Abstract
Background
This study aimed firstly to investigate whether youngsters referred for overweight treatment differ from non-referred overweight youngsters on the prevalence of psychiatric disorders and psychological symptoms. Secondly, the potentially moderating role of age, gender, socio-economic status and degree of overweight in the association of referral status and mental disorder in overweight youth was explored.
Methods
Participants were 155 overweight youngsters enrolled in an obesity treatment programme (mean age = 13.76; mean BMI = 33.99) and 73 non-referred overweight youngsters (mean age = 13.74; mean BMI = 27.35). The Structured Clinical Interview for DSM-IV-Childhood version and the Child version of the Eating Disorder Examination were administered and participants filled out the Children’s Depression Inventory, the Spence Children’s Anxiety Scale and the Youth Self Report. Parents were asked to complete the Child Behavior Checklist.
Results
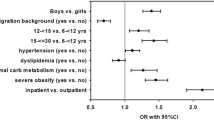
In the referred group 37.50% and in the non-referred group 23.29% of the participants met criteria for at least one mental disorder. In both groups, anxiety disorders were most prominent. Overall, a higher prevalence of mental disorders was found in the referred group. Referred youth displayed significantly more ‘full blown’ eating disorders and binge eating than non-referred youngsters and exhibited a significantly greater severity of self- and parent-reported internalizing symptoms. Referral was also associated with a significantly higher degree of overweight and significantly lower SES. After controlling for these pre-existing differences in degree of overweight and SES, only the greater severity of parent-reported internalizing symptoms in referred youth remained significant. Older age was generally predictive for the presence of mental disorders and in the non-referred group SES was positively associated with psychiatric disorder.
Conclusions
A substantial proportion of overweight youngsters suffer from mental disorders. Referral status and age are associated with the presence of psychopathology. However, differences between referred and non-referred youngsters are not as pronounced as expected on the basis of earlier research in the field.
Similar content being viewed by others
References
Achenbach TM (1991) Manual for the child behavior checklist 4–18 and 1991 profile. University of Vermont Department of Psychiatry, Burlington
Achenbach TM (1991) Manual for the youth self report and 1991 profile. University of Vermont, Department of Psychiatry, Burlington
Achenbach TM, Mcconaughy SH, Howell CT (1987) Child adolescent behavioral and emotional-problems-implications of cross-informant correlations for situational specificity. Psychol Bull 101:213–232
Agranat-Meged AN, Deitcher C, Goldzweig G, Leibenson L, Stein M, Galili-Weisstub E (2005) Childhood obesity and attention deficit/hyperactivity disorder: a newly described comorbidity in obese hospitalized children. Int J Eat Disord 37:357–359
Braet C, Mervielde I, Vandereycken W (1997) Psychological aspects of childhood obesity: a controlled study in a clinical and nonclinical sample. J Pediatr Psychol 22:59–71
Braet C, Tanghe A, Decaluwe V, Moens E, Rosseel Y (2004) Inpatient treatment for children with obesity: weight loss, psychological well-being, and eating behavior. J Pediatr Psychol 29:519–529
Britz B, Siegfried W, Ziegler A, Lamertz C, Herpertz-Dahlmann BM, Remschmidt H, Wittchen HU, Hebebrand J (2000) Rates of psychiatric disorders in a clinical study group of adolescents with extreme obesity and in obese adolescents ascertained via a population based study. Int J Obes 24:1707–1714
Bryant-Waugh RJ, Cooper PJ, Taylor CL, Lask BD (1996) The use of the eating disorder examination with children: a pilot study. Int J Eat Disord 19:391–397
Costello EJ, Egger H, Angold A (2005) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry 44:972–986
Decaluwe V, Braet C (2004) Assessment of eating disorder psychopathology in obese children and adolescents: interview versus self-report questionnaire. Behav Res Ther 42:799–811
Decaluwe V, Braet C (2003) Prevalence of binge-eating disorder in obese children and adolescents seeking weight-loss treatment. Int J Obes 27:404–409
Dreessen L, Stroux A, Weckx M (1998) Nederlandse vertaling van het gestructureerd klinisch interview voor DSM-IV—kind versie (KID-SCID; Versie 1.0). [Dutch translation of the structured clinical interview for DSM-IV—child edition]. Maastricht University, Maastricht
Dulcan M, Dunne JE, Ayres W, Arnold V, Benson RS, Bernet W, Bukstein O, Kinlan J, Leonard H, Licamele W, McClellan J, Sloan LE, Miles CM (1997) Practice parameters for the assessment and treatment of children, adolescents, and adults with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 36:S85–S121
Erermis S, Cetin N, Tamar M, Bukusoglu N, Akdeniz F, Goksen D (2004) Is obesity a risk factor for psychopathology among adolescents? Pediatr Int 46:296–301
Fairburn CG, Cooper Z (1993) The eating disorder examination (12th edn). In: Fairburn CG, Wilson T (eds) Binge eating: nature, assessment and treatment. Guilford Press, New York, 317–331
Fairburn CG, Harrison PJ (2003) Eating disorders. Lancet 361:407–416
Faith MS, Matz PE, Jorge MA (2002) Obesity—depression associations in the population. J Psychosom Res 53:935–942
Fredriks AM, van Buuren S, Wit JM, Verloove-Vanhorick SP (2000) Body index measurements in 1996–7 compared with 1980. Arch Dis Child 82:107–112
Friedman MA, Brownell KD (1995) Psychological correlates of obesity—moving to the next research generation. Psychol Bull 117:3–20
Glasofer DR, Tanofsky-Kraff M, Eddy KT, Yanovski SZ, Theim KR, Mirch MC, Ghorbani S, Ranzenhofer LM, Haaga D, Yanovski JA (2007) Binge eating in overweight treatment-seeking adolescents. J Pediatr Psychol 32:95–105
Herpertz S, Burgmer R, Stang A, de Zwaan M, Wolf AM, Chen-Stute A, Hulisz T, Jockel KH, Senf W (2006) Prevalence of mental disorders in normal-weight and obese individuals with and without weight loss treatment in a German urban population. J Psychosom Res 61:95–103
Hien D, Matzner FJ, First MB, Spitzer RL, Gibbon M, Williams JBW (1994) Structured clinical interview for DSM-IV—child edition (version 1.0). Columbia University, New York
Hollingshead A (1975) Four factor index of social status. Yale University Press, New Haven
Holtkamp K, Konrad K, Muller B, Heussen N, Herpertz S, Herpertz-Dahlmann B, Hebebrand J (2004) Overweight and obesity in children with attention-deficit/hyperactivity disorder. Int J Obes 28:685–689
Klein DN, Dougherty LR, Olino TM (2005) Toward guidelines for evidence-based assessment of depression in children and adolescents. J Clin Child Adolesc Psychol 34:412–432
Kovacs M (1996) Presentation and course of major depressive disorder during childhood and later years of the life span. J Am Acad Child Adolesc Psychiatry 35:705–715
Lamertz CM, Jacobi C, Yassouridis A, Arnold K, Henkel AW (2002) Are obese adolescents and young adults at higher risk for mental disorders? A community survey. Obes Res 10:1152–1160
Matzner F (1994) Videotapes as training tools for the development of the KID-SCID. In: American Academy of child and adolescent psychiatry 42nd annual meeting. American Academy of child and adolescent psychiatry, Washington, DC
Matzner F, Silva RR, Silvan M, Chowdhury M, Nastasi L (1997) Preliminary test–retest reliability of the KID-SCID. In: American Psychiatric Association annual meeting. American Psychiatric Association, San Diego
Muris P, Schmidt H, Merckelbach H (2000) Correlations among two self-report questionnaires for measuring DSM-defined anxiety disorder symptoms in children: the screen for child anxiety related emotional disorders and the Spence children’s anxiety scale. Pers Individ Dif 28:333–346
Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ (2003) Obesity and psychiatric disorder: developmental trajectories. Pediatrics 111:851–859
Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Grummer-Strawn LM, Curtin LR, Roche AF, Johnson CL (2002) Centers for disease control and prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health statistics version. Pediatrics 109:45–60
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164:942–948
Puhl RM, Brownell KD (2001) Bias, discrimination, and obesity. Obes Res 9:788–805
Rutter M (2006) Genes and behavior: nature–nurture interplay. Blackwell Publishing, Oxford
Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC (2006) Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry 63:824–830
Smith DC, Huber DL, Hall JA (2005) Psychometric evaluation of the structured clinical interview for DSM-IV childhood diagnoses (KID-SCID). J Hum Behav Soc Environ 11:23–40
Spence SH (1998) A measure of anxiety symptoms among children. Behav Res Ther 36:545–566
Spitzer RL, Williams JBW, Gibbon M (1986) Structured clinical interview for DSM-III-R. New York State Psychiatric Institute, Biometrics Research, New York
Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA (2004) Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. J Consult Clin Psychol 72:53–61
Timbremont B, Braet C (2002) Children’s depression inventory: Nederlandstalige versie [children’s depression inventory: Dutch version]. Swets & Zeitlinger, Lisse
Timbremont B, Braet C, Dreessen L (2004) Assessing depression in youth: relation between the children’s depression inventory and a structured interview. J Clin Child Adolesc Psychol 33:149–157
van Doorslaer E, Masseria C, Koolman X (2006) Inequalities in access to medical care by income in developed countries. Can Med Assoc J 174:177–183
Verhulst FC, Van der Ende J, Koot HM (1996) Handleiding voor de CBCL/4–18 [manual for the child behavior checklist and revised child behavior profile]. Sophia Children’s Hospital, Department of Child and Adolescent Psychiatry, Rotterdam
Verhulst FC, Van der Ende J, Koot HM (1997) Handleiding voor de youth self-report [manual for the youth self report and profile]. Sophia Children’s Hospital, Department of Child and Adolescent Psychiatry, Rotterdam
Vila G, Zipper E, Dabbas M, Bertrand C, Robert JJ, Ricour C, Mouren-Simeoni MC (2004) Mental disorders in obese children and adolescents. Psychosom Med 66:387–394
Watkins B, Frampton I, Lask B, Bryant-Waugh R (2005) Reliability and validity of the child version of the eating disorder examination: a preliminary investigation. Int J Eat Disord 38:183–187
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Vlierberghe, L., Braet, C., Goossens, L. et al. Psychiatric disorders and symptom severity in referred versus non-referred overweight children and adolescents. Eur Child Adolesc Psychiatry 18, 164–173 (2009). https://doi.org/10.1007/s00787-008-0717-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-008-0717-5