Abstract
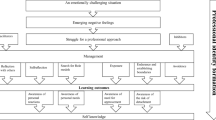
Dealing with emotions is a critical feature of professional behaviour. There are no comprehensive theoretical models, however, explaining how medical students learn about emotions. We aimed to explore factors affecting their emotions and how they learn to deal with emotions in themselves and others. During a first-year nursing attachment in hospitals and nursing homes, students wrote daily about their most impressive experiences, explicitly reporting what they felt, thought, and did. In a subsequent interview, they discussed those experiences in greater detail. Following a grounded theory approach, we conducted a constant comparative analysis, collecting and then interpreting data, and allowing the interpretation to inform subsequent data collection. Impressive experiences set up tensions, which gave rise to strong emotions. We identified four ‘axes’ along which tensions were experienced: ‘idealism versus reality’, ‘critical distance versus adaptation’, ‘involvement versus detachment’ and ‘feeling versus displaying’. We found many factors, which influenced how respondents relieved those tensions. Their personal attributes and social relationships both inside and outside the medical community were important ones. Respondents’ positions along the different dimensions, as determined by the balance between attributes and tensions, shaped their learning outcomes. Medical students’ emotional development occurs through active participation in medical practice and having impressive experiences within relationships with patients and others on wards. Tensions along four dimensions give rise to strong emotions. Gaining insight into the many conditions that influence students’ learning about emotions might support educators and supervisors in fostering medical students’ emotional and professional development.

Similar content being viewed by others
References
Anderson, S. W., Bechara, A., Damasio, H., Tranel, D., & Damasio, A. R. (1999). Impairment of social and moral behavior related to early damage in human prefrontal cortex. Nature Neuroscience, 2, 1032–1037.
Annells, M. (1997). Grounded theory method, part I: Within the five moments of qualitative research. Nursing Inquiry, 4, 120–129.
Arora, S., Ashrafian, H., Davis, R., Athanasiou, T., Darzi, A., & Sevdalis, N. (2010). Emotional intelligence in medicine: A systematic review through the context of the ACGME competencies. Medical Education, 44, 749–764.
Barbour, R. S. (2001). Checklists for improving rigour in qualitative research: A case of the tail wagging the dog? British Medical Journal, 322, 1115–1117.
Beach, M. C., & Inui, T. (2006). Relationship-centered care. A constructive reframing. Journal of General Internal Medicine, 21(Suppl 1), S3–S8.
Bell, K., Boshuizen, H. P., Scherpbier, A., & Dornan, T. (2009). When only the real thing will do: Junior medical students’ learning from real patients. Medical Education, 43, 1036–1043.
Bleakley, A. (2006). Broadening conceptions of learning in medical education: The message from teamworking. Medical Education, 40, 150–157.
Boiger, M., & Mesquita, B. (2012). The construction of emotion in interactions, relationships, and cultures. Emotion Review, 4, 221–229.
Bombeke, K., Symons, L., Debaene, L., De Winter, B., Schol, S., & Van Royen, P. (2010). Help, I’m losing patient-centredness! Experiences of medical students and their teachers. Medical Education, 44, 662–673.
Boor, K., Scheele, F., van der Vleuten, C. P. M., Teunissen, P. W., den Breejen, E. M., & Scherpbier, A. J. (2008). How undergraduate clinical learning climates differ: A multi-method case study. Medical Education, 42, 1029–1036.
Bordage, G. (2007). Moving the field forward: Going beyond quantitative-qualitative. Academic Medicine, 82, S126–S128.
Brannick, M. T., Wahi, M. M., Arce, M., Johnson, H. A., Nazian, S., & Goldin, S. B. (2009). Comparison of trait and ability measures of emotional intelligence in medical students. Medical Education, 43, 1062–1068.
Carver, C. S., & Connor-Smith, J. (2010). Personality and coping. Annual Review of Psychology, 61, 679–704.
Charon, R. (2001). The patient-physician relationship. Narrative medicine: A model for empathy, reflection, profession, and trust. The Journal of the American Medical Association, 286, 1897–1902.
Cherry, M. G., Fletcher, I., O’Sullivan, H., & Shaw, N. (2012). What impact do structured educational sessions to increase emotional intelligence have on medical students? BEME Guide No. 17. Medical Teacher, 34, 11–19.
Corbin, J., & Strauss, A. (2008). Basics of qualitative research. Thousand Oaks, CA: Sage Publications.
Croskerry, P., Abbass, A. A., & Wu, A. W. (2008). How doctors feel: Affective issues in patients’ safety. Lancet, 372, 1205–1206.
Croskerry, P., Abbass, A., & Wu, A. W. (2010). Emotional influences in patient safety. Journal of Patient Safety, 6, 199–205.
DasGupta, S., & Charon, R. (2004). Personal illness narratives: Using reflective writing to teach empathy. Academic Medicine, 79, 351–356.
Dobie, S. (2007). Viewpoint: reflections on a well-traveled path: Self-awareness, mindful practice, and relationship-centered care as foundations for medical education. Academic Medicine, 82, 422–427.
Dornan, T., Boshuizen, H., King, N., & Scherpbier, A. (2007). Experience-based learning: A model linking the processes and outcomes of medical students’ workplace learning. Medical Education, 41, 84–91.
Dyrbye, L. N., Harris, I., & Rohren, C. H. (2007). Early clinical experiences from students’ perspectives: A qualitative study of narratives. Academic Medicine, 82, 979–988.
Epstein, R. M. (1999). Mindful practice. The Journal of the American Medical Association, 282, 833–839.
Grewal, D., & Davidson, H. A. (2008). Emotional intelligence and graduate medical education. The Journal of the American Medical Association, 300, 1200–1202.
Helmich, E., Bolhuis, S., Dornan, T., Laan, R., & Koopmans, R. (2012). Entering medical practice for the very first time: Emotional talk, meaning and identity development. Medical Education, 46, 1074–1086.
Helmich, E., Bolhuis, S., Laan, R., & Koopmans, R. (2011a). Early clinical experience: Do students learn what we expect? Medical Education, 45, 731–740.
Helmich, E., Bolhuis, S., Prins, J., Laan, R., & Koopmans, R. (2011b). Emotional learning of undergraduate medical students in an early nursing attachment in a hospital or nursing home. Medical Teacher, 33, e593–e601.
Helmich, E., Derksen, E., Prevoo, M., Laan, R., Bolhuis, S., & Koopmans, R. (2010). Medical students’ professional identity development in an early nursing attachment. Medical Education, 44, 674–682.
Hochschild, A. R. (1979). Emotion work, feeling rules, and social-structure. American Journal of Sociology, 85, 551–575.
Holland, D., Lachicotte, W., Skinner, D., & Cain, C. (1998). Identity and agency in cultural worlds. Cambridge: Harvard University Press.
Immordino-Yang, M. H., & Damasio, A. (2007). We feel, therefore we learn: The relevance of affective and social neuroscience to education. Mind, brain, and education, 1, 3–10.
Karnieli-Miller, O., Vu, T. R., Holtman, M. C., Clyman, S. G., & Inui, T. S. (2010). Medical students’ professionalism narratives: A window on the informal and hidden curriculum. Academic Medicine, 85, 124–133.
Kelly, E., & Nisker, J. (2010). Medical students’ first clinical experiences of death. Medical Education, 44, 421–428.
Larson, E. B., & Yao, X. (2005). Clinical empathy as emotional labor in the patient-physician relationship. The Journal of the American Medical Association, 293, 1100–1106.
Lave, J., & Wenger, E. (1991). Situated learning. Legitimate peripheral participation. New York: Cambridge University Press.
Lewis, N. J., Rees, C. E., Hudson, J. N., & Bleakley, A. (2005). Emotional intelligence medical education: Measuring the unmeasurable? Advances in Health Sciences Education: Theory and Practice, 10, 339–355.
Mann, S. (2005). A health-care model of emotional labour. Journal of Health Organization and Management, 19, 304–317.
McConnell, M. M., & Eva, K. W. (2012). The role of emotion in the learning and transfer of clinical skills and knowledge. Academic Medicine, 87, 1316–1322.
Montgomery, A. J., Panagopolou, E., & Benos, A. (2005). Emotional labour at work and at home among Greek health-care home professionals. Journal of Health Organization and Management, 19, 395–408.
Novack, D. H., Epstein, R. M., & Paulsen, R. H. (1999). Toward creating physician-healers: Fostering medical students’ self-awareness, personal growth, and well-being. Academic Medicine, 74, 516–520.
Pitkala, K. H., & Mantyranta, T. (2004). Feelings related to first patient experiences in medical school. A qualitative study on students’ personal portfolios. Patient Education and Counseling, 54, 171–177.
Pugh, S. D., Groth, M., & Hennig-Thurau, T. (2011). Willing and able to fake emotions: A closer examination of the link between emotional dissonance and employee well-being. Journal of Applied Psychology, 96, 377–390.
Ratanawongsa, N., Teherani, A., & Hauer, K. E. (2005). Third-year medical students’ experiences with dying patients during the internal medicine clerkship: A qualitative study of the informal curriculum. Academic Medicine, 80, 641–647.
Rhodes-Kropf, J., Carmody, S. S., Seltzer, D., Redinbaugh, E., Gadmer, N., Block, S. D., et al. (2005). “This is just too awful; I just can’t believe I experienced that…”: Medical students’ reactions to their “most memorable” patient death. Academic Medicine, 80, 634–640.
Satterfield, J. M., & Hughes, E. (2007). Emotion skills training for medical students: A systematic review. Medical Education, 41, 935–941.
Shapiro, J. (2011). Perspective: Does medical education promote professional alexithymia? A call for attending to the emotions of patients and self in medical training. Academic Medicine, 86, 326–332.
Shapiro, J., Morrison, E., & Boker, J. (2004). Teaching empathy to first year medical students: Evaluation of an elective literature and medicine course. Education for Health (Abingdon), 17, 73–84.
Smith, A. C., & Kleinman, S. (1989). Managing emotions in medical school: Students’ contact with living and the dead. Social Psychology Quarterly, 52, 56–69.
Teunissen, P. W., Scheele, F., Scherpbier, A. J., van der Vleuten, C. P. M., Boor, K., van Luijk, S. J., et al. (2007). How residents learn: Qualitative evidence for the pivotal role of clinical activities. Medical Education, 41, 763–770.
Turner, J. H. (2009). The sociology of emotions: Basic theoretical arguments. Emotion Review, 1, 340–354.
Wald, H. S., Reis, S. P., Monroe, A. D., & Borkan, J. M. (2010). ‘The Loss of My Elderly Patient:’ Interactive reflective writing to support medical students’ rites of passage. Medical Teacher, 32, e178–e184.
Wenger, E. (1998). Communities of practice. Learning, meaning, and identity. Cambridge: Cambridge University Press.
Zembylas, M. (2007). Theory and methodology in researching emotions in education. International Journal of research & Method in Education, 30, 57–72.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Helmich, E., Bolhuis, S., Laan, R. et al. Medical students’ emotional development in early clinical experience: a model. Adv in Health Sci Educ 19, 347–359 (2014). https://doi.org/10.1007/s10459-013-9477-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10459-013-9477-1