Abstract
Although ADHD significantly affects the quality of life (QoL) of patients and their families, QoL in children with ADHD has rarely been investigated in association with psychopathological profile, and the relationship remains unclear. The open-label OBSEER study evaluated the effectiveness and tolerability of Equasym XL®, a modified-release methylphenidate, in routine care of children and adolescents (aged 6–17 years) with ADHD. At baseline, questionnaires assessing psychopathological profile (Strengths and Difficulties Questionnaire, SDQ; parental ratings) and QoL (KINDL; parent, child or adolescent versions) were completed; QoL was reassessed at final visit. We analysed the relationship between psychopathology and parent/patient-rated QoL in ADHD at baseline. Data from 721 consecutively referred children and adolescents were analysed. QoL was similarly low from parent and self-ratings and independent of severity on the SDQ subscale hyperactivity/inattention. Self-ratings indicated that additional conduct disorder was associated with further reduction in QoL. Similarly, children with high scores from parent and adolescent ratings on the SDQ subscale conduct problems had reduced QoL on some KINDL subscales. Adolescents with ADHD not receiving medication at baseline reported lower QoL than those already on medication. Results show that children and adolescents with ADHD have low QoL, independent of core symptom severity. Additional conduct problems may further impact QoL negatively, while ADHD medication use may show a trend towards improved QoL. Not all psychopathological problems associated with ADHD affect QoL similarly. As parents appear to have a less critical view of QoL compared with children’s self-ratings, both parent and child ratings should be included in clinical assessments.
Similar content being viewed by others
Introduction
Over the past few years, clinical work and research on quality of life (QoL) has become increasingly important in improving both physical and mental health in children. In the field of attention deficit hyperactivity disorder (ADHD), several studies on QoL have been published and were included in a systematic review [7]. This level of interest is not surprising due to the complexity of the relationships; QoL is not only influenced by the disorder itself, but also by many proximal (i.e. family, friendship) and distal (socioeconomic and cultural) factors. In addition to its core symptoms of attention deficit, hyperactivity and impulsivity, ADHD is associated with numerous developmental, cognitive, emotional, social and academic impairments [12, 17, 25]. One possible reason for this might be that in ADHD, more than 80% of children and adults are likely to have at least one other psychiatric disorder and more than 50% are likely to have two [10, 23]. Thus, in ADHD, psychiatric comorbidity is the rule rather than the exception [24]. These comorbidities, as well as the other proximal and distal factors, affect the QoL of both patients and their families [7].
There is significant potential for overlap between the instruments designed to measure QoL and those used to measure psychopathology or functional impairment. Clear distinctions between symptoms (e.g. low mood or poor concentration) and their potential effects (i.e. functional impairment and/or reduced QoL), and also between functional impairment on the one hand and QoL on the other, are desirable [7]. Otherwise, there is a clear risk that apparent QoL effects are so closely related to symptoms and functional impairment that their association with the disorder will become a tautology [7]. In this context, it becomes evident that examining not only the relationship between QoL and categorical psychopathology (i.e. an ADHD diagnosis), but also the relationship with dimensional psychopathology (i.e. functional impairment and symptom scores), would result in improved understanding of the complex interplay of one or more disorders as well as of proximal and distal factors.
For an outcome as subjective as QoL, the influence of the rater’s role should also be highlighted. A parent’s rating of their child’s QoL gives only one perspective of the overall impact of the illness on QoL. This may limit the validity of studies that do not ask children for their view on their own QoL. Such a difference is reflected, for example, by the only modest levels of agreement between the child’s and other informants’ ratings of QoL [13, 15], particularly with regard to non-observable aspects (such as emotional or social functioning). Parent ratings may, however, provide an important alternative perspective. Therefore, in studies on ADHD, measures of QoL as well as measures of psychopathology should include both a child- and a parent-rated version.
The aim of this analysis was to have a detailed look at the relationships between dimensional psychopathology and both parent- and child-rated QoL in ADHD. This analysis also evaluated the validity of the QoL concept, as described by Coghill et al. [5]. By studying correlative considerations, the relationship between QoL and psychopathological problems may be better understood. The effects of medication on QoL in ADHD are reported in a companion paper [8].
Methods
Study design
The open-label, prospective, multicentre, observational, post-marketing OBSEER (OBservation of Safety and Effectiveness of Equasym XL® in Routine care) study was designed primarily to assess the effectiveness and safety of Equasym XL® Footnote 1 (Shire Pharmaceuticals Ireland Limited, Ireland) in children and adolescents with ADHD and is described in full elsewhere [8]. Here, pre-specified outcomes of QoL and the dimensional psychopathological profile (SDQ) are examined and related to each other cross-sectionally at the baseline visit in post hoc analyses.
Patients and treatment
Patients with ADHD (diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision [DSM]-IV-TR [1] or the International Classification of Diseases [ICD]-10 criteria [26]) aged 6–17 years and attending school were included if treatment with Equasym XL® was planned by the treating physician. Patients either could have received prior medication or were medication naive. The study was conducted in accordance with local regulations and under the therapeutic responsibility of the attending physicians; ethics or institutional review board approval was not required for this study. Written informed consent was obtained from parents.
Assessments
QoL
QoL was assessed using the Kinder Lebensqualitätsfragebogen (KINDL) questionnaire for the assessment of health-related QoL in childhood and adolescence [18]. This is a validated tool comprising 24 items, with six subscores (physical well-being, emotional well-being, self-esteem, family, friends and school). Three versions were used according to age group: KID-KINDL was used for children aged 6–11 years; the self-reported KIDDO-KINDL for adolescents aged 12–17 years; and KINDL for parents of patients aged 6–17 years. Scores were transformed so that the range of possible values for the subscores and the total score was from 0 (most negative state) to 100 (most positive state).
SDQ
Parents were asked to complete a version of the Strengths and Difficulties Questionnaire (SDQ) that supplements the 25 core items on specific strengths and difficulties with an overall rating of whether their child has emotional or behavioural problems [11, 22]. Each of the 25 items is rated as being not true (0), somewhat true (1) or certainly true (2); each of the five subscales consists of five items, thus yielding scores between 0 and 10 for each subscale. Although the wording chosen for 10 of the 25 SDQ questions addresses positive behavioural attributes, five of these 10 item scores were inverted before being summed up. Thus, four of the SDQ subscales represent problem scores (emotional symptoms, conduct problems, hyperactivity/inattention and peer problems), which were added together to obtain a total difficulties score ranging from 0 to 40. The fifth subscale assesses the positive aspect of prosocial behaviour. Scores for each subscale were considered to be normal, borderline or abnormal. Total difficulties scores were considered to be normal (range 0–12), borderline (range 13–15) or abnormal (range 16–40).
Statistical analyses
The following outcomes were assessed: parent-rated dimensional psychopathological severity according to the SDQ and parent- and self-rated QoL at baseline.
Results presented are for the intent-to-treat population. Analysis of variance (ANOVA) modelling was performed to determine the effects of parent-rated SDQ subscale scores and total difficulties score on QoL. In subgroup analyses, patients were assigned to groups according to their diagnosis (ADHD only versus ADHD with conduct disorder) and treatment prior to starting Equasym XL® (no treatment; or treatment with modified-release methylphenidate [MPH], immediate-release MPH [MPH-IR] administered once daily, MPH-IR administered several times per day or ‘other’, for which treatment was unspecified [atomoxetine, amphetamine or insufficiently specified]). Finally, correlation coefficients between the parent-reported SDQ subscales and total difficulties score and the parent- and self-rated QoL scales in the study (KINDL, KID-KINDL and KIDDO-KINDL) were calculated.
Scale means for parent ratings of both the SDQ and the KINDL scales were compared with those from the BELLA study, which assessed the prevalence of general and specific mental health problems in a representative sample of children and adolescents in Germany [19, 21].
Results
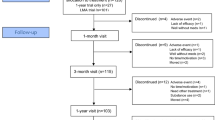
Study population
In total, 852 patients were enrolled in the study. Thirty patients were excluded from the analysis due to invalid data; a further 101 patients were excluded because their SDQ data were missing or incomplete. Therefore, 721 patients were included in the analysis population. Baseline demographics are described elsewhere [8].
Relationship between SDQ scores in the normal range and QoL
Self-ratings of QoL from children aged 6–11 years showed that those with normal (range 0–5) scores on the hyperactivity/inattention subscale of the SDQ tended to achieve higher, albeit not significantly, scores on the KID-KINDL friends subscale than if they had borderline (6) or abnormal (range 7–10) SDQ scores (mean [SD] 68.4 [19.8] vs. 61.3 [20.7] and 65.5 [22.7]; F (2, 474) = 2.445; 0.05 < P ≤ 0.1).
Children with normal (range 0–12) or borderline (range 13–15) SDQ total difficulties scores had higher scores, indicating better QoL, on the KINDL friends subscale than children with abnormal (range 16–40) SDQ scores (mean [SD] 63.2 [19.4] and 63.4 [20.8] vs. 58.7 [21.2]; F (2, 718) = 3.817; P ≤ 0.05). Compared with children with borderline or abnormal SDQ total difficulties scores, those with normal scores tended to rate themselves as more content on the KID-KINDL school subscale (mean [SD] 61.8 [21.3] vs. 53.6 [23.0] and 58.2 [22.5]; F (2, 474) = 2.589; 0.05 < P ≤ 0.1).
Adolescents with normal SDQ total difficulties scores tended to show the highest QoL on the KIDDO-KINDL family subscale compared with those with borderline or abnormal scores (mean [SD] 73.5 [20.9] vs. 59.3 [23.6] and 66.6 [22.9]; F (2, 164) = 2.545; 0.05 < P ≤ 0.1).
Correlation between severity of SDQ scores and QoL
Correlation analyses showed that children with high SDQ total difficulties scores had significantly lower QoL on the parent-rated KINDL total score (r = −0.091; P ≤ 0.05) and on the subscales emotional well-being (r = −0.106; P ≤ 0.01) and friends (r = −0.131; P ≤ 0.01; Table 1). There was also a similar trend for the subscale self-esteem (r = −0.063; 0.05 < P ≤ 0.1).
Children with high scores on the SDQ emotional problems subscale had significantly lower values on the parent-rated KINDL total score (r = –0.097; P ≤ 0.01) and on the subscales emotional well-being (r = −0.096; P ≤ 0.05) and friends (r = −0.118; P ≤ 0.01). A similar trend was found for the subscale school (r = −0.073; 0.05 < P ≤ 0.1).
For the SDQ subscale conduct problems, children with higher scores tended to have lower QoL based on the parent-rated KINDL scale emotional well-being (r = −0.069; 0.05 < P ≤ 0.1), although this was not significant.
There were no significant correlations between the SDQ subscale hyperactivity/inattention and any of the parent-rated KINDL subscales.
Children scoring high on the SDQ subscale peer problems had significantly lower QoL on the KINDL subscales emotional well-being (r = −0.084; P ≤ 0.05) and friends (r = −0.134; P ≤ 0.01). A similar trend was observed for the KINDL total score (r = −0.067; 0.05 < P ≤ 0.1).
There were no significant correlations between psychopathology and QoL self-ratings from children aged 6–11 years (KID-KINDL; data not shown).
Adolescents who had high SDQ total difficulties scores had a significantly lower QoL on the KIDDO-KINDL subscales self-esteem (r = −0.170; P ≤ 0.05) and friends (r = −0.190; P ≤ 0.05), with a trend for lower QoL on the family subscale (r = −0.128; 0.05 < P ≤ 0.1; Table 2). Children with high scores on the SDQ subscale emotional problems tended to have lower scores on the KIDDO-KINDL subscales self-esteem (r = −0.143; 0.05 < P ≤ 0.1) and friends (r = −0.137; 0.05 < P ≤ 0.1).
Adolescents with high scores on the SDQ subscale hyperactivity showed a significantly lower QoL on the KIDDO-KINDL total score (r = −0.174; P ≤ 0.05), family (r = −0.155; P ≤ 0.05) and friends (r = −0.202; P ≤ 0.01; Table 2). Furthermore, a similar trend was found for the KINDL subscale school (r = −0.132; 0.05 < P ≤ 0.1). Adolescents with high scores on the SDQ subscale peer problems tended to have a lower QoL on the KIDDO-KINDL subscale self-esteem (r = −0.153; P ≤ 0.05). There were no significant correlations between the SDQ subscales conduct problems or prosocial behaviour and any of the KIDDO-KINDL subscales.
Compared with the recent normative reference values for children and adolescents in Germany obtained in the epidemiological BELLA study [19, 21], children and adolescents with ADHD, as seen in the OBSEER study, were significantly more severely affected on every SDQ subscale and had a significantly lower QoL on every KINDL subscale (Table 3).
Comorbid conduct disorder and QoL
One-way ANOVA was used to test whether there were differences between scores on each scale associated with having an additional conduct disorder (Table 4). Of note, SDQ scores, including those for the subscale conduct problems, did not differ between diagnostic groups. Similarly, there were no differences in QoL between children with or without additional conduct disorder from KINDL parent ratings.
In contrast, self-ratings from children aged 6–11 years (KID-KINDL) showed that those with an additional conduct disorder had lower QoL than those without (Table 4). This applied to the total score (F (1, 427) = 6.246; P ≤ 0.05) and the subscales self-esteem (F (1, 432) = 6.264; P ≤ 0.05), family (F (1, 430) = 11.683; P ≤ 0.001) and friends (F (1, 431) = 4.230; P ≤ 0.05). A similar trend was found for the subscale school (F (1, 430) = 3.015; 0.05 < P ≤ 0.1), although this was not significant.
Adolescents aged 12–17 years (KIDDO-KINDL) showed a similar pattern to children for the QoL evaluation. The most impaired were the adolescents with an additional conduct disorder, with an effect on the total score (F (1, 135) = 11.715; P ≤ 0.001) and the scales physical well-being (F (1, 137) = 5.011; P ≤ 0.05), emotional well-being (F (1, 137) = 6.366; P ≤ 0.05), self-esteem (F (1, 137) = 4.639; P ≤ 0.05), family (F (1, 136) = 10.291; P ≤ 0.01) and friends (F (1, 137) = 4.660; P ≤ 0.05).
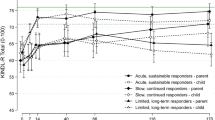
Medication subgroups and QoL
When subgroups of patients were compared according to whether they had received prior medication or not, no statistically significant differences were found either for the KINDL or for the KID-KINDL (Table 5). For the KIDDO-KINDL, adolescents receiving any prior medication scored significantly higher on the KIDDO-KINDL subscale school (F (1, 166) = 2.448; P ≤ 0.05) than those who had not received prior medication. A similar trend was found for the subscales self-esteem (F (1, 166) = 2.376; 0.05 < P ≤ 0.1) and family (F (1, 166) = 1.997; 0.05 < P ≤ 0.1). There were no significant differences in SDQ scores according to whether or not the patient had received prior medication.
Discussion
ADHD is associated with a variety of behavioural problems; therefore, knowledge of the complete psychopathological profile is important for treatment decisions and follow-up. Danckaerts et al. [7] showed that a robust negative effect on QoL was reported by the parents of children with ADHD across a broad range of psychopathology symptoms. Additional comorbid disorders, such as oppositional defiant disorder [16], and increased symptom levels also seem to predict reduced QoL [14]. For this reason, it is useful to know what influence psychopathological profile has on QoL. We investigated the relationship between these two parameters in this analysis of the observational OBSEER trial. An advantage of this study is that self-assessment of children was included and thus findings are not limited to just the views of parents or caregivers, unlike the majority of QoL studies [7].
Our results show that classifying scores on the SDQ subscale hyperactivity/inattention and the SDQ total problem score as normal, borderline or abnormal did not sufficiently differentiate between children’s QoL as rated by their parents. This may be due to the fact that, in this fairly homogeneous clinical sample, most children with ADHD had low QoL. Indeed, this was reflected in both parent and self-ratings. Thus, it is probable that an apparent ‘bottom effect’ did not allow QoL to be adequately differentiated using severity-categorized SDQ values in this sample.
Although ADHD symptom severity appeared to have little influence on QoL, having a comorbid conduct disorder had a substantial impact. However, this was evident only on self-ratings; ratings from parents did not differ between QoL of children with ADHD only and those with ADHD plus a conduct disorder. The findings indicate that adolescents, in particular, experience a significant decrease in QoL if they have a comorbid conduct disorder. Therapists should consider this aspect when planning multimodal treatment and adjust the sequence of interventions according to the subjective view of impairment given by the patient.
Parent and child ratings did not identify any significant differences in QoL due to prior medication. However, adolescents not taking medication at baseline had significantly lower QoL on the KIDDO-KINDL subscale school compared with adolescents taking any MPH medication. A similar trend was found for the subscales self-esteem and family, but the majority of scales showed no differences. Hence, the positive effect of medication on QoL seen in some previous trials [4, 9] was observed only as an overall trend in this study.
Scores for the SDQ subscales and total difficulties had varying associations with the QoL assessment scales used in the OBSEER study. For parental ratings, the highest correlation (negative) was seen between the SDQ subscale peer problems and the KINDL subscale friends. Thus, children with lower QoL according to the subscale friends had significantly more problems with their peers. It is likely that these scales measure similar, but opposing, aspects of behaviour. Furthermore, it was found that a high psychopathological value on the SDQ subscales peer problems, emotional problems and total problems is accompanied by lower QoL on the KINDL subscales emotional well-being, friends and total score. However, these significant relationships are based on low correlation coefficients and thus need to be interpreted with caution. In addition, adolescents with high scores on the SDQ scale hyperactivity had a significantly lower QoL (KIDDO-KINDL). This association was most notable for the total score and the subscales family and friends.
The results of this study are consistent with the results of another observational trial, the ADORE study [2], which recruited a comparable sample (with regard to sample size and demographic characteristics) of children with ADHD across Europe. In that study, baseline SDQ values were similar to those in the current study, and the QoL of children with ADHD in the ADORE study was markedly lower at baseline [20] than the norms for children in the community [3].
However, according to SDQ scales, a relatively high proportion of children and adolescents in the OBSEER study were classified as having impaired psychopathology. A total of 67.1% of children were classified as ‘abnormal’ on the SDQ total score and 57.1% on the SDQ subscale hyperactivity/inattention, compared with 6–9% of children in the normative BELLA study [21].
A limitation of our analysis is that the clinical diagnoses were not based on structured interviews, which may limit the reliability of the findings. Furthermore, for the ANOVA, the multiple testing of correlations was not adjusted and therefore should be regarded as exploratory. Finally, the prior medication status of patients was not identified at randomization, which makes it difficult to interpret the presence or absence of meaningful differences.
In addition to providing further evidence that QoL is low in children with ADHD, our results show that different psychopathological problems influence QoL in different ways. According to child and adolescent self-ratings, having a comorbid conduct disorder was associated with significantly lower QoL. Based on our results, it is recommended that when assessing QoL, children’s ratings should be used in conjunction with parental ratings for a complete picture.
Notes
Equasym XL is the UK trade name, and is registered and marketed by Shire in the following countries under the following trademarks: Denmark, Equasym Depot; Finland, Equasym Retard; France, Quasym LP; Germany, Equasym Retard; Ireland, Equasym XL; Netherlands, Equasym XL; Norway, Equasym Depot; Sweden, Equasym Depot; South Korea, Metadate CD; Mexico, Metadate CD. Information correct at August 2011.
References
American Psychiatric Association (2000) Attention-deficit and disruptive behaviour disorders. Attention-deficit/hyperactivity disorder. Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Arlington, pp 85–103
Becker A, Steinhausen HC, Baldursson G, Dalsgaard S, Lorenzo MJ, Ralston SJ, Dopfner M, Rothenberger A (2006) Psychopathological screening of children with ADHD: strengths and difficulties questionnaire in a pan-European study. Eur Child Adolesc Psychiatry 15(Suppl 1):I56–I62
Bullinger M, Brutt AL, Erhart M, Ravens-Sieberer U (2008) Psychometric properties of the KINDL-R questionnaire: results of the BELLA study. Eur Child Adolesc Psychiatry 17(Suppl 1):125–132
Cannon M, Pelham WH, Sallee FR, Palumbo DR, Bukstein O, Daviss WB (2009) Effects of clonidine and methylphenidate on family quality of life in attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 19:511–517
Coghill D, Danckaerts M, Sonuga-Barke E, Sergeant J (2009) Practitioner review: quality of life in child mental health—conceptual challenges and practical choices. J Child Psychol Psychiatry 50:544–561
Cohen J (1988) Statistical power analysis for the behavioural sciences. Lawrence Erlbaum Associates, Hillsdale
Danckaerts M, Sonuga-Barke EJ, Banaschewski T, Buitelaar J, Dopfner M, Hollis C, Santosh P, Rothenberger A, Sergeant J, Steinhausen HC, Taylor E, Zuddas A, Coghill D (2010) The quality of life of children with attention deficit/hyperactivity disorder: a systematic review. Eur Child Adolesc Psychiatry 19:83–105
Döpfner M, Görtz-Dorten A, Breuer D, Rothenberger A (2011) An observational study of once-daily modified-release methylphenidate in ADHD: effectiveness on symptoms and impairment, and safety. Eur Child Adolesc Psychiatry. doi:10.1007/s00787-011-0202-4
Frazier TW, Weiss M, Hodgkins P, Manos MJ, Landgraf JM, Gibbins C (2010) Time course and predictors of health-related quality of life improvement and medication satisfaction in children diagnosed with attention-deficit/hyperactivity disorder treated with the methylphenidate transdermal system. J Child Adolesc Psychopharmacol 20:355–364
Gillberg C, Gillberg IC, Rasmussen P, Kadesjo B, Soderstrom H, Rastam M, Johnson M, Rothenberger A, Niklasson L (2004) Co-existing disorders in ADHD—implications for diagnosis and intervention. Eur Child Adolesc Psychiatry 13(Suppl 1):180–192
Goodman R (1997) The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 38:581–586
Graham J, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittmann RW, Dopfner M, Hamilton R, Hollis C, Holtmann M, Hulpke-Wette M, Lecendreux M, Rosenthal E, Rothenberger A, Santosh P, Sergeant J, Simonoff E, Sonuga-Barke E, Wong IC, Zuddas A, Steinhausen HC, Taylor E (2010) European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry 20:17–37
Klassen AF (2005) Quality of life of children with attention deficit hyperactivity disorder. Expert Rev Pharmacoecon Outcomes Res 5:95–103
Klassen AF, Miller A, Fine S (2004) Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics 114:e541–e547
Klassen AF, Miller A, Fine S (2006) Agreement between parent and child report of quality of life in children with attention-deficit/hyperactivity disorder. Child Care Health Dev 32:397–406
Newcorn JH, Spencer TJ, Biederman J, Milton DR, Michelson D (2005) Atomoxetine treatment in children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry 44:240–248
Raggi VL, Chronis AM (2006) Interventions to address the academic impairment of children and adolescents with ADHD. Clin Child Fam Psychol Rev 9:85–111
Ravens-Sieberer U, Bullinger M (1998) Assessing health-related quality of life in chronically ill children with the German KINDL: first psychometric and content analytical results. Qual Life Res 7:399–407
Ravens-Sieberer U, Erhart M, Wille N, Bullinger M (2008) Health-related quality of life in children and adolescents in Germany: results of the BELLA study. Eur Child Adolesc Psychiatry 17(Suppl 1):148–156
Riley AW, Spiel G, Coghill D, Dopfner M, Falissard B, Lorenzo MJ, Preuss U, Ralston SJ (2006) Factors related to health-related quality of life (HRQoL) among children with ADHD in Europe at entry into treatment. Eur Child Adolesc Psychiatry 15(Suppl 1):I38–I45
Rothenberger A, Becker A, Erhart M, Wille N, Ravens-Sieberer U (2008) Psychometric properties of the parent strengths and difficulties questionnaire in the general population of German children and adolescents: results of the BELLA study. Eur Child Adolesc Psychiatry 17(Suppl 1):99–105
Rothenberger A, Woerner W (2004) Strengths and difficulties questionnaire (SDQ)—evaluations and applications. Eur Child Adolesc Psychiatry 13(Suppl 2):II1–II2
Steinhausen HC (2010) Comorbidity and associated problems. In: Steinhausen HC, Rothenberger A, Döpfner M (eds) Handbook of ADHD. Kohlhammer S, Stuttgart, pp 172–185
Thompson MJ, Brooke XM, West CA, Johnson HR, Bumby EJ, Brodrick P, Pepe G, Laver-Bradbury C, Scott N (2004) Profiles, co-morbidity and their relationship to treatment of 191 children with AD/HD and their families. Eur Child Adolesc Psychiatry 13:234–242
Wehmeier PM, Schacht A, Barkley RA (2010) Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. J Adolesc Health 46:209–217
World Health Organization (1992) International classification of diseases (ICD-10), Geneva
Acknowledgments
The authors would like to thank Amina Elsner, MD (Shire AG), for constructive review. The authors take full responsibility for the content of the paper but thank Joanna Wright, DPhil (Caudex Medical, Oxford, UK, supported by Shire Development Inc.) for editorial assistance and collating the comments of authors and other named contributors. The OBSEER study was funded by UCB. Additional statistical analyses and the preparation of the manuscript were supported by Shire Development Inc.
Conflict of interest
Andreas Becker has nothing to disclose. Veit Roessner has acted as a consultant or on advisory boards and/or as a speaker for Lilly, Shire Pharmaceuticals Ltd, Medice and Novartis. Dieter Breuer has been a consultant for Lilly, Shire Pharmaceuticals Ltd, UCB and Medice. Manfred Döpfner has received research grants and/or acted as a consultant or on advisory boards for Lilly, Shire Pharmaceuticals Ltd, Medice and Vifor. Aribert Rothenberger has acted as a consultant or on advisory boards and/or as a speaker for Lilly, Shire Pharmaceuticals Ltd, Medice, Novartis and UCB. He has received research support from Shire Pharmaceuticals Ltd, the German Research Society and Schwaabe, and travel and educational grants from Shire Pharmaceuticals Ltd.
This article is part of a supplement sponsored by Shire Development Inc.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Becker, A., Roessner, V., Breuer, D. et al. Relationship between quality of life and psychopathological profile: data from an observational study in children with ADHD. Eur Child Adolesc Psychiatry 20 (Suppl 2), 267–275 (2011). https://doi.org/10.1007/s00787-011-0204-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-011-0204-2