Abstract
Background
While patients tend to value their own health state systematically higher than others would rate it, it is less clear whether stated preferences for hypothetical health states differ between persons with and without specific medical conditions. The aim of this study was to determine if specific conditions affect the valuation of health using a generic measure.
Methods
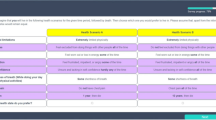
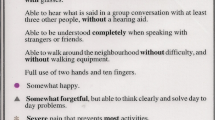
Using data from the US Valuation of EQ-5D Health States (n = 3,773), we focused on six conditions of interest (COI), e.g., arthritis, diabetes, depression, heart failure, cancer, and hay fever, and time trade-off values for 12 of 243 EQ-5D health states. For each COI, regression models compared differences in pooled health state preferences among four groups: COI, COI plus one or more additional conditions, no COI but other conditions, or no chronic conditions.
Results
No differences in health state preferences were found among the four groups for any of the COIs except for patients with cancer and additional conditions, whose mean scores were 0.07 lower compared to no chronic conditions (P < 0.01). The strongest predictors of health state preferences were race/ethnicity, age, and marital status.
Conclusions
Most self-reported chronic conditions had a trivial impact on preferences for hypothetical health states, which suggests that utility algorithms for generic preference-based measures will be similar when estimated from preferences of the general population or patients with chronic illness, conceivably because both types of respondents have not experienced many health states in the classifier system.
Similar content being viewed by others
References
Boyd, N.F., Sutherland, H.J., Heasman, K.Z., Tritchler, D.L., Cummings, B.J.: Whose utilities for decision analysis? Med. Decis. Mak. 10(1), 58–67 (1990)
Chapman, B.P., Franks, P., Duberstein, P.R., Jerant, A.: Differences between individual and societal health state valuations: any link with personality? Med. Care 47(8), 902–907 (2009)
Ubel, P.A., Loewenstein, G., Hershey, J., Baron, J., Mohr, T., Asch, D.A., Jepson, C.: Do nonpatients underestimate the quality of life associated with chronic health conditions because of a focusing illusion? Med. Decis. Mak. 21(3), 190–199 (2001)
Ubel, P.A., Richardson, J., Menzel, P.: Societal value, the person trade-off, and the dilemma of whose values to measure for cost-effectiveness analysis. Health Econ. 9(2), 127–136 (2000)
Dobrez, D., Cella, D., Pickard, A.S., Lai, J.S., Nickolov, A.: Estimation of patient preference-based utility weights from the functional assessment of cancer therapy—general. Value Health 10(4), 266–272 (2007)
Boye, K.S., Matza, L.S., Walter, K.N., Van Brunt, K., Palsgrove, A.C., Tynan, A.: Utilities and disutilities for attributes of injectable treatments for type 2 diabetes. Eur. J. Health Econ. 12(3), 219–230 (2011)
Revicki, D., Margolis, M., Thompson, C., Meltzer, E., Sandor, D., Shaw, J.: Major symptom score utility index for patients with acute rhinosinusitis. Am.J. Rhinol. Allergy 25(3), 99–106 (2011)
Pickard, A.S., Knight, S.J.: Proxy evaluation of health-related quality of life: a conceptual framework for understanding multiple proxy perspectives. Med. Care 43(5), 493–499 (2005)
Sneeuw, K.C., Sprangers, M.A., Aaronson, N.K.: The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease. J. Clin. Epidemiol. 55(11), 1130–1143 (2002)
Dolan, P.: The effect of experience of illness on health state valuations. J. Clin. Epidemiol. 49(5), 551–564 (1996)
Kind, P., Dolan, P.: The effect of past and present illness experience on the valuations of health states. Med. Care 33(Suppl 4), AS255–AS263 (1995)
Krabbe, P.F., Tromp, N., Ruers, T.J., van Riel, P.L.: Are patients’ judgments of health status really different from the general population? Health Qual. Life Outcomes 9, 31 (2011)
Postulart, D., Adang, E.M.: Response shift and adaptation in chronically ill patients. Med. Decis. Mak. 20(2), 186–193 (2000)
Ubel, P.A., Loewenstein, G., Schwarz, N., Smith, D.: Misimagining the unimaginable: the disability paradox and health care decision making. Health Psychol. 24(4 Suppl), S57–S62 (2005)
Albrecht, G.L., Devlieger, P.J.: The disability paradox: high quality of life against all odds. Soc. Sci. Med. 48(8), 977–988 (1999)
Shaw, J., Johnson, J., Chen, S., Levin, J., Coons, S.: Racial/ethnic differences in preferences for the EQ-5D health states: results from the U.S. valuation study. J. Clin. Epidemiol. 60(5), 479–490 (2007)
Rabin, R., de Charro, F.: EQ-5D: a measure of health status from the EuroQol Group. Ann. Med. 33(5), 337–343 (2001)
Shaw, J.W., Johnson, J.A., Coons, S.J.: US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med. Care 43(3), 203–220 (2005)
Pickard, A.S., Neary, M.P., Cella, D.: Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual. Life Outcomes 5, 70 (2007)
Luo, N., Johnson, J., Coons, S.J.: Using instrument-defined health state transitions to estimate minimally important differences for four preference-based health-related quality of life instruments. Med. Care 48(4), 365–371 (2010)
Kahneman, D., Tversky, A.: Prospect theory: an analysis of decision under risk. Econometrica 47(2), 263–292 (1979)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pickard, A.S., Tawk, R. & Shaw, J.W. The effect of chronic conditions on stated preferences for health. Eur J Health Econ 14, 697–702 (2013). https://doi.org/10.1007/s10198-012-0421-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-012-0421-8