisexual populations. International Journal of Eating Disorders, 40(3), 218–226. doi:10.1002/eat.20360.
Felson, R. B., & Outlaw, M. C. (2007). The control motive and marital violence. Violence and Victims, 22(4), 387–407. doi:10.1891/088667007781553964.
Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. doi:10.1037/0033-2909.99.1.20.
Folkman, S., Chesney, M., Collette, L., Boccellari, A., & Cooke, M. (1996). Postbereavement depressive mood and its prebereavement predictors in HIV + and HIV− gay men. Journal of Personality and Social Psychology, 70(2), 336–348. doi:10.1037/0022-3514.70.2.336.
Fox, H. C., Bergquist, K. L., Gu, P., & Sinha, R. (2010). Interactive effects of cumulative stress and impulsivity on alcohol consumption. Alcoholism: Clinical and Experimental Research, 34(8), 1376–1385. doi:10.1111/j.1530-0277.2010.01221.x.
Fresco, D. M., Frankel, A. N., Mennin, D. S., Turk, C. L., & Heimberg, R. G. (2002). Distinct and overlapping features of rumination and worry: The relationship of cognitive production to negative affective states. Cognitive Therapy and Research, 26(2), 179–188. doi:10.1023/A:1014517718949.
Friedman, M. S., Marshal, M. P., Stall, R., Cheong, J., & Wright, E. R. (2008). Gay-related development, early abuse and adult health outcomes among gay males. AIDS and Behavior, 12(6), 891–902. doi:10.1007/s10461-007-9319-3.
Frost, D. M., & Meyer, I. H. (2009). Internalized homophobia and relationship quality among lesbians, gay men, and bisexuals. Journal of Counseling Psychology, 56(1), 97–109. doi:10.1037/a0012844.
Gailliot, M. T., & Baumeister, R. F. (2007). Self-regulation and sexual restraint: Dispositionality and temporarily poor self-regulatory abilities contribute to failures at restraining sexual behavior. Personality and Social Psychology Bulletin, 33(2), 173–186. doi:10.1177/0146167206293472.
Gardner, K. L., Thrivikraman, K. V., Lightman, S. L., Plotsky, P. M., & Lowry, C. A. (2005). Early life experience alters behavior during social defeat: Focus on serotonergic systems. Neuroscience, 136(1), 181–191. doi:10.1016/j.neuroscience.2005.07.042.
Goldfried, M. R. (1980). Toward the delineation of therapeutic change principles. American Psychologist, 35(11), 991–999. doi:10.1037/0003-066X.35.11.991.
Goldfried, M. R. (2013). What should we expect from psychotherapy? Clinical Psychology Review, 33(7), 862–869. doi:10.1016j/j.cpr.2013.05.003.
Goldfried, M. R., & Wolfe, B. E. (1996). Psychotherapy practice and research: Repairing a strained relationship. American Psychologist, 51(10), 1007–1016. doi:10.1037/0003-066X.51.10.1007.
Goldman, M. S. (2002). Expectancy and risk for alcoholism: The unfortunate exploitation of a fundamental characteristic of neurobehavioral adaptation. Alcoholism: Clinical and Experimental Research, 26(5), 737–746. doi:10.1111/j.1530-0277.2002.tb02599.x.
Gratz, K. L., Bornovalova, M. A., Delany-Brumsey, A., Nick, B., & Lejuez, C. W. (2007). A laboratory-based study of the relationship between childhood abuse and experiential avoidance among inner-city substance users: The role of emotional nonacceptance. Behavior Therapy, 38(3), 256–268. doi:10.1016/j.beth.2006.08.006.
Green, K. E., & Feinstein, B. A. (2012). Substance use in lesbian, gay, and bisexual populations: An update on empirical research and implications for treatment. Psychology of Addictive Behaviors, 26(2), 265–278. doi:10.1037/a0025424.
Green, R., & Mitchell, V. (2002). Gay and lesbian couples in therapy: Homophobia, relational ambiguity, and social support. In A. S. Gurman & N. S. Jacobson (Eds.), Clinical handbook of couple therapy (3rd ed., pp. 546–568). New York, NY: Guilford Press.
Greenan, D. E., & Tunnell, G. (2003). Couple therapy with gay men. New York, NY: Guilford Press.
Greenberg, L. S., & Pascual-Leone, A. (2006). Emotion in psychotherapy: A practice-friendly research review. Journal of Clinical Psychology, 62(5), 611–630. doi:10.1002/jclp.20252.
Hains, A. B., & Arnsten, A. F. T. (2008). Molecular mechanisms of stress-induced prefrontal cortical impairment: Implications for mental illness. Learning and Memory, 15(8), 551–564. doi:10.1101/lm.921708.
Halkitis, P. N. (2010). Reframing HIV prevention for gay men in the United States. American Psychologist, 65(8), 752–763.
Halkitis, P. N. (2013). The AIDS generation: Stories of survival and resilience. New York, NY: Oxford University Press.
Hamilton, C. J., & Mahalik, J. R. (2009). Minority stress, masculinity, and social norms predicting gay men’s health risk behaviors. Journal of Counseling Psychology, 56(1), 132–141. doi:10.1037/a0014440.
Hart, T. A., & Heimberg, R. G. (2005). Social anxiety as a risk factor for unprotected intercourse among gay and bisexual male youth. AIDS and Behavior, 9(4), 505–512. doi:10.1007/s10461-005-9021-2.
Hatzenbuehler, M. L. (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135(5), 707–730. doi:10.1037/a0016441.
Hatzenbuehler, M. L. (2010). Social factors as determinants of mental health disparities in LGB populations: Implications for public policy. Social Issues and Policy Review, 4(1), 31–62. doi:10.1111/j.1751-2409.2010.01017.x.
Hatzenbuehler, M. L., Corbin, W. R., & Fromme, K. (2008a). Trajectories and determinants of alcohol use among LGB young adults and their heterosexual peers: Results from a prospective study. Developmental Psychology, 44(1), 81–90. doi:10.1037/0012-1649.44.1.81.
Hatzenbuehler, M. L., McLaughlin, K. A., & Nolen-Hoeksema, S. (2008b). Emotion regulation and internalizing symptoms in a longitudinal study of sexual minority and heterosexual adolescents. Journal of Child Psychology and Psychiatry, 49, 1270–1278. doi:10.1111/j.1469-7610.2008.01924.x.
Hatzenbuehler, M. L., Nolen-Hoeksema, S., & Dovidio, J. (2009). How does stigma “get under the skin”? The mediating role of emotion regulation. Psychological Science, 20(10), 1282–1289. doi:10.1111/j.1467-9280.2009.02441.x.
Hatzenbuehler, M. L., Nolen-Hoeksema, S., & Erickson, S. J. (2008c). Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: Results from a prospective study of bereaved gay men. Health Psychology, 27(4), 455–462. doi:10.1037/0278-6133.27.4.455.
Heatherton, T. F., & Wagner, D. D. (2011). Cognitive neuroscience of self-regulation failure. Trends in Cognitive Sciences, 15(3), 132–139. doi:10.1016/j/tics.2010.12.005.
Heim, C., Owens, M. J., Plotsky, P. M., & Nemeroff, C. B. (1997). Persistent change in corticotropin-releasing factor systems due to early life stress: Relationship to the pathophysiology of major depression and post-traumatic stress disorder. Psychopharmacology Bulletin, 33(2), 185–192.
Hellman, R. E., & Klein, E. (2004). A program for lesbian, gay, bisexual, and transgender individuals with major mental illness. Journal of Gay & Lesbian Psychotherapy, 8(3–4), 67–82.
Herek, G. M. (2004). Beyond “homophobia”: Thinking about sexual prejudice and stigma in the twenty-first century. Sexuality Research and Social Policy, 1(2), 6–24. doi:10.1525/srsp.2004.1.2.6.
Herrick, A. L., Stall, R., Goldhammer, H., Egan, J. E., & Mayer, K. H. (2014). Resilience as a research framework and as a cornerstone of prevention research for gay and bisexual men: Theory and evidence. AIDS and Behavior, 18, 1–9. doi:10.1007/s10461-012-0384-x.
Hershberger, S. L., & D’Augelli, A. R. (1995). The impact of victimization on the mental health and suicidality of lesbian, gay, and bisexual youths. Developmental Psychology, 31(1), 65–74. doi:10.1037/0012-1649.31.1.65.
Hershenberg, R., & Goldfried, M. R. (in press). Implications of RDoC for the research and practice of psychotherapy. Behavior Therapy. doi:10.1016/j.beth.2014.09.014.
Huebner, D. M., & Davis, M. C. (2005). Gay and bisexual men who disclose their sexual orientations in the workplace have higher workday levels of salivary cortisol and negative affect. Annals of Behavioral Medicine, 30(3), 260–267. doi:10.1207/s15324796abm3003_10.
Huebner, D. M., Davis, M. C., Nemeroff, C. J., & Aiken, L. S. (2002). The impact of internalized homophobia on HIV preventive interventions. American Journal of Community Psychology, 30(3), 327–348. doi:10.1023/A:1015325303002.
Hyman, S. E., Malenka, R. C., & Nestler, E. J. (2006). Neural mechanisms of addiction: The role of reward-related learning and memory. Annual Review of Neuroscience, 29, 565–598. doi:10.1146/annurev.neuro.29.051605.113009.
Insel, T., Cuthbert, B., Garvey, M., Heinssen, R., Pine, D. S., Quinn, K., ... Wang, P. (2010). Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry, 167(7), 748–751.
Inzlicht, M., McKay, L., & Aronson, J. (2006). Stigma as ego-depletion: How being the target of prejudice affects self-control. Psychological Science, 17(3), 262–269. doi:10.1111/j.1467-9280.2006.01695.x.
Kassel, J. D., Wardle, M., & Roberts, J. E. (2007). Adult attachment security and college student substance use. Addictive Behaviors, 32(6), 1164–1176. doi:10.1016/j.addbeh.2006.08.005.
Kernis, M. H. (1995). Efficacy, agency, and self-esteem. New York, NY: Plenum Press.
Kimmel, S. B., & Mahalik, J. R. (2005). Body image concerns of gay men: The roles of minority stress and conformity to masculine norms. Journal of Consulting and Clinical Psychology, 73(6), 1185–1190. doi:10.1037/0022-006X.73.6.1185.
Klostermann, K., Kelley, M. L., Milletich, R. J., & Mignone, T. (2011). Alcoholism and partner aggression among gay and lesbian couples. Aggression and Violent Behavior, 16(2), 115–119. doi:10.1016/j.avb.2011.01.002.
Krueger, R. F., Watson, D., & Barlow, D. H. (2005). Introduction to the special section: Toward a dimensionally based taxonomy of psychopathology. Journal of Abnormal Psychology, 114(4), 491–493. doi:10.1037/0021-843X.114.4.491.
Kubicek, K., Beyer, W. J., Weiss, G., Iverson, E., & Kipke, M. D. (2010). In the dark: Young men’s stories of sexual initiation in the absence of relevant sexual health information. Health Education and Behavior, 37(2), 243–263. doi:10.1177/1090198109339993.
Lange, A. J., Jakubowski, P., & McGovern, T. V. (1976). Responsible assertive behavior: Cognitive/behavioral procedures for trainers. Champaign, IL: Research Press.
LaSala, M. C. (2000). Lesbians, gay men, and their parents: Family therapy for the coming-out crisis. Family Process, 39(1), 67–81. doi:10.1111/j.1545-5300.2000.39108.x.
Li, C. R., & Sinha, R. (2008). Inhibitory control and emotional stress regulation: Neuroimaging evidence for frontal-limbic dysfunction in psycho-stimulant addiction. Neuroscience and Biobehavioral Reviews, 32(3), 581–597. doi:10.1016/j.neubiorev.2007.10.003.
Lin, Y., & Israel, T. (2012). A computer-based intervention to reduce internalized heterosexism in men. Journal of Counseling Psychology, 59(3), 458–464. doi:10.1037/a0028282.
Linehan, M. M. (1993). Cognitive behavioral treatment of borderline personality disorder. New York, NY: Guilford Press.
MacKinnon, D. P. (2008). Introduction to statistical mediation analysis. New York, NY: Taylor & Francis Group/Lawrence Erlbaum Associates.
Major, B., & O’Brien, L. T. (2005). The social psychology of stigma. Annual Review of Psychology, 56, 393–421. doi:10.1146/annurev.psych.56.091103.070137.
Marlatt, G. A., & Donovan, D. M. (2005). Relapse prevention: Maintenance strategies in the treatment of addictive behaviors (2nd ed.). New York, NY: Guilford Press.
Martin, A. D., & Hetrick, E. S. (1988). The stigmatization of the gay and lesbian adolescent. Journal of Homosexuality, 15(1–2), 163–183. doi:10.1300/J082v15n01_12.
Marx, B. P., & Sloan, D. M. (2002). The role of emotion in the psychological functioning of adult survivors of childhood sexual abuse. Behavior Therapy, 33(4), 563–577. doi:10.1016/S0005-7894(02)80017-X.
Mays, V. M., & Cochran, S. D. (2001). Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health, 91(11), 1869–1876. doi:10.2105/AJPH.91.11.1869.
McKenry, P. C., Serovich, J. M., Mason, T. L., & Mosack, K. (2006). Perpetration of gay and lesbian partner violence: A disempowerment perspective. Journal of Family Violence, 21(4), 233–243. doi:10.1007/s10896-006-9020-8.
McLaughlin, K. A., Hatzenbuehler, M. L., & Hilt, L. M. (2009). Emotion dysregulation as a mechanism linking peer victimization to internalizing symptoms in adolescents. Journal of Consulting and Clinical Psychology, 77(5), 894–904. doi:10.1037/a0015760.
Mennin, D., & Farach, F. (2007). Emotion and evolving treatments for adult psychopathology. Clinical Psychology: Science and Practice, 14(4), 329–352. doi:10.1111/j.1468-2850.2007.00094.x.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. doi:10.1037/0033-2909.129.5.674.
Meyer, I. H., Schwartz, S., & Frost, D. M. (2008). Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Social Science and Medicine, 67, 368–379.
Michael, R. (1990). A preliminary investigation of alexithymia in men with psychoactive substance dependence. American Journal of Psychiatry, 147, 1228–1230.
Mineka, S., Watson, D., & Clark, L. A. (1998). Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology, 49, 377–412. doi:10.1146/annurev.psych.49.1.377.
Mineka, S., & Zinbarg, R. (2006). A contemporary learning theory perspective on the etiology of anxiety disorders: It’s not what you thought it was. American Psychologist, 61(1), 10–26. doi:10.1037/0003-066X.61.1.10.
Missildine, W., Feldstein, G., Punzalan, J. C., & Parsons, J. T. (2005). S/he loves me, s/he loves me not: Questioning heterosexist assumptions of gender differences for romantic and sexually motivated behaviors. Sexual Addiction and Compulsivity, 12(1), 65–74. doi:10.1080/10720160590933662.
Miyake, Y., Okamoto, Y., Onoda, K., Shirao, N., Okamoto, Y., Otagaki, Y., & Yamawaki, S. (2010). Neural processing of negative word stimuli concerning body image in patients with eating disorders: An fMRI study. Neuroimage, 50(3), 1333–1339. doi:10.1016/j.neuroimage.2009.12.095.
Mohr, J. J., & Fassinger, R. E. (2003). Self-acceptance and self-disclosure of sexual orientation in lesbian, gay, and bisexual adults: An attachment perspective. Journal of Counseling Psychology, 50(4), 482–495. doi:10.1037/0022-0167.50.4.482.
Muraven, M., & Baumeister, R. F. (2000). Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychological Bulletin, 126(2), 247–259. doi:10.1037/0033-2909.126.2.247.
Mustanski, B., Garofalo, R., Herrick, A., & Donenberg, G. (2007). Psychosocial health problems increase risk for HIV among urban young men who have sex with men: Preliminary evidence of a syndemic in need of attention. Annals of Behavioral Medicine, 34(1), 37–45.
Mustanski, B., Greene, G. J., Ryan, D., & Whitton, S. W. (2014). Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: The Queer Sex Ed intervention. Journal of Sex Research,. doi:10.1080/00224499.2013.867924.
National Institute of Mental Health (NIMH). (2008a). The National Institute of Mental Health Strategic Plan (NIH Publication No. 08-6368). Retrieved from http://www.nimh.nih.gov/about/strategic-planning-reports/index.shtml.
National Institute of Mental Health (NIMH). (2008b). The National Institute of Mental Health Strategic Plan (NIH Publication No. 08-6368). Retrieved July 9, 2014 from NIHM website: http://www.nimh.nih.gov/about/strategic-planning-reports/nimh-strategic-plan-2008.pdf.
National Institute of Mental Health. (2011). Research domain criteria (RDoC). Retrieved from http://www.nimh.nih.gov/research-priorities/rdoc/nimh-research-domain-criteria-rdoc.shtml.
Newcomb, M. E., & Mustanski, B. (2010). Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clinical Psychology Review, 30(8), 1019–1029. doi:10.1016/j.cpr.2010.07.003.
Nijm, J., & Jonasson, L. (2009). Inflammation and cortisol response in coronary artery disease. Annals of Medicine, 41(3), 224–233. doi:10.1080/07853890802508934.
Ostafin, B. D., & Marlatt, G. A. (2008). Surfing the urge: Experiential acceptance moderates the relation between automatic alcohol motivation and hazardous drinking. Journal of Social and Clinical Psychology, 27(4), 404–418. doi:10.1521/jscp.2008.27.4.404.
Pachankis, J. E. (2007). The psychological implications of concealing stigma: A cognitive- affective-behavioral model. Psychological Bulletin, 133(2), 328–345. doi:10.1037/0033-2909.133.2.328.
Pachankis, J. E. (2009). The use of cognitive-behavioral therapy to promote authenticity. Pragmatic Case Studies in Psychotherapy, 5(4), 28–38. doi:10.14713/pcsp.v5i4.997.
Pachankis, J. E. (2014). Uncovering clinical principles and techniques to address minority stress, mental health, and related health risks among gay and bisexual men. Clinical Psychology, 21, 313–330.
Pachankis, J. E., & Goldfried, M. R. (2006). Social anxiety in young gay men. Journal of Anxiety Disorders, 20, 996–1015. doi:10.1016/j.janxdis.2006.01.001.
Pachankis, J. E., & Goldfried, M. R. (2007a). An integrative, principle-based approach to psychotherapy. In S. G. Hofmann & J. Weinberger (Eds.), The art and science of psychotherapy (pp. 49–68). New York, NY: Routledge/Taylor & Francis Group.
Pachankis, J. E., & Goldfried, M. R. (2007b). On the next generation of process research. Clinical Psychology Review, 27(6), 760–768. doi:10.1016/j.cpr.2007.01.009.
Pachankis, J. E., Goldfried, M. R., & Ramrattan, M. E. (2008). Extension of the rejection sensitivity construct to the interpersonal functioning of gay men. Journal of Consulting and Clinical Psychology, 76(2), 306–317. doi:10.1037/0022-006X.76.2.306.
Pachankis, J. E., & Hatzenbuehler, M. L. (2013). The social development of contingent self-worth in sexual minority young men: An empirical investigation of the “Best Little Boy in the World” hypothesis. Basic and Applied Social Psychology, 35(2), 176–190. doi:10.1080/01973533.2013.764304.
Pachankis, J. E., Hatzenbuehler, M. L., Rendina, H. J., Safren, S. A., & Parsons, J. T. (2015). Cognitive behavior therapy for young adult gay and bisexual men’s mental health and related health risks: A randomized controlled trial of a transdiagnostic minority stress approach. Unpublished manuscript, Yale School of Public Health, Yale University, New Haven, CT.
Pachankis, J. E., Hatzenbuehler, M. L., Schmidt, A. J., Hickson, F., Weatherburn, P., Berg, R., & Marcus, U. (2014a). Hidden from health: Structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM Internet Survey (EMIS). Unpublished manuscript, Yale University.
Pachankis, J. E., Hatzenbuehler, M. L., & Starks, T. J. (2014b). The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Social Science and Medicine, 103, 67–75. doi:10.1016/j.socscimed.2013.10.005.
Pachankis, J. E., Lelutiu-Weinberger, C., Golub, S. A., & Parsons, J. T. (2013). The development of an online risk-reduction intervention for young gay and bisexual men using social networking technology. AIDS and Behavior, 17, 2986–2998.
Pachankis, J. E., Newcomb, M. E., Feinstein, B. A., & Bernstein, L. B. (2014c). Young gay and bisexual men’s stigma experiences and mental health: A five-year longitudinal study. Unpublished manuscript, Yale School of Public Health, Yale University, New Haven.
Pachankis, J. E., Rendina, H. J., Restar, A., Ventuneac, A., Grov, C., & Parsons, J. T. (in press). A minority stress-emotion regulation model of sexual compulsivity among highly sexually active gay and bisexual men. Health Psychology. doi:10.1037/hea0000180.
Pachankis, J. E., Westmaas, J. L., & Dougherty, L. R. (2011). The influence of sexual orientation and masculinity on young men’s tobacco smoking. Journal of Consulting and Clinical Psychology, 79(2), 142–152. doi:10.1037/a0022917.
Parsons, J. T., Grov, C., & Golub, S. A. (2012). Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: Further evidence of a syndemic. American Journal of Public Health, 10(1), 156–162. doi:10.2105/AJPH.2011.300284.
Parsons, J. T., Kelly, B. C., Bimbi, D. S., Muench, F., & Morgenstern, J. (2007). Accounting for the social triggers of sexual compulsivity. Journal of Addictive Diseases, 26(3), 5–16. doi:10.1300/J069v26n03_02.
Paul, J. P., Catania, J., Pollack, L., & Stall, R. (2001). Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: The Urban Men’s Health Study. Child Abuse and Neglect, 25(4), 557–584. doi:10.1016/S0145-2134(01)00226-5.
Plöderl, M., & Fartacek, R. (2005). Suicidality and associated risk factors among lesbian, gay, and bisexual compared to heterosexual Austrian adults. Suicide and Life-Threatening Behavior, 35(6), 661–670. doi:10.1521/suli.2005.35.6.661.
Ratti, R., Bakeman, R., & Peterson, J. L. (2000). Correlates of high-risk sexual behavior among Canadian men of South Asian and European origin who have sex with men. AIDS Care, 12(2), 193–202. doi:10.1080/09540120050001878.
Reid, R. C., Carpenter, B. N., Spackman, M., & Willes, D. L. (2008). Alexithymia, emotional instability, and vulnerability to stress proneness in patients seeking help for hypersexual behavior. Journal of Sex and Marital Therapy, 34(2), 133–149. doi:10.1080/00926230701636197.
Roemer, L., Orsillo, S. M., & Salters-Pedneault, K. (2008). Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: Evaluation in a randomized controlled trial. Journal of Consulting and Clinical Psychology, 76(6), 1083–1089. doi:10.1037/a0012720.
Rosario, M., Schrimshaw, E. W., & Hunter, J. (2009). Disclosure of sexual orientation and subsequent substance use and abuse among lesbian, gay, and bisexual youths: Critical role of disclosure reactions. Psychology of Addictive Behaviors, 23(1), 175–184. doi:10.1037/a0014284.
Russell, C. J., & Keel, P. K. (2002). Homosexuality as a specific risk factor for eating disorders in men. International Journal of Eating Disorders, 31(3), 300–306. doi:10.1002/eat.10036.
Russell, S. T., Ryan, C., Toomey, R. B., Diaz, R. M., & Sanchez, J. (2011). Lesbian, gay, bisexual, and transgender adolescent school victimization: Implications for young adult health and adjustment. The Journal of School Health, 81(5), 223–230. doi:10.1111/j.1746-1561.2011.00583.x.
Safren, S. A., Blashill, A., & O’Cleirigh, C. (2011). Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS and Behavior, 15, S30–S34.
Safren, S. A., & Heimberg, R. G. (1999). Depression, hopelessness, suicidality, and related factors in sexual minority and heterosexual adolescents. Journal of Consulting and Clinical Psychology, 67(6), 859–866. doi:10.1037/0022-006X.67.6.859.
Safren, S. A., Reisner, S. A., Herrick, A., Mimiaga, M. J., & Stall, R. (2010). Mental health and HIV risk in men who have sex with men. Journal of AIDS, 55, S74–S77.
Sanislow, C. A., Pine, D. S., Quinn, K. J., Kozak, M. J., Garvey, M. A., … Cuthbert, B. N. (2010). Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology, 119(4), 631–639. doi:10.1037/a0020909.
Sherry, A. (2007). Internalized homophobia and adult attachment: Implications for clinical practice. Psychotherapy, 44(2), 219–225. doi:10.1037/0033-3204.44.2.219.
Shin, L. M., & Liberzon, I. (2010). The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology, 35(1), 169–191. doi:10.1038/npp.2009.83.
Siegel, S., & Lowe, E. (1994). Uncharted lives: Understanding the life passages of gay men. New York, NY: Plume.
Sikkema, K. J., Kochman, A., DiFranceisco, W., Kelly, J. A., & Hoffmann, R. G. (2003). AIDS- related grief and coping with loss among HIV-positive men and women. Journal of Behavioral Medicine, 26(2), 165–181. doi:10.1023/A:1023086723137.
Singer, M. C., Erickson, P. I., Badiane, L., Diaz, R., Ortiz, D., … Nicolaysen, A. M. (2006). Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Social Science and Medicine, 63(8), 2010–2021. doi:10.1016/j.socscimed.2006.05.012.
Sinha, R. (2008). Chronic stress, drug use, and vulnerability to addiction. In G. R. Uhl (Ed.), Addiction reviews 2008 (pp. 105–130). Malden: Blackwell Publishing.
Slavich, G. M., Way, B. M., Eisenberger, N. I., & Taylor, S. E. (2010). Neural sensitivity to social rejection is associated with inflammatory responses to social stress. PNAS Proceedings of the National Academy of Sciences of the United States, 107(33), 14917–14927. doi:10.1073/pnas.1009164107.
Stall, R., Friedman, M., & Catania, J. A. (2008). Interacting epidemics and gay men’s health: a theory of syndemic production among urban gay men. In R. J. Wolitski, R. Stall, & R. O. Valdiserri (Eds.), Unequal opportunity: Health disparities affecting gay and bisexual men in the United States (pp. 251–274). New York, NY: Oxford University Press.
Stall, R., & Purcell, D. W. (2000). Intertwining epidemics: A review of research on substance use among men who have sex with men and its connection to the AIDS epidemic. AIDS and Behavior, 4(2), 181–192. doi:10.1023/A:1009516608672.
Stapinski, L. A., Abbott, M. J., & Rapee, R. M. (2010). Evaluating the cognitive avoidance model of generalized anxiety disorder: Impact of worry on threat appraisal, perceived control and anxious arousal. Behaviour Research and Therapy, 48(10), 1032–1040. doi:10.1016/j.brat.2010.07.005.
Strauman, T. J. (2002). Self-regulation and depression. Self and Identity, 1(2), 151–157. doi:10.1080/152988602317319339.
Taywaditep, K. J. (2001). Marginalization among the marginalized: Gay men’s anti-effeminacy attitudes. Journal of Homosexuality, 42(1), 1–28. doi:10.1300/J082v42n01_01.
Teicher, M. H., Andersen, S. L., Polcari, A., Anderson, C. M., Navalta, C. P., & Kim, D. M. (2003). The neurobiological consequences of early stress and childhood maltreatment. Neuroscience and Biobehavioral Reviews, 27(1), 33–44. doi:10.1016/S0149-7634(03)00007-1.
Tharinger, D., & Wells, G. (2000). An attachment perspective on the developmental challenges of gay and lesbian adolescents: The needs for continuity of caregiving from family and schools. School Psychology Review, 29(2), 158–172.
Tilcsik, A. (2011). Pride and prejudice: Employment discrimination against openly gay men in the United States. American Journal of Sociology, 117(2), 586–626. doi:10.1086/661653.
Tjaden, P., Thoennes, N., & Allison, C. J. (1999). Comparing violence over the life span in samples of same-sex and opposite-sex cohabitants. Violence and Victims, 14(4), 413–425.
Trapence, G., Collins, C., Avrett, S., Carr, R., Sanchez, H., Ayala, G., … Baral, S. D. (2012). From personal survival to public health: Community leadership by men who have sex with men in the response to HIV. Lancet, 380(9839), 400–410. doi:10.1016/S0140-6736(12)60834-4.
Walkup, J., Blank, M. B., Gonzalez, J. S., Safren, S., Schwartz, R., Brown, L., … Schumacher, J. E. (2008). The impact of mental health and substance abuse factors on HIV prevention and treatment. JAIDS Journal of Acquired Immune Deficiency Syndromes, 47, S15–S19. doi:10.1097/QAI.0b013e3181605b26.
Ward, A., Ramsay, R., & Treasure, J. (2000). Attachment research in eating disorders. British Journal of Medical Psychology, 73(1), 35–51. doi:10.1348/000711200160282.
Webb, T. L., Miles, E., & Sheeran, P. (2012). Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychological Bulletin, 138(4), 775–808. doi:10.1037/a0027600.
Weeks, J., Heaphy, B., & Donovan, C. (2001). Same sex intimacies: Families of choice and other life experiments. London: Routledge.
West, C. M. (2012). Partner abuse in ethnic minority and gay, lesbian, bisexual, and transgender populations. Partner Abuse, 3(3), 336–357. doi:10.1891/1946-6560.3.3.336.
Westen, D., Novotny, C. M., & Thompson-Brenner, H. (2004). The empirical status of empirically supported therapies: Assumptions, findings, and reporting in controlled clinical trials. Psychological Bulletin, 130(4), 631–663. doi:10.1037/0033-2909.130.4.631.
Wilamowska, Z. A., Thompson-Hollands, J., Fairholme, C. P., Ellard, K. K., Farchione, T. J., & Barlow, D. H. (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety, 27(10), 882–890. doi:10.1002/da.20735.
Williams, J. L., & Lierle, D. M. (1986). Effects of stress controllability, immunization, and therapy on the subsequent defeat of colony intruders. Animal Learning and Behavior, 14(3), 305–314. doi:10.3758/BF03200072.
Wilson, W. J. (2010). Why both social structure and culture matter in a holistic analysis of inner-city poverty. Annals of the American Academy of Political and Social Science, 629(1), 200–219. doi:10.1177/0002716209357403.
Wilton, L. (2009). A preliminary study of body image and HIV sexual risk behavior in black gay and bisexual men: Implications for HIV prevention. Journal of Gay and Lesbian Social Services, 21(4), 309–325. doi:10.1080/10538720802497829.
Winters, J., Clift, R. J., & Dutton, D. G. (2004). An exploratory study of emotional intelligence and domestic abuse. Journal of Family Violence, 19(5), 255–267. doi:10.1023/B:JOFV.0000042076.21723.f3.
World Health Organization. (2006). Defining sexual health. Report of a technical consultation on sexual health, January 2002. Geneva: World Health Organization.
Yehuda, R., Bierer, L. M., Schmeidler, J., Aferiat, D. H., Breslau, I., & Dolan, S. (2000). Low cortisol and risk for PTSD in adult offspring of Holocaust survivors. American Journal of Psychiatry, 157(8), 1252–1259. doi:10.1176/appi.ajp.157.8.1252.
Yi, H., Sandfort, T. G., & Shidlo, A. (2010). Effects of disengagement coping with HIV risk on unprotected sex among HIV-negative gay men in New York City. Health Psychology, 29(2), 205–214. doi:10.1037/a0017786.
Zakalik, R. A., & Wei, M. (2006). Adult attachment, perceived discrimination based on sexual orientation, and depression in gay males: Examining the mediation and moderation effects. Journal of Counseling Psychology, 53(3), 302–313. doi:10.1037/0022-0167.53.3.302.
Zamboni, B. D., & Crawford, I. (2007). Minority stress and sexual problems among African- American gay and bisexual men. Archives of Sexual Behavior, 36(4), 569–578. doi:10.1007/s10508-006-9081-z.
Zapf, J. L., Greiner, J., & Carroll, J. (2008). Attachment styles and male sex addiction. Sexual Addiction and Compulsivity, 15(2), 158–175. doi:10.1080/10720160802035832.
Acknowledgments
The preparation of this article was supported by a research grant from the National Institute of Mental Health (R34-MH096607; John E. Pachankis, Principal Investigator). The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pachankis, J.E. A Transdiagnostic Minority Stress Treatment Approach for Gay and Bisexual Men’s Syndemic Health Conditions. Arch Sex Behav 44, 1843–1860 (2015). https://doi.org/10.1007/s10508-015-0480-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-015-0480-x