Abstract
Background
Understanding patient preferences in cancer management is essential for shared decision-making. Patient or societal willingness-to-pay (WTP) for desired outcomes in cancer management represents their preferences and values of these outcomes.
Objective
The aim of this systematic review is to critically evaluate how current literature has addressed WTP in relation to cancer treatment and achievement of outcomes.
Methods
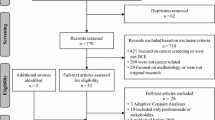
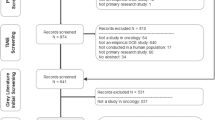
Seven databases were searched from inception until 2 March 2021 to include studies with primary data of WTP values for cancer treatments or achievement of outcomes that were elicited using stated preference methods.
Results
Fifty-four studies were included in this review. All studies were published after year 2000 and more than 90% of the studies were conducted in high-income countries. Sample size of the studies ranged from 35 to 2040, with patient being the most studied population. There was a near even distribution between studies using contingent valuation and discrete choice experiment. Based on the included studies, the highest WTP values were for a quality-adjusted life year (QALY) ($11,498–$589,822), followed by 1-year survival ($3–$198,576), quality of life (QoL) improvement ($5531–$139,499), and pain reduction ($79–$94,662). Current empirical evidence suggested that improvement in QoL and pain reduction had comparable weights to survival in cancer management.
Conclusion
This systematic review provides a summary on stated preference studies that elicited patient preferences via WTP and summarised their respective values. Respondents in this review had comparable WTP for 1-year survival and QoL, suggesting that improvement in QoL should be emphasised together with survival in cancer management.

Similar content being viewed by others
Availability of data and material
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Code availability
Not applicable.
References
Wang, H., Naghavi, M., Allen, C., Barber, R.M., Bhutta, Z.A., Carter, A., et al.: Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 388(10053), 1459–1544 (2016). https://doi.org/10.1016/S0140-6736(16)31012-1
Knaul, F.M., Farmer, P.E., Krakauer, E.L., De Lima, L., Bhadelia, A., Jiang Kwete, X., et al.: Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission report. The Lancet. 391(10128), 1391–1454 (2018). https://doi.org/10.1016/s0140-6736(17)32513-8
Yabroff, K.R., Lund, J., Kepka, D., Mariotto, A.: Economic burden of cancer in the United States: estimates, projections, and future research. Cancer Epidemiol. Biomark. Prev. 20(10), 2006–2014 (2011). https://doi.org/10.1158/1055-9965.EPI-11-0650
Luengo-Fernandez, R., Leal, J., Gray, A., Sullivan, R.: Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 14(12), 1165–1174 (2013). https://doi.org/10.1016/S1470-2045(13)70442-X
Rocque, G.B., Rasool, A., Williams, B.R., Wallace, A.S., Niranjan, S.J., Halilova, K.I., et al.: What is important when making treatment decisions in metastatic breast cancer? A qualitative analysis of decision-making in patients and oncologists. Oncologist. 24(10), 1313–1321 (2019). https://doi.org/10.1634/theoncologist.2018-0711
Kehl, K.L., Landrum, M.B., Arora, N.K., Ganz, P.A., van Ryn, M., Mack, J.W., et al.: Association of actual and preferred decision roles with patient-reported quality of care: shared decision making in cancer care. JAMA Oncol. 1(1), 50–58 (2015). https://doi.org/10.1001/jamaoncol.2014.112
Joosten, E.A.G., DeFuentes-Merillas, L., de Weert, G.H., Sensky, T., van der Staak, C.P.F., de Jong, C.A.J.: Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother. Psychosom. 77(4), 219–226 (2008). https://doi.org/10.1159/000126073
Doyle, C., Lennox, L., Bell, D.: A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 3(1), e001570 (2013). https://doi.org/10.1136/bmjopen-2012-001570
Whitehead, S.J., Ali, S.: Health outcomes in economic evaluation: the QALY and utilities. Br. Med. Bull. 96, 5–21 (2010). https://doi.org/10.1093/bmb/ldq033
Bala, M., Mauskopf, J., Wood, L.: Willingness to pay as a measure of health benefits. Pharmacoeconomics 15(1), 9–18 (1999). https://doi.org/10.2165/00019053-199915010-00002
Olsen, J.A., Smith, R.D.: Theory versus practice: a review of ‘willingness-to-pay’in health and health care. Health Econ. 10(1), 39–52 (2001). https://doi.org/10.1002/1099-1050(200101)10:1%3c39::aid-hec563%3e3.0.co;2-e
Ryan, M., Farrar, S.: Using conjoint analysis to elicit preferences for health care. BMJ 320(7248), 1530–1533 (2000). https://doi.org/10.1136/bmj.320.7248.1530
O’Brien, B., Gafni, A.: When do the" dollars" make sense? Toward a conceptual framework for contingent valuation studies in health care. Med. Decis. Mak. 16(3), 288–299 (1996)
Klose, T.: The contingent valuation method in health care. Health Policy 47(2), 97–123 (1999)
Bridges, J.F.: Stated preference methods in health care evaluation: an emerging methodological paradigm in health economics. Appl. Health. Econ. Health Policy. 2(4), 213–224 (2003)
de Bekker-Grob, E.W., Donkers, B., Bliemer, M.C.J., Veldwijk, J., Swait, J.D.: Can healthcare choice be predicted using stated preference data? Soc. Sci. Med. 246, 112736 (2020). https://doi.org/10.1016/j.socscimed.2019.112736
Morrell, L., Wordsworth, S., Rees, S., Barker, R.: Does the public prefer health gain for cancer patients? A systematic review of public views on cancer and its characteristics. Pharmacoeconomics 35(8), 793–804 (2017). https://doi.org/10.1007/s40273-017-0511-7
Whitty, J.A., Lancsar, E., Rixon, K., Golenko, X., Ratcliffe, J.: A systematic review of stated preference studies reporting public preferences for healthcare priority setting. Patient. 7(4), 365–386 (2014). https://doi.org/10.1007/s40271-014-0063-2
MacLeod, T., Harris, A., Mahal, A.: Stated and revealed preferences for funding new high-cost cancer drugs: a critical review of the evidence from patients, the public and payers. Patient. 9(3), 201–222 (2016). https://doi.org/10.1007/s40271-015-0139-7
Lin, P.J., Cangelosi, M.J., Lee, D.W., Neumann, P.J.: Willingness to pay for diagnostic technologies: a review of the contingent valuation literature. Value Health. 16(5), 797–805 (2013). https://doi.org/10.1016/j.jval.2013.04.005
Mansfield, C., Tangka, F.K., Ekwueme, D.U., Smith, J.L., Guy, G.P., Li, C., et al.: Stated preference for cancer screening: a systematic review of the literature, 1990–2013. Prev. Chronic Dis. 13, E27 (2016). https://doi.org/10.5888/pcd13.150433
Blanchard, P., Volk, R.J., Ringash, J., Peterson, S.K., Hutcheson, K.A., Frank, S.J.: Assessing head and neck cancer patient preferences and expectations: A Systematic review. Oral Oncol. 62, 44–53 (2016). https://doi.org/10.1016/j.oraloncology.2016.09.008
Guerra, R.L., Castaneda, L., de Albuquerque, R.C.R., Ferreira, C.B.T., Correa, F.M., Fernandes, R.R.A., et al.: Patient preferences for breast cancer treatment interventions: a systematic review of discrete choice experiments. Patient. 12(6), 559–569 (2019). https://doi.org/10.1007/s40271-019-00375-w
Sugitani, Y., Sugitani, N., Ono, S.: Quantitative preferences for lung cancer treatment from the patients’ perspective: a systematic review. The Patient Patient-Cent. Outcomes Res. 13(5), 521–536 (2020). https://doi.org/10.1007/s40271-020-00434-7
Schmidt, K., Damm, K., Prenzler, A., Golpon, H., Welte, T.: Preferences of lung cancer patients for treatment and decision-making: a systematic literature review. Eur. J. Cancer Care (Engl). 25(4), 580–591 (2016). https://doi.org/10.1111/ecc.12425
Damm, K., Vogel, A., Prenzler, A.: Preferences of colorectal cancer patients for treatment and decision-making: a systematic literature review. Eur J. Cancer Care. 23(6), 762–772 (2014). https://doi.org/10.1111/ecc.12207
Bath-Hextall, F., Nalubega, S., Evans, C.: The needs and experiences of patients with skin cancer: a qualitative systematic review with metasynthesis. Br J Dermatol. 177(3), 666–687 (2017). https://doi.org/10.1111/bjd.15148
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6(7), e100097 (2009)
The World Bank. World Development Indicators. https://databank.worldbank.org/reports.aspx?source=2&series=NY.GDP.DEFL.ZS. Accessed 2 Sep 2020
Smith, R.D., Sach, T.H.: Contingent valuation: what needs to be done? Health Econ Policy Law. 5(Pt 1), 91–111 (2010). https://doi.org/10.1017/S1744133109990016
Bridges, J.F., Hauber, A.B., Marshall, D., Lloyd, A., Prosser, L.A., Regier, D.A., et al.: Conjoint analysis applications in health-a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 14(4), 403–413 (2011). https://doi.org/10.1016/j.jval.2010.11.013
Benidir, T., Finelli, A., Hamilton, R., Hersey, K., Joshua, A., Kulkarni, G., et al.: Patient understanding regarding end-of-life prostate cancer and perspectives regarding cost/ benefit of current treatment paradigms. J. Urol. 193(4), e929 (2015)
Goldberg, R.J., Jang, R.W., Leighl, N.B.: A willingness-to-pay study of vascular endothelial growth factor inhibitors among patients with advanced non-small cell lung cancer. J. Clin. Oncol. 1, 6581 (2009)
Jo, C.: Using discrete choice experiments to estimate the willingness to pay for cancer treatment in Korea: a general population study. Value Health. 13(3), A46 (2010). https://doi.org/10.1016/S1098-3015%2810%2972208-7
Jo, C.: Using discrete choice experiments to estimate the marginal willingness to pay of insurance premium for lung cancer treatment in Korea. Value Health. 13(7), A515 (2010)
Jo, C., Cho, D.H.: Using discrete choice experiments to estimate the marginal willingness to pay of insurance premium for stomach cancer treatment in Korea. Value Health. 13(3), A46 (2010). https://doi.org/10.1016/S1098-3015%2810%2972207-5
Konstantopoulou, T., Pacheco, R.: Patients’ preferences for breast cancer treatments: results of a discrete choice experiment (Dce) Survey from Spain, France Poland and Ireland. Value Health. 22(Supplement 3), S922–S923 (2019). https://doi.org/10.1016/j.jval.2019.09.2737
Lalla, D., McLaughlin, T., Brammer, M., Bramley, T., Bare, A., Carlton, R.: Willingness to pay for a reduction in risk of treatment side effects in patients with metastatic breast cancer. Value Health. 14(7), A462 (2011). https://doi.org/10.1016/j.jval.2011.08.1251
Liao, C., Yang, M., Hung, Y., Chen, S., Tang, C.: A discrete choice experiment for engaging patients in reimbursement decision making: Patient preferences on adjuvant chemotherapy in breast cancer. Value Health. 18(7), A470 (2015)
Obradovic, M., Mrhar, A., Kos, M.: Willingness to pay for a life-year gained from the perspective of the general population. Value Health. 12(7), A284 (2009)
Sousa, N., Costa, T., Monteiro-Soares, M., Goncalves, F. R., Azevedo, L. F.: Bias in valuation of health care benefits in metastatic prostate cancer: A contingent valuation of willingness to pay. J. Clin. Oncol. Conf. 35(15 Supplement 1) (2017)
Tang, C.: Women’s preferences for breast reconstruction: a study using a discrete choice experiments. Value Health. 15(7), A406 (2012). https://doi.org/10.1016/j.jval.2012.08.1181
Yucel, A., Chase, K., Kumar, R., Fuehrer, D., Bensink, M.: Pcn265 breast cancer patient preference and willingness to pay for granulocyte colony-stimulating factors (G-Csf). Value Health. 22(Supplement 2), S107 (2019). https://doi.org/10.1016/j.jval.2019.04.386
Golda, N., Black, W., Patel, V., Neal, D., Etzkorn, J.: Determining patient preferences and willingness to pay related to scar length and appearance after skin cancer treatment on the face and trunk: a multicenter discrete choice experiment. J. Am. Acad. Dermatol. 81(4), 1011–1013 (2019). https://doi.org/10.1016/j.jaad.2019.01.080
Olofsson, S., Gerdtham, U.G., Hultkrantz, L., Persson, U.: Measuring the end-of-life premium in cancer using individual ex ante willingness to pay. Eur. J. Health Econ. 19(6), 807–820 (2018). https://doi.org/10.1007/s10198-017-0922-6
Bazarbashi, S., De Vol, E.B., Maraiki, F., Al-Jedai, A., Ali, A.A., Alhammad, A.M., et al.: Empirical monetary valuation of a quality-adjusted life-year in the Kingdom of Saudi Arabia: a willingness-to-pay analysis. PharmacoEconomics-Open 4(4), 625–633 (2020). https://doi.org/10.1007/s41669-020-00211-0
Thongprasert, S., Crawford, B., Sakulbumrungsil, R., Chaiyakunapruk, N., Petcharapiruch, S., Leartsakulpanitch, J., et al.: Willingness to pay for lung cancer treatment: Patient versus general public values. Int. J. Technol. Assess. Health Care 31(4), 264–270 (2015). https://doi.org/10.1017/S0266462315000409
Finkelstein, E.A., Bilger, M., Flynn, T.N., Malhotra, C.: Preferences for end-of-life care among community-dwelling older adults and patients with advanced cancer: A discrete choice experiment. Health Policy 119(11), 1482–1489 (2015). https://doi.org/10.1016/j.healthpol.2015.09.001
Fischer, B., Telser, H., Zweifel, P.: End-of-life healthcare expenditure: testing economic explanations using a discrete choice experiment. J. Health Econ. 60, 30–38 (2018). https://doi.org/10.1016/j.jhealeco.2018.06.001
Malhotra, C., Farooqui, M.A., Kanesvaran, R., Bilger, M., Finkelstein, E.: Comparison of preferences for end-of-life care among patients with advanced cancer and their caregivers: a discrete choice experiment. Palliat. Med. 29(9), 842–850 (2015). https://doi.org/10.1177/0269216315578803
Stenehjem, D.D., Au, T.H., Ngorsuraches, S., Ma, J.B.H., Wanishayakorn, T., Nelson, R.S., et al.: Immunotargeted therapy in melanoma: patient, provider preferences, and willingness to pay at an academic cancer center. Melanoma Res. 29(6), 626–634 (2019). https://doi.org/10.1097/CMR.0000000000000572
Ngorsuraches, S., Thongkeaw, K.: Patients’ preferences and willingness-to-pay for postmenopausal hormone receptor-positive, HER2-negative advanced breast cancer treatments after failure of standard treatments. Springerplus 4(1), 674 (2015). https://doi.org/10.1186/s40064-015-1482-9
Sun, H., Wang, H., Xu, N., Li, J., Shi, J., Zhou, N., et al.: Patient preferences for chemotherapy in the treatment of non-small cell lung cancer: A multicenter discrete choice experiment (DCE) study in China. Patient Prefer. Adher. 13, 1701–1709 (2019). https://doi.org/10.2147/PPA.S224529
Lakdawalla, D.N., Romley, J.A., Sanchez, Y., Maclean, J.R., Penrod, J.R., Philipson, T.: How cancer patients value hope and the implications for cost-effectiveness assessments of high-cost cancer therapies. Health Aff. (Millwood). 31(4), 676–682 (2012). https://doi.org/10.1377/hlthaff.2011.1300
Lin, P.-J., Concannon, T.W., Greenberg, D., Cohen, J.T., Rossi, G., Hille, J., et al.: Does framing of cancer survival affect perceived value of care? A willingness-to-pay survey of US residents. Expert Rev. Pharmacoecon. Outcomes Res. 13(4), 513–522 (2013). https://doi.org/10.1586/14737167.2013.814948
Oh, D.Y., Crawford, B., Kim, S.B., Chung, H.C., McDonald, J., Lee, S.Y., et al.: Evaluation of the willingness-to-pay for cancer treatment in Korean metastatic breast cancer patients: A multicenter, cross-sectional study. Asia-Pac. J. Clin. Oncol. 8(3), 282–291 (2012). https://doi.org/10.1111/j.1743-7563.2012.01546.x
Meads, D., O’Dwyer, J., Hulme, C., Chintakayala, P., Vinall-Collier, K., Bennett, M.: Patient preferences for pain management in advanced cancer: results from a discrete choice experiment. Patient. 10(5), 643–651 (2017). https://doi.org/10.1007/s40271-017-0236-x
O’Shea, E., Gannon, B., Kennelly, B.: Eliciting preferences for resource allocation in mental health care in Ireland. Health Policy 88(2–3), 359–370 (2008). https://doi.org/10.1016/j.healthpol.2008.03.018
O'Shea, E., Stewart, J.M., Donaldson, C., Shackley, P. Eliciting preferences for resource allocation in health care. Econ. Soc. Rev. 2001;32(3):217–38. http://www.esr.ie/issue/archive.
Augustin, M., Blome, C., Forschner, A., Gutzmer, R., Hauschild, A., Heinzerling, L., et al.: Willingness to pay for a cure of low-risk melanoma patients in Germany. PLoS ONE (2018). https://doi.org/10.1371/journal.pone.0197780
Franic, D.M., Pathak, D.S., Gafni, A.: Quality-adjusted life years was a poor predictor of women’s willingness to pay in acute and chronic conditions: results of a survey. J. Clin. Epidemiol. 58(3), 291–303 (2005). https://doi.org/10.1016/j.jclinepi.2004.10.005
Lang, H.C., Chang, K., Ying, Y.H.: Quality of life, treatments, and patients’ willingness to pay for a complete remission of cervical cancer in Taiwan. Health Econ. (United Kingdom). 21(10), 1217–1233 (2012). https://doi.org/10.1002/hec.1786
Lang, H.C.: Willingness to pay for lung cancer treatment. Value in Health. 13(6), 743–749 (2010). https://doi.org/10.1111/j.1524-4733.2010.00743.x
Li, C., Zeliadt, S.B., Hall, I.J., Smith, J.L., Ekwueme, D.U., Moinpour, C.M., et al.: Willingness to pay for prostate cancer treatment among patients and their family members at 1 year after diagnosis. Value Health. 15(5), 716–723 (2012). https://doi.org/10.1016/j.jval.2012.03.003
Cho, D., Jo, C.: Preference elicitation approach for measuring the willingness to pay for liver cancer treatment in Korea. Clin Mol Hepatol. 21(3), 268–278 (2015). https://doi.org/10.3350/cmh.2015.21.3.268
Gyldmark, M., Morrison, G.C.: Demand for health care in Denmark: Results of a national sample survey using contingent valuation. Soc. Sci. Med. 53(8), 1023–1036 (2001). https://doi.org/10.1016/S0277-9536%2800%2900398-1
Luchini, S., Protiere, C., Moatti, J.P.: Eliciting several willingness to pay in a single contingent valuation survey: application to health care. Health Econ. 12(1), 51–64 (2003). https://doi.org/10.1002/hec.703
Romley, J.A., Sanchez, Y., Penrod, J.R., Goldman, D.P.: Survey results show that adults are willing to pay higher insurance premiums for generous coverage of specialty drugs. Health Aff. 31(4), 683–690 (2012). https://doi.org/10.1377/hlthaff.2011.1301
Essers, B.A.B., Dirksen, C.D., Prins, M.H., Neumann, H.A.M.: Assessing the public’s preference for surgical treatment of primary basal cell carcinoma: A discrete-choice experiment in the South of the Netherlands. Dermatol. Surg. 36(12), 1950–1955 (2010). https://doi.org/10.1111/j.1524-4725.2010.01805.x
Etzkorn, J.R., Tuttle, S.D., Lim, I., Feit, E.M., Sobanko, J.F., Shin, T.M., et al.: Patients prioritize local recurrence risk over other attributes for surgical treatment of facial melanomas-Results of a stated preference survey and choice-based conjoint analysis. J. Am. Acad. Dermatol. 79(2), 210–9.e3 (2018). https://doi.org/10.1016/j.jaad.2018.02.059
Lee, J.Y., Kim, K., Lee, Y.S., Kim, H.Y., Nam, E.J., Kim, S., et al.: Treatment preferences of advanced ovarian cancer patients for adding bevacizumab to first-line therapy. Gynecol. Oncol. 143(3), 622–627 (2016). https://doi.org/10.1016/j.ygyno.2016.10.021
Lalla, D., Carlton, R., Santos, E., Bramley, T., D’Souza, A.: Willingness to pay to avoid metastatic breast cancer treatment side effects: results from a conjoint analysis. Springerplus 3(1), 350 (2014). https://doi.org/10.1186/2193-1801-3-350
Dranitsaris, G., Leung, P., Ciotti, R., Ortega, A., Spinthouri, M., Liaropoulos, L., et al.: A multinational study to measure the value that patients with cancer place on improved emesis control following cisplatin chemotherapy. Pharmacoeconomics 19(9), 955–967 (2001). https://doi.org/10.2165/00019053-200119090-00007
Miller, P.J.E., Balu, S., Buchner, D., Walker, M.S., Stepanski, E.J., Schwartzberg, L.S.: Willingness to pay to prevent chemotherapy induced nausea and vomiting among patients with breast, lung, or colorectal cancer. J. Med. Econ. 16(10), 1179–1189 (2013). https://doi.org/10.3111/13696998.2013.832257
Johnson, P., Bancroft, T., Barron, R., Legg, J., Li, X., Watson, H., et al.: Discrete choice experiment to estimate breast cancer patients’ preferences and willingness to pay for prophylactic granulocyte colony-stimulating factors. Value Health. 17(4), 380–389 (2014). https://doi.org/10.1016/j.jval.2014.01.002
Teuffel, O., Cheng, S., Ethier, M.C., Diorio, C., Martino, J., Mayo, C., et al.: Health-related quality of life anticipated with different management strategies for febrile neutropenia in adult cancer patients. Support. Care Cancer 20(11), 2755–2764 (2012). https://doi.org/10.1007/s00520-012-1397-8
Bernard, M., Brignone, M., Adehossi, A., Pefoura, S., Briquet, C., Chouaid, C., et al.: Perception of alopecia by patients requiring chemotherapy for non-small-cell lung cancer: A willingness to pay study. Lung Cancer 72(1), 114–118 (2011). https://doi.org/10.1016/j.lungcan.2010.07.004
Regier, D.A., Diorio, C., Ethier, M.C., Alli, A., Alexander, S., Boydell, K.M., et al.: Discrete choice experiment to evaluate factors that influence preferences for antibiotic prophylaxis in pediatric oncology. PLoS ONE (2012). https://doi.org/10.1371/journal.pone.0047470
Ha, T.V., Hoang, M.V., Vu, M.Q., Hoang, N.A.T., Khuong, L.Q., Vu, A.N., et al.: Willingness to pay for a quality-adjusted life year among advanced non-small cell lung cancer patients in Viet Nam, 2018. Medicine (United States). (2020). https://doi.org/10.1097/MD.0000000000019379
Leighl, N.B., Tsao, W.S., Zawisza, D.L., Nematollahi, M., Shepherd, F.A.: A willingness-to-pay study of oral epidermal growth factor tyrosine kinase inhibitors in advanced non-small cell lung cancer. Lung Cancer 51(1), 115–121 (2006). https://doi.org/10.1016/j.lungcan.2005.08.005
Havet, N., Morelle, M., Remonnay, R., Carrere, M.-O.: Cancer patients' willingness to pay for blood transfusions at home: results from a contingent valuation study in a French Cancer Network. Eur. J. Health Econ. 2012;13(3):289–300. https://link.springer.com/journal/volumesAndIssues/10198
Davidson, B.A., Ehrisman, J., Reed, S.D., Yang, J.C., Buchanan, A., Havrilesky, L.J.: Preferences of women with epithelial ovarian cancer for aspects of genetic testing. Gynecol. Oncol. Res. Pract. (2019). https://doi.org/10.1186/s40661-019-0066-8
Aristides, M., Chen, J., Schulz, M., Williamson, E., Clarke, S., Grant, K.: Conjoint analysis of a new Chemotherapy: willingness to pay and preference for the features of raltitrexed versus standard therapy in advanced Colorectal Cancer. Pharmacoeconomics 20(11), 775–784 (2002). https://doi.org/10.2165/00019053-200220110-00006
Erdem, S., Thompson, C.: Prioritising health service innovation investments using public preferences: a discrete choice experiment. BMC Health Serv. Res. 14, 360 (2014). https://doi.org/10.1186/1472-6963-14-360
Najafzadeh, M., Johnston, K.M., Peacock, S.J., Connors, J.M., Marra, M.A., Lynd, L.D., et al.: Genomic testing to determine drug response: measuring preferences of the public and patients using Discrete Choice Experiment (DCE). BMC Health Serv. Res. 13, 454 (2013). https://doi.org/10.1186/1472-6963-13-454
Ngorsuraches, S.T.K.: Breast cancer patients’ preferences and willingness to pay for mtor inhibitors. J Am Pharm Assoc 55(2), e124–e5 (2015). https://doi.org/10.1331/JAPhA.2015.15515
Bien, D.R., Danner, M., Vennedey, V., Civello, D., Evers, S.M., Hiligsmann, M.: Patients’ Preferences for Outcome, Process and Cost Attributes in Cancer Treatment: A Systematic Review of Discrete Choice Experiments. Patient. 10(5), 553–565 (2017). https://doi.org/10.1007/s40271-017-0235-y
Worldwide Palliative Care Alliance. Global Atlas of Palliative Care 2020.
Smith, R.D.: Construction of the contingent valuation market in health care: a critical assessment. Health Econ. 12(8), 609–628 (2003). https://doi.org/10.1002/hec.755
Bayoumi, A.M.: The measurement of contingent valuation for health economics. Pharmacoeconomics 22(11), 691–700 (2004). https://doi.org/10.2165/00019053-200422110-00001
Arrow, K., Solow, R., Portney, P.R., Leamer, E.E., Radner, R., Schuman, H.: Report of the NOAA panel on contingent valuation. Fed. Reg. 58(10), 4601–4614 (1993)
Harrison, G. W. Contingent valuation meets the experts: a critique of the NOAA Panel Report 2002.
Ryan, M., Scott, D.A., Donaldson, C.: Valuing health care using willingness to pay: a comparison of the payment card and dichotomous choice methods. J. Health Econ. 23(2), 237–258 (2004)
Ryan, M., Watson, V., Entwistle, V.: Rationalising the “irrational”: a think aloud study of discrete choice experiment responses. Health Econ. 18(3), 321–336 (2009). https://doi.org/10.1002/hec.1369
Bijlenga, D., Bonsel, G.J., Birnie, E.: Eliciting willingness to pay in obstetrics: comparing a direct and an indirect valuation method for complex health outcomes. Health Econ. 20(11), 1392–1406 (2011). https://doi.org/10.1002/hec.1678
Howard, K., Salkeld, G.: Does attribute framing in discrete choice experiments influence willingness to pay? Results from a discrete choice experiment in screening for colorectal cancer. Value in Health. 12(2), 354–363 (2009). https://doi.org/10.1111/j.1524-4733.2008.00417.x
Hauber, A.B., Gonzalez, J.M., Groothuis-Oudshoorn, C.G., Prior, T., Marshall, D.A., Cunningham, C., et al.: Statistical methods for the analysis of discrete choice experiments: a Report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health. 19(4), 300–315 (2016). https://doi.org/10.1016/j.jval.2016.04.004
Reed Johnson, F., Lancsar, E., Marshall, D., Kilambi, V., Muhlbacher, A., Regier, D.A., et al.: Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 16(1), 3–13 (2013). https://doi.org/10.1016/j.jval.2012.08.2223
Bridges, J.F., Hauber, A.B., Marshall, D., Lloyd, A., Prosser, L.A., Regier, D.A., et al.: Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 14(4), 403–413 (2011). https://doi.org/10.1016/j.jval.2010.11.013
Funding
No external funds supported this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ALSJY, YHL and SLT. The first draft of the manuscript was written by ASJY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Alene Sze Jing Yong, Yi Heng Lim, Ednin Hamzah, Mark Wing Loong Cheong and Siew Li Teoh declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yong, A.S.J., Lim, Y.H., Cheong, M.W.L. et al. Willingness-to-pay for cancer treatment and outcome: a systematic review. Eur J Health Econ 23, 1037–1057 (2022). https://doi.org/10.1007/s10198-021-01407-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-021-01407-9
Keywords
- Systematic review
- Willingness to pay
- Cancer treatment
- Contingent valuation
- Discrete choice experiment
- Stated preference
- Quality of life