Abstract
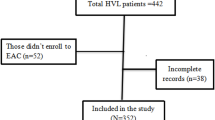
Antiretroviral therapy (ART) is efficacious in improving clinical outcomes among people living with HIV (PLWH) and reducing HIV transmission when taken regularly. Research examining modifiable factors associated with ART non-adherence is critical for informing novel intervention development in settings with high HIV prevalence. Alcohol use has been linked with ART non-adherence in studies in sub-Saharan Africa; however, no review has pooled estimates across studies. We reviewed studies of alcohol use and ART non-adherence conducted in sub-Saharan Africa. We searched PubMed, CINAHL, EMBASE, and PsycINFO through August 2019 with terms related to ART non-adherence, alcohol use, and sub-Saharan Africa. One author reviewed titles/abstracts (n = 754) and two authors reviewed full texts (n = 308) for inclusion. Discrepancies were resolved by group consensus. Studies were retained if they quantitatively measured associations between alcohol use and ART non-adherence or viral non-suppression. We defined ART non-adherence using the definitions from each parent study (e.g., patients with > 5% missed ART doses during the previous four, seven or 30 days were considered non-adherent). A random effects meta-analysis was conducted to pool associations and we conducted additional analyses to assess between-study heterogeneity and publication bias and sensitivity analyses to determine robustness of our results when considering only certain study designs, alcohol use or ART scales, or studies that used viral non-suppression as their primary outcome. Of 56 articles meeting our inclusion criteria, 32 articles were included in the meta-analysis. All studies measured alcohol use via self-report. ART non-adherence was assessed using self-report, pill counts, or pharmacy records and definition of non-adherence varied depending on the measure used. Individuals who used alcohol had twice the odds of ART non-adherence compared with those who did not use alcohol (34% non-adherence among alcohol users vs. 18% among non-users; pooled odds ratio: 2.25; 95% confidence interval: 1.87–2.69; p < 0.001). We found evidence of a high degree of heterogeneity between studies (Cochrane Q statistic: 382.84, p< 0.001; I2 proportion: 91.9%) and evidence of publication bias. However, the magnitude of our pooled odds ratio was consistent across a number of sensitivity analyses to account for heterogeneity and publication bias. In a secondary analysis with studies using viral non-suppression as their primary outcome, we also estimated a statistically significant pooled effect of alcohol use on viral non-suppression (pooled odds ratio: 2.47; 95% confidence interval: 1.58–3.87). Evidence suggests alcohol use is associated with ART non-adherence in Sub-Saharan Africa, potentially hindering achievement of the UNAIDS 90-90-90 HIV treatment targets.


Similar content being viewed by others
References
Joint United Nations Programme on HIV/AIDS (2014) UNAIDS report on the global AIDS epidemic 2013. UNAIDS, Geneva
Joint United Nations Programme on HIV/AIDS (2014) Fast track: ending the AIDS epidemic by 2030. UNAIDS, Geneva. Available from: http://www.unaids.org/sites/default/files/media_asset/JC2686_WAD2014report_en.pdf
Joint United Nations Programme on HIV/AIDS (2014) 90-90-90: an ambitious treatment target to help end the AIDS epidemic. UNAIDS, Geneva
Baggaley R, Dalal S, Johnson C, et al. Beyond the 90-90-90: refocusing HIV prevention as part of the global HIV response. J Int AIDS Soc. 2016;19(1):21348.
Langebeek N, Gisolf EH, Reiss P, Vervoort SC, Hafsteinsdóttir TB, Richter C, et al. Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Med. 2014;12:142.
Shubber Z, Mills EJ, Nachega JB, et al. Patient-reported barriers to adherence to antiretroviral therapy: a systematic review and meta-analysis. PLoS Med. 2016;13(11):e1002183.
Hudelson C, Cluver L. Factors associated with adherence to antiretroviral therapy among adolescents living with HIV/AIDS in low- and middle-income countries: a systematic review. AIDS Care. 2015;27(7):805–16.
Hahn JA, Woolf-King SE, Muyindike W. Adding fuel to the fire: alcohol’s effect on the HIV epidemic in Sub-Saharan Africa. Curr HIV/AIDS Rep. 2011;8(3):172–80.
Nakimuli-Mpungu E, Bass JK, Alexandre P, et al. Depression, alcohol use and adherence to antiretroviral therapy in sub-Saharan Africa: a systematic review. AIDS Behav. 2012;16(8):2101–18.
Heestermans T, Browne JL, Aitken SC, Vervoort SC, Klipstein-Grobusch K. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: a systematic review. BMJ Glob Health. 2016;1(4):e000125.
Kalichman SC, Grebler T, Amaral CM, et al. Viral suppression and antiretroviral medication adherence among alcohol using HIV-positive adults. Int J Behav Med. 2014;21(5):811–20.
Braithwaite RS, Conigliaro J, McGinnis KA, Maisto SA, Bryant K, Justice AC. Adjusting alcohol quantity for mean consumption and intoxication threshold improves prediction of nonadherence in HIV patients and HIV-negative controls. Alcohol Clin Exp Res. 2008;32(9):1645–51.
Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52(2):180–202.
Cook RL, Zhou Z, Kelso-Chichetto NE, et al. Alcohol consumption patterns and HIV viral suppression among persons receiving HIV care in Florida: an observational study. Addict Sci Clin Pract. 2017;12(1):22.
Barai N, Monroe A, Lesko C, et al. The association between changes in alcohol use and changes in antiretroviral therapy adherence and viral suppression among women living with HIV. AIDS Behav. 2017;21(7):1836–45.
Rehm J, Parry CD. Alcohol consumption and infectious diseases in South Africa. Lancet. 2009;374(9707):2053.
Neuman MG, Schneider M, Nanau RM, Parry C. Alcohol consumption, progression of disease and other comorbidities, and responses to antiretroviral medication in people living with HIV. AIDS Res Treat. 2012;2012:751827.
Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112(3):178–93.
Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS: a systematic review. Alcohol. 2010;45(2):159–66.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Adeniyi O, Ajayi A, Ter GD, Owolabi EO, Eboh A, Lambert J. Factors affecting adherence to antiretroviral therapy among pregnant women in the Eastern Cape, South Africa. BMC Infect Dis. 2018;18(1):175.
Alemu H, Haile Mariam D, Tsui AO, Shewamare A. Correlates of highly active antiretroviral therapy adherence among urban Ethiopian clients. Afr J AIDS Res AJAR. 2011;10(3):263–70.
Beyene KA, Gedif T, Gebre-Mariam T, Engidawork E. Highly active antiretroviral therapy adherence and its determinants in selected hospitals from south and central Ethiopia. Pharmacoepidemiol Drug Saf. 2009;18(11):1007–15.
Bezabhe WM, Chalmers L, Bereznicki LR, Gee P, Peterson GM. Antiretroviral adherence and treatment outcomes among adult Ethiopian patients. AIDS Care. 2016;28(8):1018–22.
Boyer S, Clerc I, Bonono C-R, Marcellin F, Bilé P-C, Ventelou B. Non-adherence to antiretroviral treatment and unplanned treatment interruption among people living with HIV/AIDS in Cameroon: individual and healthcare supply-related factors. Soc Sci Med. 2011;72(8):1383–92.
Bultum JA, Yigzaw N, Demeke W, Alemayehu M. Alcohol use disorder and associated factors among human immunodeficiency virus infected patients attending antiretroviral therapy clinic at Bishoftu General Hospital, Oromiya region, Ethiopia. PLoS ONE. 2018;13(3):e0189312.
Cagle A, McGrath C, Richardson BA, et al. Alcohol use and immune reconstitution among HIV-infected patients on antiretroviral therapy in Nairobi, Kenya. AIDS Care. 2017;29(9):1192–7.
Cerutti B, Broers B, Masetsibi M, et al. Alcohol use and depression: link with adherence and viral suppression in adult patients on antiretroviral therapy in rural Lesotho, Southern Africa: a cross-sectional study. BMC Public Health. 2016;16:947.
Cichowitz C, Maraba N, Hamilton R, Charalambous S, Hoffmann CJ. Depression and alcohol use disorder at antiretroviral therapy initiation led to disengagement from care in South Africa. PLoS ONE. 2017;12(12):e0189820.
Dahab M, Charalambous S, Karstaedt AS, et al. Contrasting predictors of poor antiretroviral therapy outcomes in two South African HIV programmes: a cohort study. BMC Public Health. 2010;10:430.
Denison JA, Koole O, Tsui S, et al. Incomplete adherence among treatment-experienced adults on antiretroviral therapy in Tanzania, Uganda and Zambia. AIDS. 2015;29(3):361–71.
Do NT, Phiri K, Bussmann H, Gaolathe T, Marlink RG, Wester CW. Psychosocial factors affecting medication adherence among HIV-1 infected adults receiving combination antiretroviral therapy (cART) in Botswana. AIDS Res Hum Retrovir. 2010;26(6):685–91.
Elul B, Basinga P, Nuwagaba-Biribonwoha H, et al. High levels of adherence and viral suppression in a nationally representative sample of HIV-infected adults on antiretroviral therapy for 6, 12 and 18 months in Rwanda. PloS ONE. 2013;8(1):e53586.
Etienne M, Hossain M, Redfield R, Stafford K, Amoroso A. indicators of adherence to antiretroviral therapy treatment among HIV/AIDS patients in 5 African countries. J Int Assoc Phys AIDS Care JIAPAC. 2010;9(2):98–103.
Falang KD, Akubaka P, Jimam NS. Patient factors impacting antiretroviral drug adherence in a Nigerian tertiary hospital. J Pharmacol Pharmacother. 2012;3(2):138–42.
Farley J, Miller E, Zamani A, et al. Screening for hazardous alcohol use and depressive symptomatology among HIV-infected patients in Nigeria: prevalence, predictors, and association with adherence. J Int Assoc Phys AIDS Care. 2010;9(4):218–26.
Fatch R, Emenyonu NI, Muyindike W, Kekibiina A, Woolf-King S, Hahn JA. Alcohol Interactive toxicity beliefs and ART non-adherence among HIV-infected current drinkers in Mbarara, Uganda. AIDS Behav. 2017;21(7):1812–24.
Goar SG, Audu MD, Agbir MT, Matawal B. Substance abuse and adherence to antiretroviral therapy among patients attending clinic at a specialist hospital in Jos, Nigeria. Afr J Drug Alcohol Stud. 2015;14(1):37–47.
Gross R, Bellamy SL, Ratshaa B, et al. Effects of sex and alcohol use on antiretroviral therapy outcomes in Botswana: a cohort study. Addiction. 2017;112(1):73–81.
Guira O, Kaboré DSR, Dao G, et al. The modalities of nonadherence to highly active antiretroviral therapy and the associated factors related to patients’ sociodemographic characteristics and their caregiving perceptions in Ouagadougou (Burkina Faso). J Int Assoc Provid AIDS Care. 2016;15(3):256–60.
Haberer JE, Bwana BM, Orrell C, et al. ART adherence and viral suppression are high among most non-pregnant individuals with early-stage, asymptomatic HIV infection: an observational study from Uganda and South Africa. J Int AIDS Soc. 2019;22(2):e25232.
Hicham T, Ilyas E, Tarik H, et al. Risk factors associated with unsuppressed viral load in HIV-1 infected patients at the first antiretroviral therapy in Morocco. Int J Mycobacteriol. 2019;8(2):113–7.
Idindil B, Jullu B, Mugusi F, Tanner M. A case-control study of factors associated with non-adherent to antiretroviral therapy among HIV infected people in Pwani Region, eastern Tanzania. Tanzan J Health Res. 2012;14(3):194–203.
Jaquet A, Ekouevi DK, Bashi J, et al. Alcohol use and non-adherence to antiretroviral therapy in HIV-infected patients in West Africa. Addiction. 2010;105(8):1416–21.
Kader R, Govender R, Seedat S, Koch JR, Parry C. Understanding the impact of hazardous and harmful use of alcohol and/or other drugs on ARV adherence and disease progression. PloS ONE. 2015;10(5):e0125088.
Kalichman S, Mathews C, Banas E, Kalichman M. Alcohol-related intentional nonadherence to antiretroviral therapy among people living with HIV, Cape Town, South Africa. AIDS Care. 2019;31(8):951–7.
Kalichman S, Mathews C, Banas E, Kalichman M. Treatment adherence in HIV stigmatized environments in South Africa: stigma avoidance and medication management. Int J STD AIDS. 2018;30(4):362–70.
Kazooba P, Mayanja BN, Levin J, Masiira B, Kaleebu P. Virological failure on first-line antiretroviral therapy; associated factors and a pragmatic approach for switching to second line therapy-evidence from a prospective cohort study in rural South-Western Uganda, 2004–2011. Pan Afr Med J. 2018;29:191.
Kekwaletswe CT, Jordaan E, Nkosi S, Morojele NK. Social support and the mediating roles of alcohol use and adherence self-efficacy on antiretroviral therapy (ART) adherence among ART recipients in Gauteng, South Africa. AIDS Behav. 2017;21(7):1846–56.
Kekwaletswe CT, Morojele NK. Patterns and predictors of antiretroviral therapy use among alcohol drinkers at HIV clinics in Tshwane, South Africa. AIDS Care. 2014;26(Suppl 1):S78–82.
Lancaster KE, Lungu T, Mmodzi P, et al. The association between substance use and sub-optimal HIV treatment engagement among HIV-infected female sex workers in Lilongwe, Malawi. AIDS Care. 2017;29(2):197–203.
Lyimo RA, Stutterheim SE, Hospers HJ, de Glee T, van der Ven A, de Bruin M. Stigma, disclosure, coping, and medication adherence among people living with HIV/AIDS in Northern Tanzania. AIDS Patient Care STDs. 2014;28(2):98–105.
Magidson JF, Saal W, Nel A, Remmert JE, Kagee A. Relationship between depressive symptoms, alcohol use, and antiretroviral therapy adherence among HIV-infected, clinic-attending patients in South Africa. J Health Psychol. 2017;22(11):1426–33.
Marcellin F, Boyer S, Protopopescu C, et al. Determinants of unplanned antiretroviral treatment interruptions among people living with HIV in Yaoundé, Cameroon (EVAL survey, ANRS 12-116). Trop Med Int Health. 2008;13(12):1470–8.
Méda ZC, Lin YT, Sombié I, Maré D, Morisky DE, Chen YMA. Medication-adherence predictors among patients with tuberculosis or human immunodeficiency virus infection in Burkina Faso. J Microbiol Immunol Infect. 2014;47(3):222–32.
Medley A, Seth P, Pathak S, et al. Alcohol use and its association with HIV risk behaviors among a cohort of patients attending HIV clinical care in Tanzania, Kenya, and Namibia. AIDS Care. 2014;26(10):1288–97.
Morojele NK, Kekwaletswe CT, Nkosi S. Associations between alcohol use, other psychosocial factors, structural factors and antiretroviral therapy (ART) adherence among South African ART recipients. AIDS Behav. 2014;18(3):519–24.
Nachega JB, Morroni C, Chaisson RE, et al. Impact of immune reconstitution inflammatory syndrome on antiretroviral therapy adherence. Patient Prefer Adher. 2012;6:887–91.
Nakimuli-Mpungu E, Mojtabai R, Alexandre PK, et al. Lifetime depressive disorders and adherence to anti-retroviral therapy in HIV-infected Ugandan adults: a case-control study. J Affect Disord. 2013;145(2):221–6.
Nduaguba SO, Soremekun RO, Olugbake OA, Barner JC. The relationship between patient-related factors and medication adherence among Nigerian patients taking highly active anti-retroviral therapy. Afr Health Sci. 2017;17(3):738–45.
Negash T, Ehlers V. Personal factors influencing patients’ adherence to ART in Addis Ababa, Ethiopia. J Assoc Nurses AIDS Care JANAC. 2013;24(6):530–8.
Newman J, Iriondo-Perez J, Hemingway-Foday J, et al. Older adults accessing HIV care and treatment and adherence in the IeDEA Central Africa cohort. AIDS Res Treat. 2012;2012:725713.
Pefura-Yone EW, Soh E, Kengne AP, Balkissou AD, Kuaban C. Non-adherence to antiretroviral therapy in Yaounde: prevalence, determinants and the concordance of two screening criteria. J Infect Public Health. 2013;6(4):307–15.
Peltzer K, Friend-du Preez N, Ramlagan S, Anderson J. Antiretroviral treatment adherence among HIV patients in KwaZulu-Natal, South Africa. BMC Public Health. 2010;10:111.
Ramlagan S, Peltzer K, Ruiter RAC, Barylski NA, Weiss SM, Sifunda S. Prevalence and factors associated with fixed-dose combination antiretroviral drugs adherence among HIV-positive pregnant women on Option B treatment in Mpumalanga Province, South Africa. Int J Environ Res Public Health. 2018;15(1):E161.
Ransome Y, Mayer KH, Tsuyuki K, et al. The role of religious service attendance, psychosocial and behavioral determinants of antiretroviral therapy (ART) adherence: results from HPTN 063 cohort study. AIDS Behav. 2019;23(2):459–74.
Sangeda EZ, Mosha F, Aboud S, et al. Predictors of non-adherence to antiretroviral therapy at an urban HIV care and treatment center in Tanzania. Drug Healthc Patient Saf. 2018;10:79–88.
Shumba C, Atuhaire L, Imakit R, Atukunda R, Memiah P. Missed doses and missed appointments: adherence to ART among adult patients in Uganda. ISRN AIDS. 2013;2013:270914.
Sileo KM, Simbayi LC, Abrams A, Cloete A, Kiene SM. The role of alcohol use in antiretroviral adherence among individuals living with HIV in South Africa: event-level findings from a daily diary study. Drug Alcohol Depend. 2016;167:103–11.
Sileo KM, Kitzito W, Wanyenze RK, et al. Substance use and its effect on antiretroviral treatment adherence among male fisherfolk living with HIV/AIDS in Uganda. PLoS ONE. 2019;14(6):e0216892.
Teshome W, Belayneh M, Moges M, Endriyas M, Mekonnen E, Ayele S, et al. Who takes the medicine? Adherence to antiretroviral therapy in Southern Ethiopia. Patient Prefer Adher. 2015;9:1531–7.
Veld DH, Pengpid S, Colebunders R, Skaal L, Peltzer K. High-risk alcohol use and associated socio-demographic, health and psychosocial factors in patients with HIV infection in three primary health care clinics in South Africa. Int J STD AIDS. 2017;28(7):651–9.
Wandera B, Tumwesigye NM, Nankabirwa JI, et al. Alcohol consumption among HIV-infected persons in a large urban HIV clinic in Kampala Uganda: a constellation of harmful behaviors. PloS ONE. 2015;10(5):e0126236.
Wandera B, Tumwesigye NM, Nankabirwa JI, et al. Hazardous alcohol consumption is not associated with CD4+ T-cell count decline among PLHIV in Kampala Uganda: a prospective cohort study. PloS ONE. 2017;12(6):e0180015.
Weiser SD, Palar K, Frongillo EA, et al. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28(1):115–20.
Yaya I, Landoh DE, Saka B, et al. Predictors of adherence to antiretroviral therapy among people living with HIV and AIDS at the regional hospital of Sokodé, Togo. BMC Public Health. 2014;14:1308.
WHO Assist Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–94.
Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88(6):791–804.
Bush K, Kivlahan, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95.
Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252(14):1905–7.
Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33.
Buscher A, Hartman C, Kallen MA, Giordano TP. Validity of self-report measures in assessing antiretroviral adherence of newly diagnosed, HAART-naïve, HIV patients. HIV Clin Trials. 2011;12(5):244–54.
Mannheimer SB, Mukherjee R, Hirschhorn LR, et al. The CASE adherence index: a novel method for measuring adherence to antiretroviral therapy. AIDS Care. 2006;18(7):853–61.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–54.
Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13(4):227–36.
Scott-Sheldon LAJ, Carey KB, Johnson BT, Carey MP, MASH Research Team. Behavioral interventions targeting alcohol use among people living with HIV/AIDS: a systematic review and meta-analysis. AIDS Behav. 2017;21(Suppl 2):126–43.
Simoni JM, Pearson CR, Pantalone DW, Marks G, Crepaz N. Efficacy of interventions in improving highly active antiretroviral therapy adherence and HIV-1 RNA viral load. A meta-analytic review of randomized controlled trials. J Acquir Immune Defic Syndr. 2006;43(1):S23.
Papas RK, Sidle JE, Gakinya BN, et al. Treatment outcomes of a stage 1 cognitive-behavioral trial to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction. 2011;106(12):2156–66.
Senyonyi RM, Underwood LA, Suarez E, Musisi S, Grande TL. Cognitive behavioral therapy group intervention for HIV transmission risk behavior in perinatally infected adolescents. Health. 2012;4(12):1334–45.
Wandera B, Tumwesigye NM, Nankabirwa JI, et al. Efficacy of a single, brief alcohol reduction intervention among men and women living with HIV/AIDS and using alcohol in Kampala, Uganda: a randomized trial. J Int Assoc Provid AIDS Care. 2017;16(3):276–85.
Bachanas P, Kidder D, Medley A, et al. Delivering prevention interventions to people living with HIV in clinical care settings: results of a cluster randomized trial in Kenya, Namibia, and Tanzania. AIDS Behav. 2016;20(9):2110–8.
Emenyonu NI, Fatch R, Muyindike WR, Kekibiina A, Woolf-King S, Hahn JA. Randomized study of assessment effects on alcohol use by persons with HIV in rural Uganda. J Stud Alcohol Drugs. 2017;78(2):296–305.
Edelman EJ, Hansen NB, Cutter CJ, et al. Implementation of integrated stepped care for unhealthy alcohol use in HIV clinics. Addict Sci Clin Pract. 2016;11(1):1.
World Health Organization. Global strategy to reduce the harmful use of alcohol. Geneva: World Health Organization; 2010.
Siegfried N, Parry C. Do alcohol control policies work? An umbrella review and quality assessment of systematic reviews of alcohol control interventions (2006–2017). PloS ONE. 2019;14(4):e0214865.
Sundström C, Blankers M, Khadjesari Z. Computer-based interventions for problematic alcohol use: a review of systematic reviews. Int J Behav Med. 2017;24(5):646–58.
Gordon S, Rotheram-Borus MJ, Skeen S, Parry C, Bryant K, Tomlinson M. Research priorities for the intersection of alcohol and HIV/AIDS in low and middle income countries: a priority setting exercise. AIDS Behav. 2017;21(Suppl 2):262–73.
Schroder KEE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26(2):104–23.
Alcaide ML, Ramlagan S, Rodriguez VJ, et al. Self-report and dry blood spot measurement of antiretroviral medications as markers of adherence in pregnant women in rural South Africa. AIDS Behav. 2017;21(7):2135–40.
Hahn JA, Bwana MB, Javors MA, Martin JN, Emenyonu NI, Bangsberg DR. Biomarker testing to estimate under-reported heavy alcohol consumption by persons with HIV initiating ART in Uganda. AIDS Behav. 2010;14(6):1265–8.
Morris C, Levine B, Goodridge G. Three-country assessment of alcohol-HIV related policy and programmatic responses in Africa. Afr J Drug Alcohol Stud. 2006;5:169–84.
Ioannidis JPA, Patsopoulos NA, Rothstein HR. Reasons or excuses for avoiding meta-analysis in forest plots. BMJ. 2008;336(7658):1413–5.
Acknowledgments
We are grateful for the dedication of the thousands of individuals who have participated in ART clinical trials and adherence studies around the world.
Funding
JV is supported by the National Institute of Mental Health of the US National Institutes of Health (F31 MH113420). CK is supported by a grant from the National Institute of Mental Health (F31 MH112397-01A1). FMA is supported by a grant from the National Institute of Allergy and Infectious Diseases (T32 AI07140). JMS is supported by P30 AI027757. The results and interpretation presented here do not necessarily reflect the views of the study funders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed were in accordance with the ethical standards of the University of Washington institutional review board, national research ethics committees for the study site, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Velloza, J., Kemp, C.G., Aunon, F.M. et al. Alcohol Use and Antiretroviral Therapy Non-Adherence Among Adults Living with HIV/AIDS in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. AIDS Behav 24, 1727–1742 (2020). https://doi.org/10.1007/s10461-019-02716-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02716-0