Abstract
Although surgical excision of meningioma and its dural base is the most common primary management, skull base meningiomas are quite different, and contemporary management usually consists of multimodal treatment with the aim of achieving the best possible functional outcome and quality of life (QOL) for these patients. As surgery plays an important role in the treatment of skull base meningiomas, it is crucial for neurosurgeons to appreciate the surgical outcome and QOL after meningioma surgery. Outcome is usually measured for meningiomas in terms of morbidity, mortality, time to recurrence, and QOL. The extent of resection, tumor grade, proliferative markers, and tumor location are significant factors in predicting the surgical outcome. Therefore, we address each of these factors in detail in this review. Advances in recent decades in microsurgical techniques, neuroimaging modalities, neuroanesthesia, and perioperative intensive care have substantially improved the surgical outcome; therefore, most surgical outcomes discussed in this review are cited from contemporary literature (2000 to the present) in order to depict the surgical outcome of contemporary microsurgery.

Similar content being viewed by others
References
Abdel-Aziz KM, Froelich SC, Dagnew E, Jean W, Breneman JC, Zuccarello M, van Loveren HR, Tew JM Jr (2004) Large sphenoid wing meningiomas involving the cavernous sinus: conservative surgical strategies for better functional outcomes. Neurosurgery 54(6):1375–1383
Adachi K, Kawase T, Yoshida K, Yazaki T, Onozuka S (2009) Abc surgical risk scale for skull base meningioma: a new scoring system for predicting the extent of tumor removal and neurological outcome. Clinical article. J Neurosurg 111(5):1053–1061. doi:10.3171/2007.11.17446
Aichholzer M, Bertalanffy A, Dietrich W, Roessler K, Pfisterer W, Ungersboeck K, Heimberger K, Kitz K (2000) Gamma knife radiosurgery of skull base meningiomas. Acta Neurochir (Wien) 142(6):647–652
Al-Mefty O (1990) Clinoidal meningiomas. J Neurosurg 73(6):840–849. doi:10.3171/jns.1990.73.6.0840
Arai H, Sato K, Okuda MM, Hishii M, Nakanishi H, Ishii H (2000) Transcranial transsphenoidal approach for tuberculum sellae meningiomas. Acta Neurochir (Wien) 142(7):751–756
Basso A, Carrizo A, Antico J (2006) Sphenoid ridge meningiomas. In: Schmidek HH, Roberts DW (eds) Operative neurosurgical techniques: indications, methods, and results, vol 1, 5. Saunders, Philadelphia, pp 226–237
Arnautovic KI, Al-Mefty O (2002) Primary meningiomas of the jugular fossa. J Neurosurg 97(1):12–20. doi:10.3171/jns.2002.97.1.0012
Arnautovic KI, Al-Mefty O, Husain M (2000) Ventral foramen magnum meninigiomas. J Neurosurg 92(1 Suppl):71–80
Bambakidis NC, Kakarla UK, Kim LJ, Nakaji P, Porter RW, Daspit CP, Spetzler RF (2008) Evolution of surgical approaches in the treatment of petroclival meningiomas: a retrospective review. Neurosurgery 62(6 Suppl 3):1182–1191. doi:10.1227/01.neu.0000333784.04435.65
Bassiouni H, Asgari S, Stolke D (2006) Tuberculum sellae meningiomas: functional outcome in a consecutive series treated microsurgically. Surg Neurol 66(1):37–44. doi:10.1016/j.surneu.2005.11.059
Bassiouni H, Hunold A, Asgari S, Stolke D (2004) Meningiomas of the posterior petrous bone: functional outcome after microsurgery. J Neurosurg 100(6):1014–1024. doi:10.3171/jns.2004.100.6.1014
Bassiouni H, Hunold A, Asgari S, Stolke D (2004) Tentorial meningiomas: clinical results in 81 patients treated microsurgically. Neurosurgery 55(1):108–116
Bassiouni H, Ntoukas V, Asgari S, Sandalcioglu EI, Stolke D, Seifert V (2006) Foramen magnum meningiomas: clinical outcome after microsurgical resection via a posterolateral suboccipital retrocondylar approach. Neurosurgery 59(6):1177–1185. doi:10.1227/01.NEU.0000245629.77968.37
Bertalanffy A, Roessler K, Koperek O, Gelpi E, Prayer D, Neuner M, Knosp E (2006) Intraventricular meningiomas: a report of 16 cases. Neurosurg Rev 29(1):30–35. doi:10.1007/s10143-005-0414-5
Bonnal J, Thibaut A, Brotchi J, Born J (1980) Invading meningiomas of the sphenoid ridge. J Neurosurg 53(5):587–599. doi:10.3171/jns.1980.53.5.0587
Borba LA, de Oliveira JG, Giudicissi-Filho M, Colli BO (2009) Surgical management of foramen magnum meningiomas. Neurosurg Rev 32(1):49–58. doi:10.1007/s10143-008-0161-5
Borovich B, Doron Y (1986) Recurrence of intracranial meningiomas: the role played by regional multicentricity. J Neurosurg 64(1):58–63. doi:10.3171/jns.1986.64.1.0058
Borovich B, Doron Y, Braun J, Guilburd JN, Zaaroor M, Goldsher D, Lemberger A, Gruszkiewicz J, Feinsod M (1986) Recurrence of intracranial meningiomas: the role played by regional multicentricity. Part 2: clinical and radiological aspects. J Neurosurg 65(2):168–171. doi:10.3171/jns.1986.65.2.0168
Boulton MR, Cusimano MD (2003) Foramen magnum meningiomas: concepts, classifications, and nuances. Neurosurg Focus 14(6):e10. doi:10.3171/foc.2003.14.6.10
Bret P, Guyotat J, Madarassy G, Ricci AC, Signorelli F (2000) Tentorial meningiomas. Report on twenty-seven cases. Acta Neurochir (Wien) 142(5):513–526
Bruneau M, George B (2008) Foramen magnum meningiomas: detailed surgical approaches and technical aspects at lariboisiere hospital and review of the literature. Neurosurg Rev 31(1):19–32. doi:10.1007/s10143-007-0097-1
Carvalho GA, Matthies C, Tatagiba M, Eghbal R, Samii M (2000) Impact of computed tomographic and magnetic resonance imaging findings on surgical outcome in petroclival meningiomas. Neurosurgery 47(6):1287–1294
Chicani CF, Miller NR (2003) Visual outcome in surgically treated suprasellar meningiomas. J Neuroophthalmol 23(1):3–10
Ciric I, Landau B (1993) Tentorial and posterior cranial fossa meningiomas: operative results and long-term follow-up: experience with twenty-six cases. Surg Neurol 39(6):530–537
Colli BO, Assirati JA Jr, Deriggi DJ, Neder L, dos Santos AC, Carlotti CG Jr (2008) Tentorial meningiomas: follow-up review. Neurosurg Rev 31(4):421–430. doi:10.1007/s10143-008-0141-9
Condra KS, Buatti JM, Mendenhall WM, Friedman WA, Marcus RB Jr, Rhoton AL (1997) Benign meningiomas: primary treatment selection affects survival. Int J Radiat Oncol Biol Phys 39(2):427–436
Couldwell WT, Weiss MH, Rabb C, Liu JK, Apfelbaum RI, Fukushima T (2004) Variations on the standard transsphenoidal approach to the sellar region, with emphasis on the extended approaches and parasellar approaches: surgical experience in 105 cases. Neurosurgery 55(3):539–547
Cudlip SA, Wilkins PR, Johnston FG, Moore AJ, Marsh HT, Bell BA (1998) Posterior fossa meningiomas: surgical experience in 52 cases. Acta Neurochir (Wien) 140(10):1007–1012
Cusimano MD, Sekhar LN, Sen CN, Pomonis S, Wright DC, Biglan AW, Jannetta PJ (1995) The results of surgery for benign tumors of the cavernous sinus. Neurosurgery 37(1):1–9
de Divitiis E, Esposito F, Cappabianca P, Cavallo LM, de Divitiis O (2008) Tuberculum sellae meningiomas: high route or low route? A series of 51 consecutive cases. Neurosurgery 62(3):556–563. doi:10.1227/01.neu.0000317303.93460.24
De Jesus O, Sekhar LN, Parikh HK, Wright DC, Wagner DP (1996) Long-term follow-up of patients with meningiomas involving the cavernous sinus: recurrence, progression, and quality of life. Neurosurgery 39(5):915–919
DeMonte F, Smith HK, al-Mefty O (1994) Outcome of aggressive removal of cavernous sinus meningiomas. J Neurosurg 81(2):245–251. doi:10.3171/jns.1994.81.2.0245
Dijkstra M, van Nieuwenhuizen D, Stalpers LJ, Wumkes M, Waagemans M, Vandertop WP, Heimans JJ, Leenstra S, Dirven CM, Reijneveld JC, Klein M (2009) Late neurocognitive sequelae in patients with who grade I meningioma. J Neurol Neurosurg Psychiatry 80(8):910–915. doi:10.1136/jnnp.2007.138925
Dziuk TW, Woo S, Butler EB, Thornby J, Grossman R, Dennis WS, Lu H, Carpenter LS, Chiu JK (1998) Malignant meningioma: an indication for initial aggressive surgery and adjuvant radiotherapy. J Neurooncol 37(2):177–188
Eustacchio S, Trummer M, Fuchs I, Schrottner O, Sutter B, Pendl G (2002) Preservation of cranial nerve function following gamma knife radiosurgery for benign skull base meningiomas: experience in 121 patients with follow-up of 5 to 9.8 years. Acta Neurochir Suppl 84:71–76
Fahlbusch R, Schott W (2002) Pterional surgery of meningiomas of the tuberculum sellae and planum sphenoidale: surgical results with special consideration of ophthalmological and endocrinological outcomes. J Neurosurg 96(2):235–243. doi:10.3171/jns.2002.96.2.0235
Gerszten PC (1998) Outcomes research: a review. Neurosurgery 43(5):1146–1156
Gilbert ME, Shelton C, McDonald A, Salzman KL, Harnsberger HR, Sharma PK, Jensen RL (2004) Meningioma of the jugular foramen: glomus jugulare mimic and surgical challenge. Laryngoscope 114(1):25–32. doi:10.1097/00005537-200401000-00004
Goel A, Desai K, Muzumdar D (2001) Surgery on anterior foramen magnum meningiomas using a conventional posterior suboccipital approach: a report on an experience with 17 cases. Neurosurgery 49(1):102–106
Goel A, Muzumdar D, Desai KI (2002) Tuberculum sellae meningioma: a report on management on the basis of a surgical experience with 70 patients. Neurosurgery 51(6):1358–1363
Gokalp HZ, Arasil E, Erdogan A, Egemen N, Deda H, Cerci A (1995) Tentorial meningiomas. Neurosurgery 36(1):46–51
Guidetti B, Ciappetta P, Domenicucci M (1988) Tentorial meningiomas: surgical experience with 61 cases and long-term results. J Neurosurg 69(2):183–187. doi:10.3171/jns.1988.69.2.0183
Harrison MJ, al-Mefty O (1997) Tentorial meningiomas. Clin Neurosurg 44:451–466
Heim E, Valach L, Schaffner L (1997) Coping and psychosocial adaptation: longitudinal effects over time and stages in breast cancer. Psychosom Med 59(4):408–418
Heimans JJ, Taphoorn MJ (2002) Impact of brain tumour treatment on quality of life. J Neurol 249(8):955–960. doi:10.1007/s00415-002-0839-5
Hentschel SJ, DeMonte F (2003) Olfactory groove meningiomas. Neurosurg Focus 14(6):e4. doi:10.3171/foc.2003.14.6.4
Henzel M, Gross MW, Hamm K, Surber G, Kleinert G, Failing T, Strassmann G, Engenhart-Cabillic R (2006) Significant tumor volume reduction of meningiomas after stereotactic radiotherapy: results of a prospective multicenter study. Neurosurgery 59(6):1188–1194. doi:10.1227/01.NEU.0000245626.93215.F6
Ho DM, Hsu CY, Ting LT, Chiang H (2002) Histopathology and MIB-1 labeling index predicted recurrence of meningiomas: a proposal of diagnostic criteria for patients with atypical meningioma. Cancer 94(5):1538–1547. doi:10.1002/cncr.10351
Jallo GI, Benjamin V (2002) Tuberculum sellae meningiomas: microsurgical anatomy and surgical technique. Neurosurgery 51(6):1432–1439
Joung H, Lee BS (2008) The novel “class” algorithmic scale for patient selection in meningioma surgery. In: Lee JH (ed) Meningiomas: diagnosis, treatment, and outcome. Springer, Berlin
Jung HW, Yoo H, Paek SH, Choi KS (2000) Long-term outcome and growth rate of subtotally resected petroclival meningiomas: experience with 38 cases. Neurosurgery 46(3):567–574
Kalkanis SN, Quinones-Hinojosa A, Buzney E, Ribaudo HJ, Black PM (2000) Quality of life following surgery for intracranial meningiomas at Brigham and Women's Hospital: a study of 164 patients using a modification of the functional assessment of cancer therapy-brain questionnaire. J Neurooncol 48(3):233–241
Kandenwein JA, Richter HP, Antoniadis G (2009) Foramen magnum meningiomas—experience with the posterior suboccipital approach. Br J Neurosurg 23(1):33–39. doi:10.1080/02688690802545932
Ketter R, Rahnenfuhrer J, Henn W, Kim YJ, Feiden W, Steudel WI, Zang KD, Urbschat S (2008) Correspondence of tumor localization with tumor recurrence and cytogenetic progression in meningiomas. Neurosurgery 62(1):61–69. doi:10.1227/01.NEU.0000311062.72626.D6
Kinjo T, al-Mefty O, Kanaan I (1993) Grade zero removal of supratentorial convexity meningiomas. Neurosurgery 33(3):394–399
Kleihues P, Burger PC, Scheithauer BW (1993) The new who classification of brain tumours. Brain Pathol 3(3):255–268
Knosp E, Perneczky A, Koos WT, Fries G, Matula C (1996) Meningiomas of the space of the cavernous sinus. Neurosurgery 38(3):434–442
Kondziolka D, Mathieu D, Lunsford LD, Martin JJ, Madhok R, Niranjan A, Flickinger JC (2008) Radiosurgery as definitive management of intracranial meningiomas. Neurosurgery 62(1):53–58. doi:10.1227/01.NEU.0000311061.72626.0D
Krupp W, Klein C, Koschny R, Holland H, Seifert V, Meixensberger J (2009) Assessment of neuropsychological parameters and quality of life to evaluate outcome in patients with surgically treated supratentorial meningiomas. Neurosurgery 64(1):40–47. doi:10.1227/01.NEU.0000336330.75381.39
Lang DA, Neil-Dwyer G, Garfield J (1999) Outcome after complex neurosurgery: the caregiver's burden is forgotten. J Neurosurg 91(3):359–363. doi:10.3171/jns.1999.91.3.0359
Larson JJ, van Loveren HR, Balko MG, Tew JM Jr (1995) Evidence of meningioma infiltration into cranial nerves: clinical implications for cavernous sinus meningiomas. J Neurosurg 83(4):596–599. doi:10.3171/jns.1995.83.4.0596
Lee JH, Jeun SS, Evans J, Kosmorsky G (2001) Surgical management of clinoidal meningiomas. Neurosurgery 48(5):1012–1019
Little KM, Friedman AH, Sampson JH, Wanibuchi M, Fukushima T (2005) Surgical management of petroclival meningiomas: defining resection goals based on risk of neurological morbidity and tumor recurrence rates in 137 patients. Neurosurgery 56(3):546–559
Margalit NS, Lesser JB, Singer M, Sen C (2005) Lateral approach to anterolateral tumors at the foramen magnum: factors determining surgical procedure. Neurosurgery 56(2 Suppl):324–336
Maruyama K, Shin M, Kurita H, Kawahara N, Morita A, Kirino T (2004) Proposed treatment strategy for cavernous sinus meningiomas: a prospective study. Neurosurgery 55(5):1068–1075
Mathiesen T, Lindquist C, Kihlstrom L, Karlsson B (1996) Recurrence of cranial base meningiomas. Neurosurgery 39(1):2–7
Mendenhall WM, Morris CG, Amdur RJ, Foote KD, Friedman WA (2003) Radiotherapy alone or after subtotal resection for benign skull base meningiomas. Cancer 98(7):1473–1482. doi:10.1002/cncr.11645
Miller E, Crockard HA (1987) Transoral transclival removal of anteriorly placed meningiomas at the foramen magnum. Neurosurgery 20(6):966–968
Mirimanoff RO, Dosoretz DE, Linggood RM, Ojemann RG, Martuza RL (1985) Meningioma: analysis of recurrence and progression following neurosurgical resection. J Neurosurg 62(1):18–24. doi:10.3171/jns.1985.62.1.0018
Molony TB, Brackmann DE, Lo WW (1992) Meningiomas of the jugular foramen. Otolaryngol Head Neck Surg 106(2):128–136
Nakamura M, Roser F, Dormiani M, Matthies C, Vorkapic P, Samii M (2005) Facial and cochlear nerve function after surgery of cerebellopontine angle meningiomas. Neurosurgery 57(1):77–90
Nakamura M, Roser F, Jacobs C, Vorkapic P, Samii M (2006) Medial sphenoid wing meningiomas: clinical outcome and recurrence rate. Neurosurgery 58(4):626–639. doi:10.1227/01.NEU.0000197104.78684.5D
Nakamura M, Roser F, Mirzai S, Matthies C, Vorkapic P, Samii M (2004) Meningiomas of the internal auditory canal. Neurosurgery 55(1):119–127
Nakamura M, Roser F, Struck M, Vorkapic P, Samii M (2006) Tuberculum sellae meningiomas: clinical outcome considering different surgical approaches. Neurosurgery 59(5):1019–1028. doi:10.1227/01.NEU.0000245600.92322.06
Nakamura M, Struck M, Roser F, Vorkapic P, Samii M (2008) Olfactory groove meningiomas: clinical outcome and recurrence rates after tumor removal through the frontolateral and bifrontal approach. Neurosurgery 62(6 Suppl 3):1224–1232. doi:10.1227/01.neu.0000333788.83349.1e
Nanda A, Vincent DA, Vannemreddy PS, Baskaya MK, Chanda A (2002) Far-lateral approach to intradural lesions of the foramen magnum without resection of the occipital condyle. J Neurosurg 96(2):302–309. doi:10.3171/jns.2002.96.2.0302
Natarajan SK, Sekhar LN, Schessel D, Morita A (2007) Petroclival meningiomas: multimodality treatment and outcomes at long-term follow-up. Neurosurgery 60(6):965–979. doi:10.1227/01.NEU.0000255472.52882.D6
Neil-Dwyer G, Lang DA, Davis A (2000) Outcome from complex neurosurgery: an evidence based approach. Acta Neurochir (Wien) 142(4):367–371
Niranjan A, Lunsford LD, Flickinger JC, Maitz A, Kondziolka D (1999) Dose reduction improves hearing preservation rates after intracanalicular acoustic tumor radiosurgery. Neurosurgery 45(4):753–762
Nozaki K, Kikuta K, Takagi Y, Mineharu Y, Takahashi JA, Hashimoto N (2008) Effect of early optic canal unroofing on the outcome of visual functions in surgery for meningiomas of the tuberculum sellae and planum sphenoidale. Neurosurgery 62(4):839–844. doi:10.1227/01.neu.0000318169.75095.cb
O'Sullivan MG, van Loveren HR, Tew JM Jr (1997) The surgical resectability of meningiomas of the cavernous sinus. Neurosurgery 40(2):238–244
Obeid F, Al-Mefty O (2003) Recurrence of olfactory groove meningiomas. Neurosurgery 53(3):534–542
Oghalai JS, Leung MK, Jackler RK, McDermott MW (2004) Transjugular craniotomy for the management of jugular foramen tumors with intracranial extension. Otol Neurotol 25(4):570–579
Pamir MN, Ozduman K, Belirgen M, Kilic T, Ozek MM (2005) Outcome determinants of pterional surgery for tuberculum sellae meningiomas. Acta Neurochir (Wien) 147(11):1121–1130. doi:10.1007/s00701-005-0625-0
Park CK, Jung HW, Kim JE, Paek SH, Kim DG (2006) The selection of the optimal therapeutic strategy for petroclival meningiomas. Surg Neurol 66(2):160–165. doi:10.1016/j.surneu.2005.12.024
Park CK, Jung HW, Yang SY, Seol HJ, Paek SH, Kim DG (2006) Surgically treated tuberculum sellae and diaphragm sellae meningiomas: the importance of short-term visual outcome. Neurosurgery 59(2):238–243. doi:10.1227/01.NEU.0000223341.08402.C5
Perry A, Banerjee R, Lohse CM, Kleinschmidt-DeMasters BK, Scheithauer BW (2002) A role for chromosome 9p21 deletions in the malignant progression of meningiomas and the prognosis of anaplastic meningiomas. Brain Pathol 12(2):183–190
Perry A, Scheithauer BW, Stafford SL, Lohse CM, Wollan PC (1999) “Malignancy” in meningiomas: a clinicopathologic study of 116 patients, with grading implications. Cancer 85(9):2046–2056. doi:10.1002/(SICI)1097-0142(19990501)85:9<2046::AID-CNCR23>3.0.CO;2-M
Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM (1997) Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol 21(12):1455–1465
Pichierri A, Santoro A, Raco A, Paolini S, Cantore G, Delfini R (2009) Cavernous sinus meningiomas: retrospective analysis and proposal of a treatment algorithm. Neurosurgery 64(6):1090–1099. doi:10.1227/01.NEU.0000346023.52541.0A
Pollock BE, Stafford SL, Link MJ (2000) Gamma knife radiosurgery for skull base meningiomas. Neurosurg Clin N Am 11(4):659–666
Pollock BE, Stafford SL, Utter A, Giannini C, Schreiner SA (2003) Stereotactic radiosurgery provides equivalent tumor control to simpson grade 1 resection for patients with small- to medium-size meningiomas. Int J Radiat Oncol Biol Phys 55(4):1000–1005. doi:10.1016/S0360-3016(02)04356-0
Puzzilli F, Ruggeri A, Mastronardi L, Agrillo A, Ferrante L (1999) Anterior clinoidal meningiomas: report of a series of 33 patients operated on through the pterional approach. Neuro Oncol 1(3):188–195
Quinones-Hinojosa A, Chang EF, McDermott MW (2003) Falcotentorial meningiomas: clinical, neuroimaging, and surgical features in six patients. Neurosurg Focus 14(6):e11. doi:10.3171/foc.2003.14.6.11
Ramina R, Neto MC, Fernandes YB, Aguiar PH, de Meneses MS, Torres LF (2006) Meningiomas of the jugular foramen. Neurosurg Rev 29(1):55–60. doi:10.1007/s10143-005-0415-4
Reijneveld JC, Sitskoorn MM, Klein M, Nuyen J, Taphoorn MJ (2001) Cognitive status and quality of life in patients with suspected versus proven low-grade gliomas. Neurology 56(5):618–623
Roberti F, Sekhar LN, Kalavakonda C, Wright DC (2001) Posterior fossa meningiomas: surgical experience in 161 cases. Surg Neurol 56(1):8–20. doi:10.1016/S0090-3019(01)00479-7
Roser F, Nakamura M, Dormiani M, Matthies C, Vorkapic P, Samii M (2005) Meningiomas of the cerebellopontine angle with extension into the internal auditory canal. J Neurosurg 102(1):17–23. doi:10.3171.jns.2005.102.1.0017
Roser F, Nakamura M, Jacobs C, Vorkapic P, Samii M (2005) Sphenoid wing meningiomas with osseous involvement. Surg Neurol 64(1):37–43. doi:10.1016/j.surneu.2004.08.092
Russell SM, Benjamin V (2008) Medial sphenoid ridge meningiomas: classification, microsurgical anatomy, operative nuances, and long-term surgical outcome in 35 consecutive patients. Neurosurgery 62(6 Suppl 3):1169–1181. doi:10.1227/01.neu.0000333783.96810.58
Sachsenheimer W, Bimmler T (1992) Assessment of quality of survival in patients with surgically treated meningioma. Neurochirurgia (Stuttg) 35(5):133–136
Sachsenheimer W, Piotrowski W, Bimmler T (1992) Quality of life in patients with intracranial tumors on the basis of Karnofsky's performance status. J Neurooncol 13(2):177–181
Samii M, Carvalho GA, Tatagiba M, Matthies C, Vorkapic P (1996) Meningiomas of the tentorial notch: surgical anatomy and management. J Neurosurg 84(3):375–381. doi:10.3171/jns.1996.84.3.0375
Sanna M, Bacciu A, Falcioni M, Taibah A, Piazza P (2007) Surgical management of jugular foramen meningiomas: a series of 13 cases and review of the literature. Laryngoscope 117(10):1710–1719. doi:10.1097/MLG.0b013e3180cc20a3
Schick U, Hassler W (2005) Surgical management of tuberculum sellae meningiomas: involvement of the optic canal and visual outcome. J Neurol Neurosurg Psychiatry 76(7):977–983. doi:10.1136/jnnp.2004.039974
Seifert V, Raabe A, Zimmermann M (2003) Conservative (labyrinth-preserving) transpetrosal approach to the clivus and petroclival region—indications, complications, results and lessons learned. Acta Neurochir (Wien) 145(8):631–642. doi:10.1007/s00701-003-0086-2
Sekhar LN, Jannetta PJ, Maroon JC (1984) Tentorial meningiomas: surgical management and results. Neurosurgery 14(3):268–275
Sekhar LN, Wright DC, Richardson R, Monacci W (1996) Petroclival and foramen magnum meningiomas: surgical approaches and pitfalls. J Neurooncol 29(3):249–259
Simpson D (1957) The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry 20(1):22–39
Spektor S, Valarezo J, Fliss DM, Gil Z, Cohen J, Goldman J, Umansky F (2005) Olfactory groove meningiomas from neurosurgical and ear, nose, and throat perspectives: approaches, techniques, and outcomes. Neurosurgery 57(4 Suppl):268–280. doi:10.1227/01.NEU.0000176409.70668.EB
Stafford SL, Pollock BE, Foote RL, Link MJ, Gorman DA, Schomberg PJ, Leavitt JA (2001) Meningioma radiosurgery: tumor control, outcomes, and complications among 190 consecutive patients. Neurosurgery 49(5):1029–1037
Tobias S, Kim CH, Kosmorsky G, Lee JH (2003) Management of surgical clinoidal meningiomas. Neurosurg Focus 14(6):e5. doi:10.3171/foc.2003.14.6.5
Tuniz F, Soltys SG, Choi CY, Chang SD, Gibbs IC, Fischbein NJ, Adler JR Jr (2009) Multisession cyberknife stereotactic radiosurgery of large, benign cranial base tumors: preliminary study. Neurosurgery 65(5):898–907. doi:10.1227/01.NEU.0000359316.34041.A8
Voss NF, Vrionis FD, Heilman CB, Robertson JH (2000) Meningiomas of the cerebellopontine angle. Surg Neurol 53(5):439–446. doi:10.1016/S0090-3019(00)00195-6
Walsh MT, Couldwell WT (2009) Management options for cavernous sinus meningiomas. J Neurooncol 92(3):307–316. doi:10.1007/s11060-009-9824-5
Welge-Luessen A, Temmel A, Quint C, Moll B, Wolf S, Hummel T (2001) Olfactory function in patients with olfactory groove meningioma. J Neurol Neurosurg Psychiatry 70(2):218–221
Wu ZB, Yu CJ, Guan SS (2005) Posterior petrous meningiomas: 82 cases. J Neurosurg 102(2):284–289. doi:10.3171/jns.2005.102.2.0284
Wyrwich KW, Bullinger M, Aaronson N, Hays RD, Patrick DL, Symonds T (2005) Estimating clinically significant differences in quality of life outcomes. Qual Life Res 14(2):285–295
Zachenhofer I, Wolfsberger S, Aichholzer M, Bertalanffy A, Roessler K, Kitz K, Knosp E (2006) Gamma-knife radiosurgery for cranial base meningiomas: experience of tumor control, clinical course, and morbidity in a follow-up of more than 8 years. Neurosurgery 58(1):28–36
Zevgaridis D, Medele RJ, Muller A, Hischa AC, Steiger HJ (2001) Meningiomas of the sellar region presenting with visual impairment: impact of various prognostic factors on surgical outcome in 62 patients. Acta Neurochir (Wien) 143(5):471–476
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Michael W. McDermott, San Francisco, USA
The authors have provided a very nice review of the literature since 2000, indicating that challenges remain in the management of the most common primary brain tumor in adults, a meningioma. Not since Cushing first wrote about the significant difficulties these tumors present to the surgeon in 1939 have we been able to provide patients with a definitive surgical cure and acceptable morbidity for our efforts. At our institution, we have published on our own series to document, like the authors here, what the current status of surgical and radiosurgical treatment is (see attached references below; none include in the current paper). Still, many of our efforts are associated with not insignificant morbidity and residual chance for recurrence. Compared to 20 years ago, the neurosurgical community has for the most part accepted that the maximal “safe” resection, followed by observation or adjuvant therapy, provides patients with a better quality of life than attempting complete tumor removal. Soon I suspect that not only the patients, but medical insurers, medical review boards, and government-run health systems will dictate some of the options for treatment for our patients. If we can prove with quality of life follow-up studies and not just freedom from progression or overall survival data that our surgical treatment leaves the patients able to live a nearly normal life postoperatively, then our future surgical endeavors will continue to advance.
References
1. Kane AJ, Sughrue ME, Rutkowski MJ, Shangari G, Fang S, McDermott MW, Berger MS, Parsa AT (2001) Anatomic location is a risk factor for atypical and malignant meningiomas. Cancer 117(6):1272–1278 (Mar 15). doi:10.1002/cncr.25591. Epub 2010 Nov 8. PMID: 21381014 [PubMed—in process]. Related citations
2. Sughrue ME, Rutkowski MJ, Shangari G, Fang S, Parsa AT, Berger MS, McDermott MW (2011) Incidence, risk factors, and outcome of venous infarction after meningioma surgery in 705 patients. J Clin Neurosci 18(5):628–632 (May). Epub 2011 Feb 23. PMID: 21349725 [PubMed—in process]. Related citations
3. Kane AJ, Sughrue ME, Rutkowski MJ, Shangari G, Fang S, McDermott MW, Berger MS, Parsa AT (2010) Anatomic location is a risk factor for atypical and malignant meningiomas. Cancer (Nov 8). [Epub ahead of print]. PMID: 21061397 [PubMed—as supplied by publisher]. Related citations
4. Zlotnick D, Kalkanis SN, Quinones-Hinojosa A, Chung K, Linskey ME, Jensen RL, DeMonte F, Barker FG, Racine CA, Berger MS, Black PM, Cusimano M, Sekhar LN, Parsa A, Aghi M, McDermott MW (2010) FACT-MNG: tumor site specific web-based outcome instrument for meningioma patients. J Neurooncol 99(3):423–431 (Sep). Epub 2010 Sep 18. Review. PMID: 20853019 [PubMed—indexed for MEDLINE] Free PMC Article. Free full text. Related citations
5. Sughrue ME, Rutkowski MJ, Shangari G, Chang HQ, Parsa AT, Berger MS, McDermott MW (2011) Risk factors for the development of serious medical complications after resection of meningiomas. J Neurosurg 114(3):697–704 (Mar). Epub 2010 Jul 23. PMID: 20653395 [PubMed—in process]. Related citations
6. Sughrue ME, Rutkowski MJ, Chang EF, Shangari G, Kane AJ, McDermott MW, Berger MS, Parsa AT (2011) Postoperative seizures following the resection of convexity meningiomas: are prophylactic anticonvulsants indicated? J Neurosurg 114(3):705–709 (Mar). Epub 2010 Jun 25. PMID: 20578801 [PubMed—in process]. Related citations
7. Sughrue ME, Cage T, Shangari G, Parsa AT, McDermott MW (2010) Clinical characteristics and surgical outcomes of patients presenting with meningiomas arising predominantly from the floor of the middle fossa. Neurosurgery 67(1):80–86; discussion 86 (Jul). PMID: 20559094 [PubMed—in process]. Related citations
8. Sughrue ME, Rutkowski MJ, Aranda D, Barani IJ, McDermott MW, Parsa AT (2010) Factors affecting outcome following treatment of patients with cavernous sinus meningiomas. J Neurosurg 113(5):1087–1092 (Nov). Epub 2010 May 7. PMID: 20450274 [PubMed—indexed for MEDLINE]. Related citations
9. Sughrue ME, Rutkowski MJ, Aranda D, Barani IJ, McDermott MW, Parsa AT (2010) Treatment decision making based on the published natural history and growth rate of small meningiomas. J Neurosurg 113(5):1036–1042 (Nov). Epub 2010 Apr 30. Review. PMID: 20433281 [PubMed—indexed for MEDLINE]. Related citations
10. Sughrue ME, Kane AJ, Shangari G, Parsa AT, Berger MS, McDermott MW (2010) Prevalence of previous extracranial malignancies in a series of 1228 patients presenting with meningioma. J Neurosurg 113(5):1115–1121 (Nov). Epub 2010 Apr 30. PMID: 20433279 [PubMed—indexed for MEDLINE]. Related citations
11. Sughrue ME, Kane AJ, Shangari G, Rutkowski MJ, McDermott MW, Berger MS, Parsa AT (2010) The relevance of Simpson grade I and II resection in modern neurosurgical treatment of World Health Organization grade I meningiomas. J Neurosurg 113(5):1029–1035 (Nov). Epub 2010 Apr 9. PMID: 20380529 [PubMed—indexed for MEDLINE]. Related citations
12. Sughrue ME, Sanai N, Shangari G, Parsa AT, Berger MS, McDermott MW (2010) Outcome and survival following primary and repeat surgery for World Health Organization grade III meningiomas. J Neurosurg 113(2):202–209 (Aug). PMID: 20225922 [PubMed—indexed for MEDLINE]. Related citations
13. Sanai N, McDermott MW (2010) A modified far-lateral approach for large or giant meningiomas of the posterior fossa. J Neurosurg 112(5):907–912 (May). PMID: 19877805 [PubMed—indexed for MEDLINE]. Related citations
14. Quiñones-Hinojosa A, Kaprealian T, Chaichana KL, Sanai N, Parsa AT, Berger MS, McDermott MW (2009) Pre-operative factors affecting resectability of giant intracranial meningiomas. Can J Neurol Sci 36(5):623–630 (Sep). PMID: 19831133 [PubMed—indexed for MEDLINE]. Related citations
15. Sanai N, Sughrue ME, Shangari G, Chung K, Berger MS, McDermott MW (2010) Risk profile associated with convexity meningioma resection in the modern neurosurgical era. J Neurosurg 112(5):913–919 (May). PMID: 19645533 [PubMed—indexed for MEDLINE]. Related citations
16. Cage TA, Lamborn KR, Ware ML, Frankfurt A, Chakalian L, Berger MS, McDermott MW (2009) Adjuvant enoxaparin therapy may decrease the incidence of postoperative thrombotic events though does not increase the incidence of postoperative intracranial hemorrhage in patients with meningiomas. J Neurooncol 93(1):151–156 (May). Epub 2009 May 9. PMID: 19430892 [PubMed—indexed for MEDLINE]. Related citations
17. Quiñones-Hinojosa A, Chang EF, Chaichana KL, McDermott MW (2009) Surgical considerations in the management of falcotentorial meningiomas: advantages of the bilateral occipital transtentorial/transfalcine craniotomy for large tumors. Neurosurgery 64(5 Suppl 2):260–268; discussion 268 (May). PMID: 19287325 [PubMed—indexed for MEDLINE]. Related citations
18. Smith JS, Lal A, Harmon-Smith M, Bollen AW, McDermott MW (2007) Association between absence of epidermal growth factor receptor immunoreactivity and poor prognosis in patients with atypical meningioma. J Neurosurg 106(6):1034–1040 (Jun). PMID: 17564176 [PubMed—indexed for MEDLINE]. Related citations
19. Chi JH, Parsa AT, Berger MS, Kunwar S, McDermott MW (2006) Extended bifrontal craniotomy for midline anterior fossa meningiomas: minimization of retraction-related edema and surgical outcomes. Neurosurgery 59(4 Suppl 2):ONS426–ONS433; discussion ONS433–ONS434 (Oct). PMID: 17041513 [PubMed—indexed for MEDLINE]. Related citations
20. Chi JH, McDermott MW (2003) Tuberculum sellae meningiomas. Neurosurg Focus 14(6):e6 (Jun 15). PMID: 15669791 [PubMed—indexed for MEDLINE]. Related citations
21. Quinones-Hinojosa A, Chang EF, McDermott MW (2003) Falcotentorial meningiomas: clinical, neuroimaging, and surgical features in six patients. Neurosurg Focus 14(6):e11 (Jun 15). Review. PMID: 15669786 [PubMed—indexed for MEDLINE]. Related citations
22. McDermott MW (2003) Intraventricular meningiomas. Neurosurg Clin N Am 14(4):559–569 (Oct). Review. PMID: 15024801 [PubMed—indexed for MEDLINE]. Related citations
23. Ware ML, Larson DA, Sneed PK, Wara WW, McDermott MW (2004) Surgical resection and permanent brachytherapy for recurrent atypical and malignant meningioma. Neurosurgery 54(1):55–63; discussion 63–64 (Jan). PMID: 14683541 [PubMed—indexed for MEDLINE]. Related citations
24. Chun JY, McDermott MW, Lamborn KR, Wilson CB, Higashida R, Berger MS (2002) Delayed surgical resection reduces intraoperative blood loss for embolized meningiomas. Neurosurgery 50(6):1231–1235; discussion 1235–1237 (Jun). PMID: 12015840 [PubMed—indexed for MEDLINE]. Related citations
25. Ojemann SG, Sneed PK, Larson DA, Gutin PH, Berger MS, Verhey L, Smith V, Petti P, Wara W, Park E, McDermott MW (2000) Radiosurgery for malignant meningioma: results in 22 patients. J Neurosurg 93(Suppl 3):62–67 (Dec). PMID: 11143265 [PubMed—indexed for MEDLINE]. Related citations
Kenji Ohata, Osaka, Japan
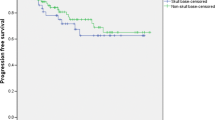
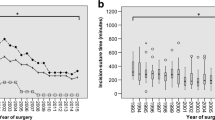
The authors reviewed the contemporary literature regarding the surgical outcome and quality of life after the surgery of skull base meningiomas in different locations. Their endeavor of reviewing 120 articles is worthy of praise and very informative. In the history of the treatment of skull base meningioma, the advancement of skull base surgery in the 1980s greatly contributed to the surgical resectability of the basal meningioma even from the complex area including cavernous sinus and petroclival region, whereas the surgical mortality after the radical resection became the issue of discussion for QOL. In the 1990s, stereotactic radiosurgery provided a resolution of this problem and multimodal treatment is now commonly applied in order to achieve a satisfactory functional outcome and control the tumor. However, I am concerned that the role of stereotactic radiosurgery has been overestimated and the role of radical resection has a tendency of underestimation. As the radiation technology is advanced, the surgical techniques also could be advanced for the cure of this disease. We need the long-term follow-up results over 10 or 20 years in order to obtain the truth of the treatment philosophy. Our recent analysis of this particular tumor in the long-term follow-up periods showed that radical resection could provide a satisfactory outcome with 91.5% recurrence-free survival rate at 20 years [1]. As a result, I advocate that radical resection has the most important role even in the era of multimodal treatment. Additionally, I completely agree with the authors’ comment that the most important factors are the experience, philosophy, and techniques of the surgeon.
References
1. Ichinose T, Goto T, Ishibashi K, Takami T, Ohata K (2010) The role of radical microsurgical resection in multimodal treatment for skull base meningioma. J Neurosurg 113:1072–1078
Madjid Samii, Venelin Miroslav Gerganov, Hannover, Germany
The authors present a comprehensive review of the current management of skull base meningiomas with a special emphasize on the role of surgery. The significance of extent of resection, of tumor grade, and of various proliferative markers as predictors of the outcome and of the risk of recurrence is presented in detail. The surgical outcome in regards to tumor location is discussed, summarizing the results published by recognized expert groups in the last 10 years.
Some areas of future research are suggested in the manuscript. The current grading system of meningiomas is based on histopathological criteria, which do not account for the many individual tumor differences that are of paramount importance for the outcome. We believe that meningiomas, regardless of their histopathological grade, are two types: encapsulated or infiltrating. Encapsulated meningiomas can be removed completely without or with minimal morbidity. Infiltrating meningiomas, which frequently but not always, are microcystic, atypical, or anaplastic, tend to infiltrate the pial covering and even the neural tissue. In such cases, the attempt to remove the tumor completely may have dramatic consequences. The infiltration of the pia is not restricted to the aforementioned tumor categories and does not necessarily indicate malignant tumor: it may occur also in WHO grade I meningiomas. The possibility to predict these relationships of the meningioma to surrounding structures reliably before surgery would be of great value for the selection of appropriate management in each individual patient. In the future, meningioma grading will be certainly refined by inclusion of molecular and genetic criteria.
The goal of surgery in skull base meningiomas, according to the authors, is to “achieve as extensive resection as possible while minimizing neurological morbidity”—a statement that should be generally accepted. Radiosurgery has a certain place in the management of patients with meningiomas that are not amenable to complete removal due to the aforementioned tumor characteristics, due to tumor critical location (e.g., cavernous sinus), or in case the patient’s general condition precludes open surgery.
Chien-Min Chen and Abel Po-Hao Huang contributed equally to this study.
Rights and permissions
About this article
Cite this article
Chen, CM., Huang, A.PH., Kuo, LT. et al. Contemporary surgical outcome for skull base meningiomas. Neurosurg Rev 34, 281–296 (2011). https://doi.org/10.1007/s10143-011-0321-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-011-0321-x