Abstract
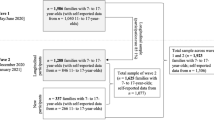
Children of parents with mental health problems (CPM) have an increased risk for behavioral and psychological problems. This study investigated the age- and gender-specific course as well as predictors of mental health problems in CPM using the longitudinal data (baseline 1- and 2-year follow-ups) of a German general population sample from the BELLA study. Children and adolescents aged 11–17 years (at baseline) who had a parent with mental health problems (n = 325) were analyzed. The mental health problems of the children were assessed by the self-reported version of the strengths and difficulties questionnaire (SDQ). We used individual growth modeling to investigate the age- and gender-specific course, and the effects of risk as well as personal, familial and social protective factors on self-reported mental health problems in CPM. Additionally, data were examined differentiating internalizing and externalizing mental health problems in CPM. Results indicated that female compared to male CPM showed increasing mental health problems with increasing age. Mental health problems in CPM were associated with lower self-efficacy, worse family climate and less social competence over time. Internalizing problems were associated with lower self-efficacy, less social competence and more severe parental mental health problems. Externalizing problems were associated with lower self-efficacy, worse family climate and lower social competence. The main limitations of the study are the short time period (2 years) covered and the report of mental health problems by only one parent. Our findings should be considered in the development of treatment and prevention programs for mental health problems in CPM.



Similar content being viewed by others
References
Beardslee WR, Gladstone TRG, O’Connor EE (2011) Transmission and prevention of mood disorders among children of affectively ill parents: a review. J Am Acad Child Adolesc Psychiatry 50(11):1098–1109. https://doi.org/10.1016/j.jaac.2011.07.020
Mattejat F, Remschmidt H (2008) The children of mentally Ill parents. Deutsch Arzteblatt Int 105(23):413–418. https://doi.org/10.3238/arztebl.2008.413
Siegenthaler E, Munder T, Egger M (2012) Effect of preventive interventions in mentally ill parents on the mental health of the offspring: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 51(1):8–17. https://doi.org/10.1016/j.jaac.2011.10.018
McLaughlin KA, Gadermann AM, Hwang I, Sampson NA, Al-Hamzawi A, Andrade LH, Angermeyer MC, Benjet C, Bromet EJ, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, de Graaf R, Florescu S, Gureje O, Haro JM, Hinkov HR, Horiguchi I, Hu CY, Karam AN, Kovess-Masfety V, Lee S, Murphy SD, Nizamie SH, Posada-Villa J, Williams DR, Kessler RC (2012) Parent psychopathology and offspring mental disorders: results from the WHO World Mental Health Surveys. Br J Psychiatry 200(4):290–299. https://doi.org/10.1192/bjp.bp.111.101253
Plass-Christl A, Haller AC, Otto C, Barkmann C, Wiegand-Grefe S, Holling H, Schulte-Markwort M, Ravens-Sieberer U, Klasen F (2017) Parents with mental health problems and their children in a German population based sample: results of the BELLA study. PLoS One 12(7):e0180410. https://doi.org/10.1371/journal.pone.0180410
Lewandowski RE, Verdeli H, Wickramaratne P, Warner V, Mancini A, Weissman M (2014) Predictors of positive outcomes in offspring of depressed parents and non-depressed parents across 20 years. J Child Fam Stud 23(5):800–811. https://doi.org/10.1007/s10826-013-9732-3
Pargas RCM, Brennan PA, Hammen C, Le Brocque R (2010) Resilience to maternal depression in young adulthood. Dev Psychol 46(4):805–814. https://doi.org/10.1037/a0019817
Masten AS, Reed M-GJ (2002) Resilience in development. In: Snyder CR, Lopez SJ (eds) Handbook of positive psychology. Oxford University Press, Oxford, pp 74–88
Plass A, Haller AC, Habermann K, Barkmann C, Petermann F, Schipper M, Wiegand-Grefe S, Holling H, Ravens-Sieberer U, Klasen F (2016) Factors promoting mental health in children of parents with mental health problems: results of the BELLA Cohort study. Kindheit und Entwicklung 25(1):41–49. https://doi.org/10.1026/0942-5403/a000187
Garai EP, Forehand RL, Colletti CJM, Reeslund K, Potts J, Compas B (2009) The relation of maternal sensitivity to children’s internalizing and externalizing problems within the context of maternal depressive symptoms. Behav Modif 33(5):559–582. https://doi.org/10.1177/0145445509342581
Reuben JD, Shaw DS (2015) Resilience in the offspring of depressed mothers: variation across risk, domains, and time. Clin Child Fam Psychol Rev 18(4):300–327. https://doi.org/10.1007/s10567-015-0195-5
Kamtsiuris P, Lange M, Schaffrath Rosario A (2007) Der Kinder- und Jugendgesundheitssurvey (KiGGS): stichprobendesign, response und nonresponse-analyse (The German Health Interview and Examination Survey for Children and Adolescents (KiGGS): sample design, response and nonresponse analysis). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50(5–6):547–556. https://doi.org/10.1007/s00103-007-0215-9
Ravens-Sieberer U, Otto C, Kriston L, Rothenberger A, Dopfner M, Herpertz-Dahlmann B, Barkmann C, Schon G, Holling H, Schulte-Markwort M, Klasen F, Grp BS (2015) The longitudinal BELLA study: design, methods and first results on the course of mental health problems. Eur Child Adolesc Psychiatry 24(6):651–663. https://doi.org/10.1007/s00787-014-0638-4
Kurth BM, Kamtsiuris P, Holling H, Schlaud M, Dolle R, Ellert U, Kahl H, Knopf H, Lange M, Mensink G, Neuhauser H, Rosario A, Scheidt-Nave C, Schenk L, Schlack R, Stolzenberg H, Thamm M, Thierfelder W, Wolf U (2008) The challenge of comprehensively mapping children’s health in a nation-wide health survey: design of the German KiGGS-study. BMC Public Health 8(1):196
Klaghofer R, Brahler E (2001) Construction and statistical testing of a short version of the SCL-90-R. Zeitschrift für Klinische Psychologie Psychiatrie und Psychotherapie 49(2):115–124
Derogatis LR (ed) (1977) SCL-90-R administration, scoring and procedures—manual-I for the Revised version. John Hopkins University School of Medicine, Baltimore
Franke GH (2002) SCL-90-R: Symptom-Checkliste von L.R. Derogatis—deutsche Version. Beltz Test GmbH, Göttingen
Goodman R (1997) The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 38(5):581–586
Goodman A, Lamping DL, Ploubidis GB (2010) When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the Strengths and Difficulties Questionnaire (SDQ): data from British parents, teachers and children. J Abnorm Child Psychol 38(8):1179–1191
Schwarzer R, Jerusalem M (1995) Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M (eds) Measures in health psychology: a user’s portfolio. Causal and control beliefs NFER-NELSON, Windsor, pp 35–37
Schneewind K, Beckmann M, Hecht-Jackl A (1985) Familienklima-Skalen. Bericht 8.1 und 8.2. Ludwig Maximilians Universität, Institut für Psychologie-Persönlichkeitspsychologie und Psychodiagnostik, München
Currie C, Samdal O, Boyce W, Smith R (2001) Health behaviour in school-aged children: A WHO Cross-National Study (HBSC), Research Protocol for the 2001/2002 Survey. University of Edinburgh: Child and Adolescent Health Research Unit (CAHRU)
Winkler J, Stolzenberg H (1999) Der Sozialschichtindex im Bundes-Gesundheitssurvey. Gesundheitswesen 61:S178–S183
Lange M, Kamtsiuris P, Lange C, Schaffrath Rosario A, Stolzenberg H, Lampert T (2007) Messung soziodemographischer Merkmale im Kinder- und Jugendgesundheitssurvey (KiGGS) und ihre Bedeutung am Beispiel der Einschätzung des allgemeinen Gesundheitszustands. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50(5–6):578–589
DeLucia C, Pitts SC (2006) Applications of individual growth curve modeling for pediatric psychology research. J Pediatr Psychol 31(10):1002–1023. https://doi.org/10.1093/jpepsy/jsj074
Heck R, Thomas S, Tabata L (2014) Multilevel and longitudinal modeling with IBM SPSS. Routledge, New York
Field A (2015) Discovering statistics using IBM SPSS statistics, 4th edn. Sage Publications Ltd., London
McFadden D (1974) Conditional logit analysis of qualitative choice behaviour. In: Zarembka P (ed) Frontiers in Ecnometrics. Academic Press, New York, pp 105–142
Chang JJ, Halpern CT, Kaufman JS (2007) Maternal depressive symptoms, father’s involvement, and the trajectories of child problem Behaviors in a US national sample. Arch Pediatr Adolesc Med 161(7):697–703. https://doi.org/10.1001/archpedi.161.7.697
Meltzer H, Gatward R, Goodman R, Ford T (2000) Mental health of children and adolescents in Great Britain. Stationery Office, London
Mellor D (2005) Normative data for the Strengths and Difficulties Questionnaire in Australia. Aust Psychol 40(3):215–222. https://doi.org/10.1080/00050060500243475
Costello EJ, Copeland W, Angold A (2011) Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry 52(10):1015–1025. https://doi.org/10.1111/j.1469-7610.2011.02446.x
Turner SM, Beidel DC, Costello A (1987) Psychopathology in the offspring of anxiety disorder patients. J Consult Clin Psychol 55:229–235
Biedermann J, Petty C, Faraone SV, Henin A, Hirshfeld-Becker D, Pollack MH et al (2006) Effects of parental anxiety disorders in children at high risk for panic disorder: a controlled study. J Affect Disord 94:191–197
Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig MA, Fenton B, Zhang HP, O’Malley SS, Rounsaville BJ (1998) Familial transmission of substance use disorders. Arch Gen Psychiatry 55(11):973–979. https://doi.org/10.1001/archpsyc.55.11.973
Clark DB, Cornelius J, Wood DS, Vanyukov M (2004) Psychopathology risk transmission in children of parents with substance use disorders. Am J Psychiatry 161:685–691
Lieb R, Isensee B, Höfler M, Pfister H, Wittchen HU (2002) Parental major depression and the risk of depression and other mental disorders in offspring. A prospective-longitudinal community study. Arch Gen Psychiatry 59:365–374
Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D (2011) Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev 14(1):1–27. https://doi.org/10.1007/s10567-010-0080-1
Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE (2010) Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am J Psychiatry 167(5):509–527. https://doi.org/10.1176/appi.ajp.2010.09101452
Kendler KS, Prescott CA, Myers J, Neale MC (2003) The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry 60(9):929–937. https://doi.org/10.1001/archpsyc.60.9.929
Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ (2004) Family transmission and heritability of externalizing disorders—a twin-family study. Arch Gen Psychiatry 61(9):922–928. https://doi.org/10.1001/archpsyc.61.9.922
Luthar SS, Sexton CC (2007) Maternal drug abuse versus maternal depression: vulnerability and resilience among school-age and adolescent offspring. Dev Psychopathol 19(1):205–225. https://doi.org/10.1017/s0954579407070113
Wiegand-Grefe S, Geers P, Halverscheid S, Petermann F, Plass A (2010) Kinder psychisch kranker Eltern. Zusammenhänge zwischen der Krankheitsbewältigung einer elterlichen psychischen Erkrankung und der Gesundheit der Kinder. Zeitschrift für klinische Psychologie und Psychotherapie 39(1):13–23
Becker A, Hagenberg N, Roessner V, Woerner W, Rothenberger A (2004) Evaluation of the self-reported SDQ in a clinical setting: do self-reports tell us more than ratings by adult informants? Eur Child Adolesc Psychiatry 13:17–24. https://doi.org/10.1007/s00787-004-2004-4
Klasen F, Petermann F, Meyrose AK, Barkmann C, Otto C, Haller AC, Schlack R, Schulte-Markwort M, Ravens-Sieberer U (2016) Trajectories of mental health problems in children and adolescents: results of the BELLA Cohort Study. Kindheit und Entwicklung 25(1):10–20. https://doi.org/10.1026/0942-5403/a000184
Brent D, Brunwasser SM, Hollon SD, Weersing VR, Clarke GN, Dickerson JF, Beardslee WR, Gladstone T, Porta G, Lynch F, Iyengar S, Garber J (2015) Effect of a cognitive-behavioral prevention program on depression 6 years after implementation among at-risk adolescents: a randomized clinical trial. JAMA Psychiatry 72(11):1110–1118. https://doi.org/10.1001/jamapsychiatry.2015.1559
Wiegand-Grefe S, Alberts J, Petermann F, Plass A (2016) Differential perspectives on family functioning and interfamilial relationships: the effect of a manualized intervention program on children of mentally Ill parents. Kindheit und Entwicklung 25(2):77–88. https://doi.org/10.1026/0942-5403/a000192
Acknowledgements
The authors thank all participants of the BELLA study and their parents for their time and involvement. We also would like to thank the Robert-Koch Institute for their ongoing support and co-operation. The baseline, 1- and 2-year follow-up assessments of the BELLA study were financed by the German Science Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Plass-Christl, A., Otto, C., Klasen, F. et al. Trajectories of mental health problems in children of parents with mental health problems: results of the BELLA study. Eur Child Adolesc Psychiatry 27, 867–876 (2018). https://doi.org/10.1007/s00787-017-1084-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-017-1084-x