Abstract
Aim/ Background
Few or no data are currently available in Germany on the effects of different acceptance by the pharmaceutical manufacturers and the implementation of fixed prices for drugs, some of which are still under patent protection. We therefore investigated the extent to which patients who were prescribed atorvastatin in the third quarter of 2004 continued to receive lipid-lowering treatment during the first three quarters of 2005 and whether a change in treatment altered their risk-factor profile, particularly their cholesterol levels.
Methods
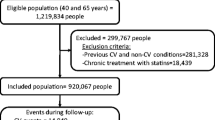
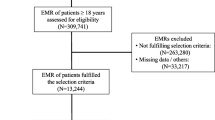
To prevent any study-related influence on prescribing practice, we conducted a retrospective study that included up to 50 patients from each of 52 GP or internist practices who were prescribed atorvastatin in the third quarter of 2004. We documented the patients’ risk-factor profile, age, sex, BMI, insurance status, and blood pressure as well as prescriptions of lipid-lowering drugs, drug dosage, lipid levels, the hospitalization rate and duration up to the end of the third quarter of 2005.
Results
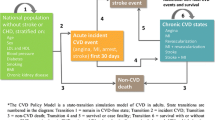
A total of 1,249 patients (median 65 years, 90.5% in the statutory health insurance system, 56.5% male) with a mean BMI of 28.07 were enrolled in the study. Seventy-two percent had CHD, diabetes mellitus, or a history of a cerebrovascular event. After the fixed-price regulation came into effect, atorvastatin was replaced in 71.2% of the patients by another lipid-lowering agent, in 90.6% of cases by another statin. Just 15.3% of the patients received an equivalent dose and 44.5% a lower dose of the alternative statin. In 15.3% the lipid-lowering therapy was discontinued. Cholesterol levels remained constant during continuous atorvastatin therapy (LDL cholesterol 115.5 mg/dl, baseline 116.9 mg/dl); within a few weeks of the treatment being changed, 60.5% of the patients experienced an increase in LDL cholesterol to 124.3 (vs. 116.5 mg/dl), which according to the epidemiologic data was prognostically relevant and unfavorable, as well as an increase in hospitalizations (p = 0.01). The share of patients with LDL cholesterol levels <100 mg/dl fell by more than one third to 24.6%, compared to 34.6% in the group that continued to receive atorvastatin. The key factors influencing a change in treatment were the patients’ insurance status (treatment was changed in 76.6% of statutory health insurance patients and in 19.8% of privately insured patients) and the number of risk factors (the higher the number of risk factors the lower the change rate).

Similar content being viewed by others
References
Baessler A, Fischer M, Huf V, Mell S, Hengstenberg C, Mayer B, Holmer S, Riegger G, Schunkert H (2005) Failure to achieve recommended LDL cholesterol levels by suboptimal statin therapy relates to elevated cardiac event rates. Int J Cardiol 293–298
Baigent C, Keck A, Kearney PM et al (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90.056 participants in 14 randomized trials of statins. Lancet 366:1267–1278
Cohen JC, Boerwinkle E, Mosley TH, Hobbs H (2006) Sequence Variations in PCSK9, Low LDL, and Protection against Coronary Heart Disease. NEJM 354:1264–1272
de Backer G, Ambrosioni E, Borch-Johnsen K et al (2003) European guidelines on cardiovascular disease prevention in clinical practice: third joint task force of European and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of eight societies and by invited experts). Eur J Cardiovasc Prev Rehabil 10:S-1–10
Dietz R, Rauch B (2003) Leitlinie zur Diagnose and Behandlung der chronischen koronaren Herzerkrankung der Deutschen Gesellschaft für Kardiologie-Herz-and Kreislaufforschung (DGK). Z Kardiol 92:501–521
Gesetz zur Modernisierung der gesetzlichen Krankenversicherung (GKV-Modernisierungsgesetz-GMGF) (2004) Bundesgesundheitsblatt Teil I, Nr 55:2190–2258
Law MR, Wald NJ, Rudnicka AR (2003) Quantifying effect of statins on low density lipoprotein cholesterol, ischemic heart disease, and stroke: systematic review and meta-analysis. BMJ 326:1423–1427
Thomas MC, Mann J (1998) Increased thrombotic vascular events after change of statin. Lancet 352:1830–1831
Thomas MC, Mann J, Williams S (1998) The impact of reference pricing on clinical lipid control. NZ Med J 1998; 111:292–294
Acknowledgement
The study was initiated and funded by essex pharma GmbH in 81737 Munich and MSD SHARP & DOHME GmbH in 85540 Haar. It was conducted by CONVENTIS AG in 18182 Rostock. The Institute for Applied Statistics Dr. J. Schnitker GmbH in 33647 Bielefeld carried out the biometric analyses.
Conflict of interest statement
The authors confirm that there are no relevant associations that might pose a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bestehorn, K., Greiner, W. Effects of the introduction of fixed prices for statins on lipid levels in Germany. J Public Health 16, 215–219 (2008). https://doi.org/10.1007/s10389-007-0167-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-007-0167-4