Abstract
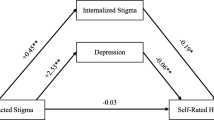
This study examined the demographic and clinical correlates of HIV stigma and evaluated how HIV stigma was associated with physical and mental health outcomes one year later in a primary-care based cohort of persons living with HIV (PLHIV; N = 584). HIV stigma was measured using a modified Berger HIV stigma scale, which includes four subscales: (1) personalized stigma; (2) disclosure concerns; (3) negative self-image; and (4) concerns around public attitudes towards PLHIV. Physical and mental health were assessed using the 12-item short form survey (SF-12). Compared to whites, African Americans were more likely to have higher personalized stigma scores (adjusted prevalence ratio [aPR] 1.54 [95% confidence interval 1.10–2.15]), disclosure concerns (aPR 1.40 [1.03–1.92]), and concerns with public attitudes about PLHIV (aPR 1.61 [1.11–2.34]). Hispanic/Latinx participants were more likely to have concerns around public attitudes towards PLHIV (aPR 1.50 [1.11–2.02]) than whites. Compared to men, women were more likely to have higher negative self-image scores (aPR 1.50 [1.08–2.08]). Higher stigma scores were associated with poorer subsequent self-reported physical and mental health functional status. Our findings highlight the substantial need for addressing HIV stigma, particularly among minority subgroups.
Resumen
El objetivo de este estudio era examinar la correlación del estigma del VIH con aspectos demográficos y clínicos. Se buscaba evaluar la asociación del estigma del VIH con los efectos de la salud física y mental luego de un año en un cohorte de personas viviendo con VIH (PVV; N = 584) provenientes de una clínica de servicios primarios. El estigma del VIH se midió utilizando la escala modificada de estigma del VIH de Berger que incluye cuatro sub-escalas: (1) estigma personalizado; (2) preocupaciones por revelación de diagnóstico; (3) auto-imagen negativa; y (4) preocupaciones acerca de actitudes hacia PVV. La salud física y mental fue evaluada utilizando una encuesta corta de 12 ítems. En comparación con las personas blancas, entre las personas Afroamericanas había más probabilidad de obtener una mayor puntuación en las escalas de estigma personalizado (razón de prevalencia ajustada [aRP] 1.54 [95% intervalo de confianza 1.10–2.15]), preocupaciones por revelación de diagnóstico (aRP 1.40 [1.03–1.92]), y preocupacionespor actitudes negativas hacia PVV (aRP 1.61 [1.11–2.34]). Participantes Hispanos/Latinos tenían más probabilidad de tener preocupaciones por las actitudes negativas hacia PVV (aRP 1.50 [1.11–2.02]) en comparación con personas blancas. En comparación con los hombres, las mujeres tenían mayor probabilidad de tener un resultado más alto en la escala de auto-imagen negativa (aRP 1.50 [1.08–2.08]). Resultados mayores estuvieron asociados a estatus más pobres de funcionalidad de salud física y mental. Nuestros resultados destacan la necesidad substancial de atender asuntos de estigma por el VIH, particularmente en grupos minoritarios.

Similar content being viewed by others
References
Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–21. https://doi.org/10.2105/AJPH.2012.301069.
Link BG, Phelan JC. Conceptualizing stigma. Ann Rev Sociol. 2001;27:363–85. https://doi.org/10.1146/annurev.soc.27.1.363.
Golub SA, Gamarel KE. The impact of anticipated HIV stigma on delays in HIV testing behaviors: findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care STDS. 2013;27(11):621–7.
Gamarel KE, Nelson KM, Stephenson R, Santiago Rivera OJ, Chiaramonte D, Miller RL, et al. Anticipated HIV stigma and delays in regular HIV testing behaviors among sexually-active young gay, bisexual, and other men who have sex with men and transgender women. AIDS Behav. 2018;22(2):522–30. https://doi.org/10.1007/s10461-017-2005-1.
Naar-King S, Bradford J, Coleman S, Green-Jones M, Cabral H, Tobias C. Retention in care of persons newly diagnosed with HIV: outcomes of the Outreach Initiative. AIDS Patient Care STDS. 2007;21(s1):S40–S4848.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640. https://doi.org/10.7448/IAS.16.3.18640.
Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6(7):e011453. https://doi.org/10.1136/bmjopen-2016-011453.
Wolitski RJ, Pals SL, Kidder DP, Courtenay-Quirk C, Holtgrave DR. The effects of HIV stigma on health, disclosure of HIV status, and risk behavior of homeless and unstably housed persons living with HIV. AIDS Behav. 2009;13(6):1222–32.
Edelman EJ, Cole CA, Richardson W, Boshnack N, Jenkins H, Rosenthal MS. Stigma, substance use and sexual risk behaviors among HIV-infected men who have sex with men: a qualitative study. Prev Med Rep. 2016;3:296–302. https://doi.org/10.1016/j.pmedr.2016.03.012.
Stuber J, Meyer I, Link B. Stigma, prejudice, discrimination and health. Soc Sci Med. 2008;67(3):351–7. https://doi.org/10.1016/j.socscimed.2008.03.023.
Grossman CI, Stangl AL. Editorial: global action to reduce HIV stigma and discrimination. J Int AIDS Soc. 2013;16(3 Suppl 2):18881. https://doi.org/10.7448/IAS.16.3.18881.
International Association of Providers of AIDS Care. Fast track Cities. https://www.fast-trackcities.org/.
San Francisco Department of Public Health. HIV epidemiology annual report 2018. 2019 Sep. https://www.sfdph.org/dph/files/reports/RptsHIVAIDS/HIV-Epidemiology-Annual-Report-2018.pdf.
Beltran S, Chen Y-H, Miller D, Ick T, Lin J, Packer T, et al. Will we get to zero HIV stigma in San Francisco? AIDS Behav. 2019;6(7):1–3.
Christopoulos KA, Neilands TB, Hartogensis W, Geng EH, Sauceda J, Mugavero MJ, et al. Internalized HIV stigma is associated with concurrent viremia and poor retention in a cohort of US patients in HIV care. J Acquir Immune Defic Syndr. 2019;82(2):116–23.
Saitz R. Clinical practice. Unhealthy alcohol use. N Engl J Med. 2005;352(6):596–607.
Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;320(18):1899–909.
Williams EC, Hahn JA, Saitz R, Bryant K, Lira MC, Samet JH. Alcohol use and human immunodeficiency virus (HIV) infection: current knowledge, implications, and future directions. Alcohol Clin Exp Res. 2016;40(10):2056–72. https://doi.org/10.1111/acer.13204.
Williams EC, McGinnis KA, Bobb JF, Rubinsky AD, Lapham GT, Skanderson M, et al. Changes in alcohol use associated with changes in HIV disease severity over time: a national longitudinal study in the Veterans Aging Cohort. Drug Alcohol Depend. 2018;189:21–9.
Satre DD, Sarovar V, Leyden W, Hare CB, Catz SL, Bryant KJ, et al. Changes in days of unhealthy alcohol use and antiretroviral therapy adherence, HIV RNA levels, and condomless sex: a secondary analysis of clinical trial data. AIDS Behav. 2020;24:1784–92. https://doi.org/10.1007/s10461-019-02742-y.
Satre DD, Leibowitz AS, Leyden W, Catz SL, Hare CB, Jang HJ, et al. Interventions to reduce unhealthy alcohol use among primary care patients with HIV: the Health and Motivation randomized clinical trial. J Gen Intern Med. 2019;34:2054–61. https://doi.org/10.1007/s11606-019-05065-9.
Silverberg MJ, Leyden WA, Leibowitz A, Hare CB, Jang HJ, Sterling S, et al. Factors associated with hazardous alcohol use and motivation to reduce drinking among HIV primary care patients: baseline findings from the Health & Motivation study. Addict Behav. 2018;84:110–7. https://doi.org/10.1016/j.addbeh.2018.03.033.
Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–29.
Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. J Adolesc Health. 2007;40(1):96–8.
Delate T, Coons SJ. The discriminative ability of the 12-item short form health survey (SF-12) in a sample of persons infected with HIV. Clin Ther. 2000;22(9):1112–20.
Aden B, Dunning A, Nosyk B, Wittenberg E, Bray JW, Schackman BR. Impact of illicit drug use on health-related quality of life in opioid-dependent patients undergoing HIV treatment. J Acquir Immune Defic Syndr. 2015;70(3):304–10. https://doi.org/10.1097/QAI.0000000000000768.
Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Ware JEJ, Kosinski MA, Keller SD. SF-12: how to Score the SF-12 Physical and Mental Health Summary Scales. 2nd ed. The Health Institute, New England Medical Center; 1995 Dec 1. https://www.researchgate.net/publication/242636950_SF-12_How_to_Score_the_SF-12_Physical_and_Mental_Health_Summary_Scales.
World Health Organization. AUDIT: the Alcohol Use Disorders Identification Test guidelines for use in primary health care. Geneva: World Health Organization; 2001. https://apps.who.int/iris/handle/10665/67205.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68(4):225–36. https://doi.org/10.1037/a0032705.
Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Longitudinal relationships between antiretroviral treatment adherence and discrimination due to HIV-serostatus, race, and sexual orientation among African-American men with HIV. Ann Behav Med. 2010;40(2):184–90. https://doi.org/10.1007/s12160-010-9200-x/.
Rendina HJ, Golub SA, Grov C, Parsons JT. Stigma and sexual compulsivity in a community-based sample of HIV-positive gay and bisexual men. AIDS Behav. 2012;16(3):741–50.
Hatzenbuehler ML, O'Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Ann Behav Med. 2011;42(2):227–34.
Crockett KB, Kalichman SC, Kalichman MO, Cruess DG, Katner HP. Experiences of HIV-related discrimination and consequences for internalised stigma, depression and alcohol use. Psychol Health. 2019;34(7):796–810.
Lunze K, Lioznov D, Cheng DM, Nikitin RV, Coleman SM, Bridden C, et al. HIV stigma and unhealthy alcohol use among people living with HIV in Russia. AIDS Behav. 2017;21(9):2609–17.
Wray TB, Pantalone DW, Kahler CW, Monti PM, Mayer KH. The role of discrimination in alcohol-related problems in samples of heavy drinking HIV-negative and positive men who have sex with men (MSM). Drug Alcohol Depend. 2016;166:226–34.
Wardell JD, Shuper PA, Rourke SB, Hendershot CS. Stigma, coping, and alcohol use severity among people living with HIV: a prospective analysis of bidirectional and mediated associations. Ann Behav Med. 2018;52(9):762–72.
Degroote S, Vogelaers D, Vandijck DM. What determines health-related quality of life among people living with HIV: an updated review of the literature. Arch Public Health. 2014;72(1):40–10.
Logie CH, Wang Y, Lacombe-Duncan A, Wagner AC, Kaida A, Conway T, et al. HIV-related stigma, racial discrimination, and gender discrimination: pathways to physical and mental health-related quality of life among a national cohort of women living with HIV. Prev Med. 2018;107:36–44.
Jackson-Best F, Edwards N. Stigma and intersectionality: a systematic review of systematic reviews across HIV/AIDS, mental illness, and physical disability. BMC Public Health. 2018;18(1):919. https://doi.org/10.1186/s12889-018-5861-3.
Cole ER. Intersectionality and research in psychology. Am Psychol. 2009;64(3):170–80.
Sipe TA, Barham TL, Johnson WD, Joseph HA, Tungol-Ashmon ML, O'Leary A. structural interventions in HIV prevention: a taxonomy and descriptive review. AIDS Behav. 2017;21(12):3366–430. https://doi.org/10.1007/s10461-017-1965-5.
Ma PHX, Chan ZCY, Loke AY. Self-stigma reduction interventions for people living with HIV/AIDS and their families: a systematic review. AIDS Behav. 2019;23(3):707–41. https://doi.org/10.1007/s10461-018-2304-1.
Kerrigan D, Kennedy CE, Morgan-Thomas R, Reza-Paul S, Mwangi P, Win KT, et al. A community empowerment approach to the HIV response among sex workers: effectiveness, challenges, and considerations for implementation and scale-up. Lancet. 2015;385(9963):172–85. https://doi.org/10.1016/S0140-6736(14)60973-9.
Clement S, Lassman F, Barley E, Evans-Lacko S, Williams P, Yamaguchi S, et al. Mass media interventions for reducing mental health-related stigma. Cochrane Databases Syst Rev. 2013;46(7):CD009453. https://doi.org/10.1002/14651858.CD009453.pub2.
Kerr JC, Valois RF, DiClemente RJ, Carey MP, Stanton B, Romer D, et al. The effects of a mass media HIV-risk reduction strategy on HIV-related stigma and knowledge among African American adolescents. AIDS Patient Care STDS. 2015;29(3):150–6. https://doi.org/10.1089/apc.2014.0207.
Acknowledgements
This study was supported by the National Institute on Alcohol Abuse and Alcoholism (U01 AA021997 and K24 AA025703), the National Institute on Drug Abuse (T32 DA007250), and the National Institute of Mental Health (T32 MH19105).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hojilla, J.C., Santiago-Rodriguez, E.I., Sterling, S. et al. HIV Stigma and Its Associations with Longitudinal Health Outcomes Among Persons Living with HIV with a History of Unhealthy Alcohol Use. AIDS Behav 25, 215–224 (2021). https://doi.org/10.1007/s10461-020-02963-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-02963-6