Abstract
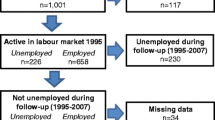
Too many people with HIV have left the job market permanently and those with reduced work capacity have been unable to keep their jobs. There is a need to examine the health effects of labor force participation in people with HIV. This study presents longitudinal data from 1,415 HIV-positive men who have sex with men taking part in the Multicenter AIDS Cohort Study. Generalized Estimating Equations show that employment is associated with better physical and mental health quality of life and suggests that there may be an adaptation process to the experience of unemployment. Post hoc analyses also suggest that people who are more physically vulnerable may undergo steeper health declines due to job loss than those who are generally healthier. However, this may also be the result of a selection effect whereby poor physical health contributes to unemployment. Policies that promote labor force participation may not only increase employment rates but also improve the health of people living with HIV.
Resumen
Demasiadas personas que viven con VIH han abandonado permanentemente el mercado laboral y aquellas con reducida capacidad de trabajo no han podido mantener sus puestos de trabajo. Es necesario evaluar los efectos de la participación laboral sobre la salud en personas que viven con VIH. Este estudio presenta datos longitudinales de 1,415 hombres VIH-positivos que tienen sexo con hombres, recabados del Multicenter AIDS Cohort Study. Ecuaciones de Estimación Generalizadas mostraron que el empleo esta asociado con mejor calidad de vida en relacion a la salud fisica y mental y ademas sugiere un proceso de adaptación a la experiencia de desempleo. Análisis posteriores y provisionales también sugieren que las personas físicamente mas vulnerables pueden sufrir caidas mas pronunciadas de la salud debido a la pérdida de empleo, comparados con aquellos que generalmente estan mas saludables. Sin embargo, esto también puede ser el resultado de un efecto de selección mediante el cual una salud física disminuida contribuye al desempleo. Las politicas que promueven la participación en el mercado laboral no solo podrian aumentar las tasas de empleo, sino también mejorar la salud de las personas que viven con VIH.



Similar content being viewed by others
References
Jin R, Shah C, Svoboda T. The impact of unemployment on health: a review of the evidence. J Public Health Policy. 1997;18:275–301.
Strully K. Job loss and health in the US labor market. Demography. 2009;46(2):221–46.
Price RH, Choi JN, Vinokur AD. Links in the chain of adversity following job loss: how financial strain and loss of personal control lead to depression, impaired functioning, and poor health. J Occup Health Psychol. 2002;7(4):302–12.
Gallo WT, Teng HM, Falba TA, Kasl SV, Krumholz HM, Bradley EH. The impact of late career job loss on myocardial infarction and stroke: a 10 year follow up using the health and retirement survey. Occup Environ Med. 2006;63(10):683–7.
Sullivan D, von Wachter T. Job displacement and mortality: an analysis using administrative data. Q J Econ. 2009;124(3):1265–306.
Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58(5):295–300.
Ginexi EM, Howe GW, Caplan RD. Depression and control beliefs in relation to reemployment: what are the directions of effect? J Occup Health Psychol. 2000;5(3):323–36.
Thomas C, Benzeval M, Stansfeld SA. Employment transitions and mental health: an analysis from the British household panel survey. J Epidemiol Community Health. 2005;59(3):243–9.
Bond GR, Resnick SG, Drake RE, Xie H, McHugo GJ, Bebout RR. Does competitive employment improve nonvocational outcomes for people with severe mental illness? J Consult Clin Psychol. 2001;69(3):489–501.
Martikainen P, Valkonen T. Excess mortality of unemployed men and women during a period of rapidly increasing unemployment. Lancet. 1996;348(9032):909–12.
Rueda S, Chambers L, Wilson M, Mustard C, Rourke S, Bayoumi A, et al. Association of returning to work with better health in working-aged adults: a systematic review. Am J Public Health. 2012;102(3):541–56.
Jahoda M. Work, employment, and unemployment: values, theories, and approaches in social research. Am Psychol. 1981;36(2):184–91.
Burgoyne R, Saunders D. Quality of life among urban Canadian HIV/AIDS clinic outpatients. Int J STD AIDS. 2001;12(8):505–12.
Dray-Spira R, Gueguen A, Ravaud J, Lert F. Socioeconomic differences in the impact of HIV infection on workforce participation in France in the era of highly active antiretroviral therapy. Am J Public Health. 2007;97(3):552–8.
Blalock A, McDaniel J, Farber E. Effect of employment on quality of life and psychological functioning in patients with HIV/AIDS. Psychosomatics. 2002;43(5):400–4.
Worthington C, Krentz H. Socio-economic factors and health-related quality of life in adults living with HIV. Int J STD AIDS. 2005;16:608–14.
Rueda S, Raboud J, Mustard C, Bayoumi A, Lavis J, Rourke S. Employment status is associated with both physical and mental health quality of life in people living with HIV. AIDS Care. 2011;23(4):435–43.
Dray-Spira R, Gueguen A, Persoz A, Deveau C, Lert F, Delfraissy J, et al. Temporary employment, absence of stable partnership, and risk of hospitalization or death during the course of HIV infection. J Acquir Immune Defic Syndr. 2005;40(2):190–7.
Silvestre A, Hylton J, Johnson L, Houston C, Witt M, Jacobson L, et al. Recruiting minority men who have sex with men for HIV research: results from a 4-city campaign. Am J Public Health. 2006;96(6):1020–7.
Kaslow RA, Ostrow DG, Detels R, Phair JP, Polk BF, Rinaldo CR Jr. The Multicenter AIDS Cohort Study: rationale, organization, and selected characteristics of the participants. Am J Epidemiol. 1987;126(2):310–8.
Detels R, Munoz A, McFarlane G, Kingsley LA, Margolick JB, Giorgi J, et al. Effectiveness of potent antiretroviral therapy on time to AIDS and death in men with known HIV infection duration. Multicenter AIDS Cohort Study Investigators. JAMA. 1998;280(17):1497–503.
Liu C, Johnson L, Ostrow D, Silvestre A, Visscher B, Jacobson L. Predictors for lower quality of life in the HAART era among HIV-infected men. J Acquir Immune Defic Syndr. 2006;42:470–7.
Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273(1):59–65.
Ware JE Jr, Sherbourne CD. 36-Item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Ware J, Kosinski M, Bjoner J, Turner-Bowker D, Gandeck B, Maruish M. User’s manual for the SF-36v2 health survey. 2nd ed. Lincoln: QualityMetric Incorporated; 2007.
Bing EG, Hays RD, Jacobson LP, Chen B, Gange SJ, Kass NE, et al. Health-related quality of life among people with HIV disease: results from the Multicenter AIDS Cohort Study. Qual Life Res. 2000;9(1):55–63.
Riley ED, Bangsberg DR, Perry S, Clark RA, Moss AR, Wu AW. Reliability and validity of the SF-36 in HIV-infected homeless and marginally housed individuals. Qual Life Res. 2003;12(8):1051–8.
Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22.
Twisk J. Applied longitudinal data analysis for epidemiology: a practical guide. Cambridge: Cambridge University Press; 2003.
Jones B, Nagin D, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29(3):374–93.
Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol Methods. 1999;4(2):139–57.
Dekker SWA, Schaufeli WB. The effects of job insecurity on psychological health and withdrawal: a longitudinal study. Aust Psychol. 1995;30(1):57–63.
Broom D, D’Souza R, Strazdins L, Butterworth P, Parslow R, Rodgers B. The lesser evil: bad jobs or unemployment? A survey of mid-aged Australians. Soc Sci Med. 2006;63:575–86.
Rueda S, Raboud J, Rourke S, Bekele T, Bayoumi A, Lavis J, et al. The influence of employment and job security on physical and mental health in HIV-positive patients: a cross-sectional analysis. Open Med. 2012 (in press).
Warr P, Jackson P. Adapting to the unemployed role: a longitudinal investigation. Soc Sci Med. 1987;25(11):1219–24.
Lucas R, Clark A, Georgellis Y, Diener E. Unemployment alters the set point for life satisfaction. Psychol Sci. 2004;15(1):8–13.
Morrell S, Taylor R, Quine S, Kerr C, Western J. A cohort study of unemployment as a cause of psychological disturbance in Australian youth. Soc Sci Med. 1994;38(11):1553–64.
Braveman B, Levin M, Kielhofner G, Finlayson M. HIV/AIDS and return to work: a literature review one-decade post-introduction of combination therapy (HAART). Work. 2006;27(3):295–303.
Martin DJ, Brooks RA, Ortiz DJ, Veniegas RC. Perceived employment barriers and their relation to workforce-entry intent among people with HIV/AIDS. J Occup Health Psychol. 2003;8(3):181–94.
Rabkin JG, McElhiney M, Ferrando SJ, Van Gorp W, Lin SH. Predictors of employment of men with HIV/AIDS: a longitudinal study. Psychosom Med. 2004;66(1):72–8.
Dray-Spira R, Gueguen A, Lert F. Disease severity, self-reported experience of workplace discrimination and employment loss during the course of chronic HIV disease: differences according to gender and education. Occup Environ Med. 2008;65(2):112–9.
Dray-Spira R, Persoz A, Boufassa F, Gueguen A, Lert F, Allegre T, et al. Employment loss following HIV infection in the era of highly active antiretroviral therapies. Eur J Pub Health. 2006;16(1):89–95.
Martin DJ, Arns PG, Batterham PJ, Afifi AA, Steckart MJ. Workforce reentry for people with HIV/AIDS: intervention effects and predictors of success. Work. 2006;27(3):221–33.
van Gorp WG, Rabkin JG, Ferrando SJ, Mintz J, Ryan E, Borkowski T, et al. Neuropsychiatric predictors of return to work in HIV/AIDS. J Int Neuropsychol Soc. 2007;13(1):80–9.
Acknowledgments
The Multicenter AIDS Cohort Study (MACS) includes the following: Baltimore: The Johns Hopkins University Bloomberg School of Public Health: Joseph B. Margolick (Principal Investigator), Michael Plankey (Co-Principal Investigator), Barbara Crain, Adrian Dobs, Homayoon Farzadegan, Joel Gallant, Lisette Johnson-Hill, Ned Sacktor, Ola Selnes, James Shepard, Chloe Thio. Chicago: Howard Brown Health Center, Feinberg School of Medicine, Northwestern University, and Cook County Bureau of Health Services: John P. Phair (Principal Investigator), Steven M. Wolinsky (Principal Investigator), Sheila Badri, Craig Conover, Maurice O’Gorman, David Ostrow, Frank Palella, Ann Ragin. Los Angeles: University of California, UCLA Schools of Public Health and Medicine: Roger Detels (Principal Investigator), Otoniel Martínez-Maza (Co-Principal Investigator), Aaron Aronow, Robert Bolan, Elizabeth Breen, Anthony Butch, John Fahey, Beth Jamieson, Eric N. Miller, John Oishi, Harry Vinters, Barbara R. Visscher, Dorothy Wiley, Mallory Witt, Otto Yang, Stephen Young, Zuo Feng Zhang. Pittsburgh: University of Pittsburgh, Graduate School of Public Health: Charles R. Rinaldo (Principal Investigator), Lawrence A. Kingsley (Co-Principal Investigator), James T. Becker, Ross D. Cranston, Jeremy J. Martinson, John W. Mellors, Anthony J. Silvestre, Ronald D. Stall. Data Coordinating Center: The Johns Hopkins University Bloomberg School of Public Health: Lisa P. Jacobson (Principal Investigator), Alvaro Munoz (Co-Principal Investigator), Alison, Abraham, Keri Althoff, Christopher Cox, Gypsyanber D’Souza, Stephen J. Gange, Elizabeth Golub, Janet Schollenberger, Eric C. Seaberg, Sol Su. NIH: National Institute of Allergy and Infectious Diseases: Robin E. Huebner; National Cancer Institute: Geraldina Dominguez. UO1-AI-35042, UL1-RR025005, UO1-AI-35043, UO1-AI-35039, UO1-AI-35040, UO1-AI-35041. Website located at http://www.statepi.jhsph.edu/macs/macs.html.
Conflict of interest
There are no conflicts of interest related to this paper and project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rueda, S., Raboud, J., Plankey, M. et al. Labor Force Participation and Health-Related Quality of Life in HIV-Positive Men Who Have Sex with Men: The Multicenter AIDS Cohort Study. AIDS Behav 16, 2350–2360 (2012). https://doi.org/10.1007/s10461-012-0257-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0257-3