Abstract
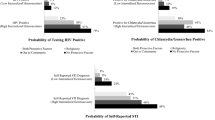
The present study sought to replicate effects of the number of syndemic psychosocial health conditions on sexual risk behavior and HIV infection among a sample of high-risk African American men who have sex with men (MSM) and to identify resilience factors that may buffer these effects. We used baseline data from an HIV risk-reduction trial to examine whether a higher number of syndemic conditions was associated with higher rates of self-reported sexual risk behavior and HIV infection. Using logistic regression models, we tested for interactions between number of syndemic conditions and several potential resilience factors to identify buffering effects. Replicating previous studies, we found significant associations between numbers of syndemic conditions and higher rates of sexual risk behavior and HIV infection. Surprisingly, we also replicated a previous finding (Stall et al., Am J Public Health, 93(6):939–942, 2003) that the effects of syndemic burden on HIV status fell off at the highest levels of syndemic conditions. Among a variety of potential resilience factors, two—optimism and education—buffered the syndemic effect on HIV prevalence. This is, to our knowledge, the first paper to identify resilience factors buffering against syndemic effects among MSM. It also constitutes a significant contribution to the literature regarding prevention among black MSM. These results point to the need to identify HIV-positive black MSM and provide effective treatment for them and to develop interventions addressing both syndemic and resilience factors.


Similar content being viewed by others
References
Singer M. AIDS and the health crisis of the urban poor: the perspective of critical Medical Anthropology. Soc Sci Med. 1994;39(7):931–48.
Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq. 1996;24(2):99–110.
Wallace R. A synergism of plagues. Environ Res. 1988;47:1–33.
Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. Am J Public Health. 2012;102(1):156–62.
Stall RD, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Pollack L, Binson D, Osmond D, Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–42.
Dyer TP, Shoptaw S, Guadamuz TE, Plankey M, Kao U, Ostrow D, Chmiel JS, Herrick A, Stall R. Application of syndemic theory to Black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health. 2012;89(4):696–708.
Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45.
Jie W, Ciyong L, Xueqing D, Hui W, Lingyao H. Syndemic of psychosocial problems places the MSM (men who have sex with men) population at greater risk of HIV infection. PLoS One. 2012;7(3):e32312.
Brennan J, Kuhns LM, Johnson AK, Belzer M, Wilson EC, Garofalo R. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102(9):1751–7.
Senn TE, Carey MP, Vanable PA. The intersection of violence, substance use, depression, and STDs: testing of a syndemic pattern among patients attending an urvan STD clinic. J Natl Med Assoc. 2010;102(7):614–20.
Bruce D, Harper GW. Operating without a safety net: gay male adolescents and emerging adults’ experiences of marginalization and migration, and implications for theory of syndemic production of health disparities. Health Educ Behar. 2011;38(4):367–78.
Herrick AL, Lim SH, Wei C, Smith H, Guadamuz T, Friedman MS, Stall R. Resilience as an untapped resource in behavioral intervention design for gay men. AIDS Behav. 2011;15:S25–9.
Herrick AL, Stall RD, Goldhammer H, Egan JE, Mayer KH. Resilience as a research framework and as a cornerstone of prevention research for gay and bisexual men: theory and evidence. AIDS Behav. 2013; doi:10.1007/s10461-012-0384-x.
Kurtz SP, Buttram ME, Surratt HL, Stall RD. Resilience, syndemic factors, and serosorting behaviors among HIV-positive and HIV-negative substance-using MSM. AIDS Educ Prev. 2012;24(3):193–205.
Jemmott JB, et al. (in preparation). Efficacy of a one-on-one HIV/STI risk reduction intervention for African American men who have sex with men: a randomized controlled trial.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Wyatt GE, Lawrence J, Vodounon A, et al. The Wyatt Sex History Questionnaire: a structured interview for female sexual history taking. J Child Sex Abuse. 1992;1:51–68.
Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252:1905–7.
Peters RH, Greenbaum PE, Steinberg ML, et al. Effectiveness of screening instruments in detecting substance use disorders among prisoners. J Subst Abuse Treat. 2000;18:349–58.
Lowmaster SE, Morey LC, Baker L, Hopwood CJ. Structure, reliability, and predictive validity of the Texas Christian University correctional residential self-rating form at intake in a residential substance abuse treatment facility. J Subst Abuse Treat. 2010;39(2):180–7.
Strauss M, Hamby S, Boney-McKoy S, et al. The revised conflict tactics scale (CTS2). J Fam Issues. 1996;17:283–316.
Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Social ties and susceptibility to the common cold. JAMA. 1997;277(24):1940–4. doi:10.1001/Jama.277.24.1940.
Pew Forum on Religion and Public Life. U.S. religious landscape survey, religious affiliation: diverse and dynamic. http://religions.pewforum.org/pdf/report-religious-landscapestudy-full.pdf (2008). Accessed Feb 2008.
Sellers RM, Rowley SAJ, Chavous TM, Shelton JN, Smith MA. Multidimensional inventory of black identity: a preliminary investigation of reliability and construct validity. J Pers Soc Psychol. 1997;73(4):805–15.
Brown JS, Rawlinson ME, Hilles NC. Life satisfaction and chronic disease: exploration of a theoretical model. Med Care. 1981;29:1136–46.
Cantril H. The pattern of human concerns. New Brunswick: Rutgers University Press; 1965.
Marks G, Millett GA, Bingham T, Bond L, Lauby J, Liau A, Murrill CS, Stueve A. Understanding differences in HIV sexual transmission among Latino and Black men who have sex with men: the Brothers y Hermanos Study. AIDS Behav. 2009;13:682–90.
Philadelphia Department of Public Health. Surveillance report, 2011 and construct validity. J Pers Soc Psychol. 2013;73(4):805–15. doi:10.1037/0022-3514.73.4.805.
Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57.
Rasmussen HN, Scheier M, Greenhouse JB. Optimism and physical health: a meta-analytic review. Ann Behav Med. 2013;37(3):239–56.
Centers for Disease Control and Prevention. HIV prevalence, unrecognized infection, and HIV testing among men who have sex with men—five U.S. cities, June 2004–April 2005. MMWR. 2005;54(24):597–601.
Centers for Disease Control and Prevention. Prevalence and awareness of HIV infection among men who have sex with men—21 cities, United States, 2008. MMWR. 2010;59(37):1201–7.
Millet GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96:1007–19.
Paul JP, Catania J, Pollack L, Stall R. Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: the Urban Men’s Health Study. Child Abuse Negl. 2001;25:557–84.
Greenwood GL, Reif MV, Huang B, Pollack LM, Canchola JA, Catania JA. Battering victimization among a probability=based sample of men who have sex with men. Am J Public Health. 2002;92:1964–9.
Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, Mills TC, Binson D, Coates TJ, Catania JA. Alcohol use, drug use and alcohol-related problems among men who have sex with men: the Urban Men’s Health Study. Addiction. 2001;96:1589–601.
Acknowledgments
The authors wish to recognize their funding source, the National Institute of Mental Health grant 1-R01-MH079736. We are grateful to many individuals who helped to bring this project to fruition, including Dr. Loretta S. Jemmott, Dr. Christopher Coleman, Janet Hsu, Brian Taylor, Mikia Croom, Pandora Woods, and Dennis Clegg. The findings and conclusions are those of the authors and do not necessarily reflect the official views of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Leary, A., Jemmott, J.B., Stevens, R. et al. Optimism and Education Buffer the Effects of Syndemic Conditions on HIV Status Among African American Men Who Have Sex with Men. AIDS Behav 18, 2080–2088 (2014). https://doi.org/10.1007/s10461-014-0708-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0708-0