Abstract
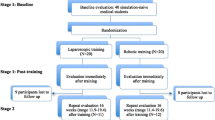
Our aim was to test our laparoscopic simulator for construct validity and for establishing performance standards. The skills of laparoscopic novices (n = 18) and advanced gynaecologists (experts, n = 5) were tested on our inanimate simulator by their performance of five tasks. The sum score was the sum of scores of all five tasks. We calculated the scores by adding completion time and penalty points. After baseline evaluation, the novices were assigned to five weekly training sessions (n = 8, training group) or no training (n = 10, control group). Both groups were retested. The experts were tested once, and their performance was compared with the baseline scores of all novices to establish construct validity. The training group improved significantly in all tasks. The final scores of the trained group were significantly better than those of the control group. The training group reached a plateau within seven trials, except for intra-corporeal knot tying. During final testing, the trained group reached the experts’ level of skills on the simulator. We concluded that our simulation model has construct validity. Novices can reach the experts’ basic laparoscopic skills level on the simulator after a short and intense simulator training course. Experts’ basic skills level on the simulator is an achievable performance standard during residency training.



Similar content being viewed by others
References
Darzi A, Mackay S (2002) Recent advances in minimal access surgery. BMJ 423:31–34
Lehmann KS, Ritz JP, Maass H, Cakmak HK, Kuehnapfel UG, Germer CT, Bretthauer G, Buhr HJ (2005) A prospective randomized study to test the transfer of basic psychomotor skills from virtual reality to physical reality in a comparable training setting. Ann Surg 241:442–449
Munz Y, Kumar BD, Moorthy K, Bann S, Darzi A (2004) Laparoscopic virtual reality and boxtrainers. Is one superior to the other? Surg Endosc 18:485–494
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–528
Derossis AM, Antoniuk M, Fried GM (1999) Evaluation of laparoscopic skills: a 2-year follow-up during residency training. Can J Surg 42:293–296
Jordan JA, Gallagher AG, McGuigan J, McClure N (2001) Virtual reality training leads to faster adaptation to the novel psychomotor restrictions encountered by laparoscopic surgeons. Surg Endosc 15:1080–1084
Lentz GM, Mandel LS, Lee D, Gardella C, Melville J, Goff BA (2001) Testing surgical skills of obstetrics and gynecologic residents in a bench laboratory setting: validity and reliability. Am J Obstet Gynecol 184:1462–1470
Rosser JC, Rosser LE, Savalgi RS (1997) Skill acquisition and assessment for laparoscopic surgery. Arch Surg 132:200–204
Scott DJ, Young WN, Tesfay ST, Tesfay ST, Frawley WH, Rege RV, Jones DB (2001) Laparoscopic skills training. Am J Surg 182:137–142
Fraser SA, Klassen DR, Feldman LS, Ghitulescu GA, Stanbridge D, Fried GM (2003) Evaluating laparoscopic skills: setting the pass/fail score for the MISTELS system. Surg Endosc 17:964–967
Reznick R, Regehr G, MacRae H, Martin J, McCulloch W (1997) Testing technical skill via an innovative "bench station" examination. Am J Surg 173:226–230
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91:146–150
Hamilton EC, Scott DJ, Fleming JB, Rege RV, Laycock R, Bergen PC, Tesfay ST, Jones DB (2002) Comparison of video trainer and virtual reality training systems on acquisition of laparoscopic skills. Surg Endosc 16:406–411
Hyltander A, Liljegren E, Rhodin PH, Lonroth H (2002) The transfer of basic skills learning in a laparoscopic simulator to the operating room. Surg Endosc 16:1324–1328
Jakimowicz JJ, Cuschieri A (2005) Time for evidence-based minimal access surgery training—simulate or sink. Surg Endosc 19:1521–1522
Korndorffer JR Jr, Clayton JL, Tesfay ST, Brunner WC, Sierra R, Dunne JB, Jones DB, Rege RV, Touchard CL, Scott DJ (2005) Multicenter construct validity for Southwestern laparoscopic videotrainer stations. J Surg Res 128:114–119
Derossis AM, Fried GM, Abrahamowicz M, Sigman HH, Barkun JS, Meakins JL (1998) Development of a model for training and evaluation of laparoscopic skills. Am J Surg 175(6):482–487
Stefanidis D, Korndorffer JR Jr, Sierra R, Touchard C, Dunne JB, Scott DJ (2005) Skill retention following proficiency-based laparoscopic simulator training. Surgery 138:165–170
Stefanidis D, Korndorffer JR Jr, Markley S, Sierra R, Scott DJ (2006) Proficiency maintenance: impact of ongoing simulator training on laparoscopic skill retention. J Am Coll Surg 2024:599–603
Torkington J, Smith SG, Rees B, Darzi A (2001) The role of the basic laparoscopic skills course in the acquisition and retention of laparoscopic skill. Surg Endosc 15:1071–1075
Acknowledgements
We thank all the students and gynaecologists for participating in our study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kolkman, W., van de Put, M.A.J., Wolterbeek, R. et al. Laparoscopic skills simulator: construct validity and establishment of performance standards for residency training. Gynecol Surg 5, 109–114 (2008). https://doi.org/10.1007/s10397-007-0345-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10397-007-0345-y