Abstract
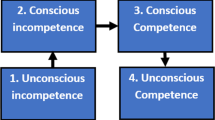
Changing the culture of medicine through the education of medical students has been proposed as a solution to the intractable problems of our profession. Yet few have explored the issues associated with making students partners in this change. There is a powerful hidden curriculum that perpetuates not only desired attitudes and behaviors but also those that are less than desirable. So, how do we educate medical students to resist adopting unprofessional practices they see modeled by supervisors and mentors in the clinical environment? This paper explores these issues and, informed by the literature, we propose a specific set of reflective competencies for medical students as they transition from classroom curricula to clinical practice in a four-step approach: (1) Priming—students about hidden curriculum in their clinical environment and their motivations to conform or comply with external pressures; (2) Noticing—educating students to be aware of their motivations and actions in situations where they experience pressures to conform to practices that they may view as unprofessional; (3) Processing—guiding students to analyze their experiences in collaborative reflective exercises and finally; (4) Choosing—supporting students in selecting behaviors that validate and reinforce their aspirations to develop their best professional identity.
Similar content being viewed by others
References
AFMC. (2009). The future of medical education in canada (fmec) [Online]. http://www.afmc.ca/projects-international-future-med-can-e.php
Amalberti, R., Auroy, Y., Berwick, D., & Barach, P. (2005). Five system barriers to achieving ultrasafe health care. Annals of Internal Medicine, 142, 756–764.
Asch, S. (1951). Effects of group pressure upon the modification and distortion of judgment. Pittsburgh: Carnegie Press.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall.
Bandura, A., & Huston, A. C. (1961). Identification as a process of incidental learning. Journal of Abnormal and Social Psychology, 63, 311–312.
Bargh, J. A., & Chartrand, T. L. (1999). The unbearable automaticity of being. American Psychologist, 54, 462–479.
Blanton, H., & Christie, C. (2003). Deviance regulation: A theory of action and identity. Review of General Psychology, 7, 115–149.
Boelen, C., & Woollard, B. (2009). Social accountability and accreditation: A new frontier for educational institutions. Medical Education, 43, 887–894.
Bombeke, K., Symons, L., Debaene, L., De Winter, B., Schol, S., & Van Royen, P. (2010). Help, i’m losing patient-centredness! Experiences of medical students and their teachers. Medical Education, 44, 662–673.
Brainard, A. H., & Brislen, H. C. (2007). Viewpoint: Learning professionalism: A view from the trenches. Academic Medicine, 82, 1010–1014.
Brigley, S., Young, Y., Littlejohns, P., & Mcewen, J. (1997). Continuing education for medical professionals: A reflective model. Postgraduate Medical Journal, 73, 23–26.
Brookfield, S. D. (1987). Developing critical thinkers: Challenging adults to explore alternative ways of thinking and acting. San Francisco: Jossey-Bass Inc.
Cialdini, R. B., & Goldstein, N. J. (2004). Social influence: Compliance and conformity. Annual Review of Psychology, 55, 591–621.
CMPA. (2012). Team communication; speaking up. Good Practices Guide [Online]. http://www.cmpa-acpm.ca/cmpapd04/docs/ela/goodpracticesguide/pages/communication/Team_Communication/speaking_up-e.html
Cohen, M. J., Kay, A., Youakim, J. M., & Balaicuis, J. M. (2009). Identity transformation in medical students. American Journal of Psychoanalysis, 69, 43–52.
Coulehan, J., & Williams, P. C. (2001). Vanquishing virtue: The impact of medical education. Academic Medicine, 76, 598–605.
Cribb, A., & Bignold, S. (1999). Towards the reflexive medical school: The hidden curriculum and medical education research. Studies in Higher Education, 24, 195–209.
Dwyer, J. (1994). Primum non tacere. An ethics of speaking up. Hastings Center Report, 24, 13–18.
Eva, K. W., & Regehr, G. (2008). “I’ll never play professional football” and other fallacies of self-assessment. Journal of Continuing Education in the Health Professions, 28, 14–19.
Ferrer, R. A., Dillard, A. J., & Klein, W. M. (2012). Projection, conformity and deviance regulation: A prospective study of alcohol use. Psychology & Health, 27, 688–703.
Festinger, L. (1957). A theory of cognitive dissonance. Stanford: Stanford University Press.
Feudtner, C., & Christakis, D. A. (1994). Making the rounds. The ethical development of medical students in the context of clinical rotations. Hastings Center Report, 24, 6–12.
Fischer, M. A., Mazor, K. M., Baril, J., Alper, E., Demarco, D., & Pugnaire, M. (2006). Learning from mistakes. Factors that influence how students and residents learn from medical errors. Journal of General Internal Medicine, 21, 419–423.
Frankford, D. M., Patterson, M. A., & Konrad, T. R. (2000). Transforming practice organizations to foster lifelong learning and commitment to medical professionalism. Academic Medicine, 75, 708–717.
Gaufberg, E. H., Batalden, M., Sands, R., & Bell, S. K. (2010). The hidden curriculum: What can we learn from third-year medical student narrative reflections? Academic Medicine, 85, 1709–1716.
Ginsburg, S., Lingard, L., Regehr, G., & Underwood, K. (2008). Know when to rock the boat: How faculty rationalize students’ behaviors. Journal of General Internal Medicine, 23, 942–947.
Ginsburg, S., Regehr, G., & Lingard, L. (2003). The disavowed curriculum: Understanding student’s reasoning in professionally challenging situations. Journal of General Internal Medicine, 18, 1015–1022.
Ginsburg, S., Regehr, G., Stern, D., & Lingard, L. (2002). The anatomy of the professional lapse: Bridging the gap between traditional frameworks and students’ perceptions. Academic Medicine, 77, 516–522.
Goldie, J., Schwartz, L., Mcconnachie, A., & Morrison, J. (2003). Students’ attitudes and potential behaviour with regard to whistle blowing as they pass through a modern medical curriculum. Medical Education, 37, 368–375.
Graber, M. L. (2009). Safety for beginners: Thoughts on teaching patient safety to medical undergraduates. Medical Education, 43, 1125–1126.
Hafferty, F. W. (1998). Beyond curriculum reform: Confronting medicine’s hidden curriculum. Academic Medicine, 73, 403–407.
Harris, I. B. (1993). Perspectives for curriculum renewal in medical education. Academic Medicine, 68, 484–486.
Harris, I. (2011). Conceptions and theories of learning for workplace education. In J. P. Hafler (Ed.), Extraordinary learning in the workplace. Dordrecht: Springer.
Hornsey, M. J., Majkut, L., Terry, D. J., & Mckimmie, B. M. (2003). On being loud and proud: Non-conformity and counter-conformity to group norms. British Journal of Social Psychology, 42, 319–335.
Hornsey, M. J., Smith, J. R., & Begg, D. (2007). Effects of norms among those with moral conviction: Counter-conformity emerges on intentions but not behaviors. Social Influence, 2, 244–268.
Jackson, P. W. (1968). Life in classrooms. New York: Holt, Rinehart and Winston.
Jarvis-Selinger, S., Pratt, D. D., & Regehr, G. (2012). Competency is not enough: Integrating identity formation into the medical education discourse. Academic Medicine, 87, 1185–1190.
Jochemsen-Van Der Leeuw, H. G., Van Dijk, N., Van Etten-Jamaludin, F. S., & Wieringa-De Waard, M. (2013). The attributes of the clinical trainer as a role model: A systematic review. Academic Medicine, 88, 26–34.
Karnieli-Miller, O., Vu, T. R., Holtman, M. C., Clyman, S. G., & Inui, T. S. (2010). Medical students’ professionalism narratives: A window on the informal and hidden curriculum. Academic Medicine, 85, 124–133.
Kawulich, B. B. (2005). Participant observation as a data collection method. Mayo 2005 [Online], 6. http://www.qualitative-research.net/index.php/fqs/article/view/466/996
Kohn, L., Corrigan, J., & Donaldson, M. S. (1999). To err is human: Building a safer health system. Washington, DC: Institutes of Medicine.
Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development. Englewood Cliffs, NJ: Prentice-Hall.
Kulier, R., Gee, H., & Khan, K. S. (2008). Five steps from evidence to effect: Exercising clinical freedom to implement research findings. BJOG, 115, 1197–1202.
Lave, J., & Wenger, E. (1991). Situated learning: Legitimate peripheral participation. New York: Cambridge University Press.
Leape, L. L., & Berwick, D. (2010). Unmet needs; teaching physicians to provide safe patient care. In Institute, L. L. (Ed.). Boston: National Patient Safety Foundation [Online], http://www.npsf.org/wpcontent/uploads/2011/10/LLI-Unmet-Needs-Report.pdf
Leape, L. L., Shore, M. F., Dienstag, J. L., Mayer, R. J., Edgman-Levitan, S., Meyer, G. S., et al. (2012a). Perspective: A culture of respect, part 1: The nature and causes of disrespectful behavior by physicians. Academic Medicine, 87, 845–852.
Leape, L. L., Shore, M. F., Dienstag, J. L., Mayer, R. J., Edgman-Levitan, S., Meyer, G. S., et al. (2012b). Perspective: A culture of respect, part 2: Creating a culture of respect. Academic Medicine, 87, 853–858.
Loftus, E. (2003). Our changeable memories: Legal and practical implications. Nature Reviews Neuroscience, 4, 231–234.
Mann, K., Gordon, J., & Macleod, A. (2009). Reflection and reflective practice in health professions education: A systematic review. Advances in Health Sciences Education: Theory and Practice, 14, 595–621.
Mauksch, L., Farber, S., & Greer, H. T. (2013). Design, dissemination, and evaluation of an advanced communication elective at seven U.S. Medical schools. Academic Medicine, 88, 843–851.
Mayer, D., Klamen, D. L., Gunderson, A., & Barach, P. (2009). Designing a patient safety undergraduate medical curriculum: The telluride interdisciplinary roundtable experience. Teaching and Learning in Medicine, 21, 52–58.
Mcconnell, M. M., & Eva, K. W. (2012). The role of emotion in the learning and transfer of clinical skills and knowledge. Academic Medicine, 87, 1316–1322.
Mezirow, J. (1990). Fostering critical reflection in adulthood: A guide to transformative and emancipatory learning. San Francisco: Jossey-Bass.
Moulton, C. A., Regehr, G., Mylopoulos, M., & Macrae, H. M. (2007). Slowing down when you should: A new model of expert judgment. Academic Medicine, 82, S109–S116.
Mylopoulos, M., & Regehr, G. (2007). Cognitive metaphors of expertise and knowledge: Prospects and limitations for medical education. Medical Education, 41, 1159–1165.
Neumann, M., Edelhauser, F., Tauschel, D., Fischer, M. R., Wirtz, M., Woopen, C., et al. (2011). Empathy decline and its reasons: A systematic review of studies with medical students and residents. Academic Medicine, 86, 996–1009.
Nisbett, R. E., & Wilson, T. D. (1977). Telling more than we can know—Verbal reports on mental processes. Psychological Review, 84, 231–259.
Nolan, J. M., Schultz, P. W., Cialdini, R. B., Goldstein, N. J., & Griskevicius, V. (2008). Normative social influence is underdetected. Personality and Social Psychology Bulletin, 34, 913–923.
Papadimos, T. J., & Murray, S. J. (2008). Foucault’s “fearless speech” and the transformation and mentoring of medical students. Ethics, and Humanities in Medicine, 3, 12.
Patenaude, J., Niyonsenga, T., & Fafard, D. (2003). Changes in students’ moral development during medical school: A cohort study. CMAJ, 168, 840–844.
Portelli, J. P. (1993). Exposing the hidden curriculum. Journal of Curriculum Studies, 25, 343–358.
Reeves, S., Perrier, L., Goldman, J., Freeth, D., & Zwarenstein, M. (2013). Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database of Systematic Reviews, 3, CD002213.
Rennie, S. C., & Crosby, J. R. (2002). Students’ perceptions of whistle blowing: Implications for self-regulation. A questionnaire and focus group survey. Medical Education, 36, 173–179.
Sandars, J. (2009). The use of reflection in medical education: Amee guide no. 44. Medical Teacher, 31, 685–695.
Sandars, J., & Murray, C. (2011). Digital storytelling to facilitate reflective learning in medical students. Medical Education, 45, 649.
Sandars, J., Murray, C., & Pellow, A. (2008). Twelve tips for using digital storytelling to promote reflective learning by medical students. Medical Teacher, 30, 774–777.
Schön, D. A. (1987). Educating the reflective practitioner. San Francisco: Jossey-Bass.
Treadway, K., & Chatterjee, N. (2011). Into the water—The clinical clerkships. New England Journal of Medicine, 364, 1190–1193.
UK-Consensus-Statement. (1998). Teaching medical ethics and law within medical education: A model for the UK core curriculum. Journal of Medical Ethics, 24, 188–192.
Wilson, T. D., & Brekke, N. (1994). Mental contamination and mental correction—Unwanted influences on judgments and evaluations. Psychological Bulletin, 116, 117–142.
Wong, B. M., Etchells, E. E., Kuper, A., Levinson, W., & Shojania, K. G. (2010). Teaching quality improvement and patient safety to trainees: A systematic review. Academic Medicine, 85, 1425–1439.
Zimbardo, P. G., & Leippe, M. R. (1991). The psychology of attitude change and social influence. Philadelphia: Temple University Press.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holmes, C.L., Harris, I.B., Schwartz, A.J. et al. Harnessing the hidden curriculum: a four-step approach to developing and reinforcing reflective competencies in medical clinical clerkship. Adv in Health Sci Educ 20, 1355–1370 (2015). https://doi.org/10.1007/s10459-014-9558-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-014-9558-9