Abstract
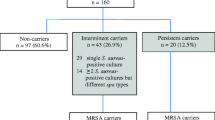
This study assessed the antimicrobial resistance and population structure of Staphylococcus aureus isolated from general practice (GP) patients and nursing home (NH) residents in the province of Limburg (near the border with Germany and Belgium) in comparison with those obtained in the remaining provinces of the Netherlands. A total of 617 and 418 S. aureus isolates were isolated from 2,691 to 1,351 nasal swabs from GP patients and NH residents, respectively. Quantitative antibiotic susceptibility testing was performed using a microbroth dilution method. Putative methicillin-resistant S. aureus (MRSA) isolates were tested for the presence of the mecA gene and spa typing was performed on all S. aureus isolates. No significant differences in the prevalence of resistance were found between the two groups of GP isolates, but the isolates from the NH residents showed a lower resistance for trimethoprim–sulfamethoxazole (p = 0.003) in Limburg province compared with the remaining provinces in the Netherlands. Among the isolates from NH residents in Limburg province, the prevalence of spa-CC 084 was higher (p = 0.003) and that of spa-CC 002 was lower (p = 0.01) compared with isolates from NHs in the remaining provinces of the Netherlands. We observed no differences in resistance and population structure between S. aureus isolates from GP patients in Limburg and the remaining provinces of the Netherlands, and only a few differences were observed between the NH populations. There was no higher prevalence of resistance among the GP and NH isolates from Limburg compared with the remaining provinces.
Similar content being viewed by others
References
Lowy FD (1998) Staphylococcus aureus infections. N Engl J Med 339(8):520–532
European Centre for Disease Prevention and Control (ECDC) (2011) Antimicrobial resistance surveillance in Europe 2010. Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net)
Dutch Working Party on Antibiotic Policy (SWAB) Nethmap 2011. Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands
AT5. MRSA-uitbraak in verpleeghuis Bernardus. Available online at: http://www.at5.nl/artikelen/57488/mrsa-uitbraak-in-verpleeghuis-bernardus. Accessed 20 June 2012
Nursing voor verpleegkundigen. MRSA-uitbraak in verpleeghuis Delfzijl. Available online at: http://www.nursing.nl/home/nieuw/2853/mrsa-uitbraak-in-verpleeghuis-delfzijl. Accessed 20 June 2012
BN De Stem. MRSA-bacterie in Janshove. Available online at: http://www.bndestem.nl/regio/breda/7969474/MRSAbacterie-in-Janshove.ece. Accessed 20 June 2012
Omroep Flevoland. MRSA-uitbraak Laarstaete gestopt. Available online at: http://www.omroepflevoland.nl/Nieuws/31528/mrsa-uitbraak-laarstaete-gestopt. Accessed 20 June 2012
Provincie Limburg. Feiten en cijfers. Available online at: http://www.limburg.nl/Over_Limburg/Feiten_en_cijfers. Accessed 20 June 2012
Commission of the European Communities (2008) Proposal for a directive of the European parliament and the council on the application of patients’ rights in cross-border healthcare. Brussels, 2.7.2008. COM(2008) 414 final
Vaessens RCM (2011) Limburgse pendel 2010: pendelstromen op provinciaal en gemeentelijk niveau. ETIL, Maastricht
Stadt Aachen. Euregion Maas-Rijn. Available online at: http://www.aachen.de/nl/sb/euregio/index.html. Accessed 20 June 2012
Donker GA, Deurenberg RH, Driessen C, Sebastian S, Nys S, Stobberingh EE (2009) The population structure of Staphylococcus aureus among general practice patients from The Netherlands. Clin Microbiol Infect 15(2):137–143
European Committee on Antimicrobial Susceptibility Testing (EUCAST) (2011) Breakpoint tables for interpretation of MICs and zone diameters. Version 1.3, January 2011
Fuchs PC, Jones RN, Barry AL (1990) Interpretive criteria for disk diffusion susceptibility testing of mupirocin, a topical antibiotic. J Clin Microbiol 28(3):608–609
Diagnostica R. EUCAST-and CLSI potency NEO-SENSITABS™. Interpretation zones and MIC breakpoints according to CLSI. Staphylococci. Document 3.3.0
Frénay HM, Bunschoten AE, Schouls LM, van Leeuwen WJ, Vandenbroucke-Grauls CM, Verhoef J, Mooi FR (1996) Molecular typing of methicillin-resistant Staphylococcus aureus on the basis of protein A gene polymorphism. Eur J Clin Microbiol Infect Dis 15(1):60–64
Schouls LM, Spalburg EC, van Luit M, Huijsdens XW, Pluister GN, van Santen-Verheuvel MG, van der Heide HG, Grundmann H, Heck ME, de Neeling AJ (2009) Multiple-locus variable number tandem repeat analysis of Staphylococcus aureus: comparison with pulsed-field gel electrophoresis and spa-typing. PLoS One 4(4):e5082
Narum SR (2006) Beyond Bonferroni: less conservative analyses for conservation genetics. Conserv Genet 7:783–787
Grundmann H, Hori S, Tanner G (2001) Determining confidence intervals when measuring genetic diversity and the discriminatory abilities of typing methods for microorganisms. J Clin Microbiol 39(11):4190–4192
den Heijer CDJ et al (2012) Prevalence and susceptibility of commensal S. aureus in nine European countries. In: Proceedings of the World Organization of Family Doctors Europe Conference 2012 (WONCA 2012), Vienna, Austria, July 2012
Wertheim HF, Vos MC, Ott A, van Belkum A, Voss A, Kluytmans JA, van Keulen PH, Vandenbroucke-Grauls CM, Meester MH, Verbrugh HA (2004) Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non-carriers. Lancet 364(9435):703–705
Daeschlein G, Assadian O, Rangous I, Kramer A (2006) Risk factors for Staphylococcus aureus nasal carriage in residents of three nursing homes in Germany. J Hosp Infect 63(2):216–220
Lasseter G, Charlett A, Lewis D, Donald I, Howell-Jones R, McNulty CA (2010) Staphylococcus aureus carriage in care homes: identification of risk factors, including the role of dementia. Epidemiol Infect 138(5):686–696
Karabay O, Otkun MT, Yavuz MT, Otkun M (2006) Nasal carriage of methicillin-resistant and methicillin-susceptible Staphylococcus aureus in nursing home residents in Bolu, Turkey. W Indian Med J 55(3):183–187
van der Donk CFM, Schols JMGA, Driessen CJ, Hagenouw RGP, Meulendijks A, Stobberingh EE (2012) Prevalence and spread of multidrug resistant Escherichia coli isolates among nursing home residents in the southern part of the Netherlands. J Am Med Dir Assoc (in press)
Dutch Working Party on Antibiotic Policy (SWAB) Nethmap 2009. Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands
Goossens H, Ferech M, Vander Stichele R, Elseviers M; ESAC Project Group (2005) Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 365(9459):579–587
Vellinga A, Tansey S, Hanahoe B, Bennett K, Murphy AW, Cormican M (2012) Trimethoprim and ciprofloxacin resistance and prescribing in urinary tract infection associated with Escherichia coli: a multilevel model. J Antimicrob Chemother 67(10):2523–2530
Balslev U, Bremmelgaard A, Svejgaard E, Havstreym J, Westh H (2005) An outbreak of borderline oxacillin-resistant Staphylococcus aureus (BORSA) in a dermatological unit. Microb Drug Resist 11(1):78–81
Skinner S, Murray M, Walus T, Karlowsky JA (2009) Failure of cloxacillin in treatment of a patient with borderline oxacillin-resistant Staphylococcus aureus endocarditis. J Clin Microbiol 47(3):859–861
Nadarajah J, Lee MJ, Louie L, Jacob L, Simor AE, Louie M, McGavin MJ (2006) Identification of different clonal complexes and diverse amino acid substitutions in penicillin-binding protein 2 (PBP2) associated with borderline oxacillin resistance in Canadian Staphylococcus aureus isolates. J Med Microbiol 55(Pt 12):1675–1683
Mellmann A, Weniger T, Berssenbrügge C, Keckevoet U, Friedrich AW, Harmsen D, Grundmann H (2008) Characterization of clonal relatedness among the natural population of Staphylococcus aureus strains by using spa sequence typing and the BURP (based upon repeat patterns) algorithm. J Clin Microbiol 46(8):2805–2808
Grundmann H, Aanensen DM, van den Wijngaard CC, Spratt BG, Harmsen D, Friedrich AW; European Staphylococcal Reference Laboratory Working Group (2010) Geographic distribution of Staphylococcus aureus causing invasive infections in Europe: a molecular-epidemiological analysis. PLoS Med 7(1):e1000215
Acknowledgments
The authors would like to thank the participants for their help, and the general practitioners and the nursing home staff for their assistance with the collection of the samples.
Funding
This project was financially supported, in part, by the Dutch Working Party on Antibiotic Policy (SWAB) and, in part, by Provincie Limburg, the Netherlands; Ministerium für Wirtschaft, Energie, Bauen, Wohnen und Verkehr des Landes Nordrhein-Westfalen, Germany; Ministerium der Deutschsprachigen Gemeinschaft Belgiens, Belgium; Provincie Limburg, Belgium; Wallonie, Belgium; Rheinland-Westfalen, Germany; Interreg and the Euregio Maas-Rijn with support of the European Fund for Regional Development (EFRO).
The funding institutions were not involved in any part of this study.
Competing interests
None to declare.
Ethical approval
Ethical approval for this project was granted by the Medical Ethics Committee of the Maastricht University Medical Centre, reference number: 07-4-012.4/pl.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van der Donk, C.F.M., Rijnders, M.I.A., Donker, G.A. et al. Is living in a border region a risk for a high prevalence of resistance?. Eur J Clin Microbiol Infect Dis 32, 989–995 (2013). https://doi.org/10.1007/s10096-013-1835-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-013-1835-7