Abstract
A review of studies on the body fluid levels of neuroactive amino acids, including glutamate, glutamine, taurine, gamma-aminobutyric acid (GABA), glycine, tryptophan, d-serine, and others, in autism spectrum disorders (ASD) is given. The results reported in the literature are generally inconclusive and contradictory, but there has been considerable variation among the previous studies in terms of factors such as age, gender, number of subjects, intelligence quotient, and psychoactive medication being taken. Future studies should include simultaneous analyses of a large number of amino acids [including d-serine and branched-chain amino acids (BCAAs)] and standardization of the factors mentioned above. It may also be appropriate to use saliva sampling to detect amino acids in ASD patients in the future—this is noninvasive testing that can be done easily more frequently than other sampling, thus providing more dynamic monitoring.
Similar content being viewed by others
Autism spectrum disorders
The term autism spectrum disorders (ASD) refers to neurodevelopmental diseases that affect 1–2 % of children, according to the data on the broad array of ASD (Baron-Cohen et al. 2009). ASD is characterized by different levels of severity and occurs in all ethnic groups. Noto et al. (2014) reported that 1 out of 88 children aged 8 years will develop an ASD, with males more at risk than females. Blumberg et al. (2013) showed that the prevalence of ASD had risen 75 % from 2007 to 2012 in the United States. Feng et al. (2013) identified 12 studies when searching Chinese databases in 2013; the prevalence in these studies varied from 2.8 to 29.5/10,000.
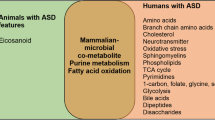
ASD is characterized by impaired social interaction skills combined with restrictive/repetitive behaviors (American Psychiatric Association 2013). Genetic predisposition and environmental factors undoubtedly have effects on the pathophysiology of ASD, but the precise mechanisms related to the pathophysiology of ASD are unknown and definitive methods for prevention or treatment are lacking (Blaylock 2008). DSM-5 proposes that ASD symptoms must appear in the early childhood (infant) (American Psychiatric Association 2013). Receiving diagnosis at an early stage of development could contribute to the early intervention and therapy, benefiting both patients and their families (Zwaigenbaum et al. 2015; Sacrey et al. 2015; Brian et al. 2015). However, behavioral abnormalities are often overlooked in the early stage of ASD, even experienced professionals involved in pediatric healthcare (Howlin and Asgharian 1999). Therefore, many researchers have been trying to establish quantitative diagnostic criteria that could contribute to an early and more accurate ASD diagnosis. Many interacting factors are probably contributing to the etiology of ASD, and these potential factors are described in several excellent review articles (Lam et al. 2006; Pardo and Eberhart 2007; Aoki et al. 2012; Parellada et al. 2014; Lozano et al. 2015; Rozas et al. 2015; Subramanian et al. 2015; Zhang et al. 2015; Martin et al. 2016; Muller et al. 2016; Park et al. 2016); this review focuses on amino acids.
Neuroactive amino acids
Several lines of evidence have shown that changes (e.g., availability, metabolism, and/or receptor activity) in neuroactive amino acids associated with central brain functions may play a role in the pathogenesis and/or pharmacotherapy of several psychiatric disorders (e.g., schizophrenia and mood disorders) that have symptoms, such as cognitive impairment and problems with social interactions, in common with ASD (Coyle 2006; Grant et al. 2006; Lam et al. 2006; Labrie et al. 2008; Ongür et al. 2008; Yüksel and Öngür 2010; Durrant and Heresco-Levy 2014). Several preclinical and clinical studies have implicated neuroactive amino acids in the etiology of ASD, fragile X syndrome, and tuberous sclerosis complex (TSC), but most of these studies have focused on glutamate, GABA, and/or glutamine (El-Ansary and Al-Ayadhi 2014; Rojas 2014; Santini et al. 2014; Rozas et al. 2015; Cochran et al. 2015; Lozano et al. 2015; Robertson et al. 2016). Other amino acids could also be involved and it may be important to conduct comprehensive studies in which a number of these amino acids are investigated simultaneously. Due to the potential role of neuroactive amino acids in the pathogenesis and treatment of ASD, monitoring changes in their concentrations in body fluids are also important in case they may be relevant to the early diagnosis and intervention in patients with ASD. This paper reviews the literature on such measurements of several of these important compounds in body fluids in ASD subjects.
Glutamate (GLU)
GLU, which is highly concentrated in brain, is the primary excitatory neurotransmitter (Naaijen et al. 2015). GLU normally has a protective effect with regard to neural plasticity and cognitive function, but excessive GLU may be neurotoxic, leading to death of neurons and glia (Olney 1969; Manev et al. 1989) and may possibly play a role in the pathogenesis of psychiatric disorders, such as ASD (Sheldon and Robinson 2007). Ghanizadeh (2011) and El-Ansary and Al-Ayadhi (2014) showed that GLU is involved in neuroinflammation in ASD, and Ghanizadeh and Namazi (2010) proposed GLU and homocysteine as targets for therapy of ASD patients’ irritability and aggression. A hyperglutamatergic hypothesis of ASD has been proposed (Fatemi 2008; Blaylock and Strunecka 2009). Fatemi et al. (2002) showed that the levels of GAD 65 kDa and GAD 67 kDa proteins, both of which are involved in converting GLU to gamma-aminobutyric acid (GABA), are reduced in the brains of patients with ASD, resulting in the increased levels of GLU in the brain.
Studies on GLU levels in the plasma of patients with ASD compared to healthy controls (HCs) are contradictory, with some reporting increased levels (Moreno-Fuenmayor et al. 1996; Aldred et al. 2003; MacDermot et al. 2005; Shimmura et al. 2011; Tirouvanziam et al. 2011; Naushad et al. 2013; El-Ansary and Al-Ayadhi 2014; Cai et al. 2016) and some decreased levels (El-Ansary 2016). In addition, increased levels have been reported in serum (Shinohe et al. 2006) and decreased levels in platelets (Rolf et al. 1993) and urine samples (Evans et al. 2008; Yap et al. 2010; Nadal-Desbarats et al. 2014). Some studies have used magnetic resonance spectroscopy (MRS) to measure amino acid levels in patients with ASD and have reported that patients with ASD have increased GLU levels in brain (Page et al. 2006; Joshi et al. 2012; Hassan et al. 2013). Cochran et al. (2015) showed that, compared with HCs, patients with ASD had increased glutamine (GLN) levels, decreased GABA levels, and no difference in GLU levels in brain. However, van Elst et al. (2014) reported that GLU and GLN levels were decreased in ASD brains.
Glutamine (GLN)
GLU is stored in the form of GLN in astrocytes until it is transferred to presynaptic terminals and converted back to GLU (Magistretti and Pellerin 1999). Ghanizadeh (2010) reported that a glutamine (GLN) synthetase inhibitor may improve inflammation in ASD. Shimmura et al. (2011) suggested that the level of GLN in plasma could be a screening test for detecting ASD in children, especially those with a normal intelligence quotient (IQ). In studies of GLN levels in ASD patients compared to HCs, plasma (Moreno-Fuenmayor et al. 1996; Aldred et al. 2003; Shimmura et al. 2011; Tirouvanziam et al. 2011; Good 2011a; Tu et al. 2012; El-Ansary 2016) and platelet (Rolf et al. 1993) levels have been reported to be decreased, serum levels to be no different (Shinohe et al. 2006), and urine levels either increased (Noto et al. 2014) or decreased (Evans et al. 2008).
Taurine (TAUR)
TAUR is an osmoregulator and neuromodulator that suppresses vasopressin and has been reported to be depleted in urine of autistic children (Good 2011a). However, in other studies on TAUR levels in ASD patients compared to HCs, plasma levels have been reported to be increased (Moreno-Fuenmayor et al. 1996; Shimmura et al. 2011; Kuwabara et al. 2013) or decreased (Geier et al. 2009; Kern et al. 2011; Tu et al. 2012), and levels in urine samples to be increased (Yap et al. 2010; Nadal-Desbarats et al. 2014) or decreased (Ming et al. 2012). Although the results reported on TAUR levels in plasma and urine samples are contradictory, there is a consistent opinion that TAUR plays a protective role in patients with ASD (Good 2011a, b; Omura et al. 2015). Kuwabara et al. (2013) showed elevated plasma TAUR levels in adults with ASD and proposed that TAUR is compensatory against pathogenesis of ASD, such as that caused by oxidative stress.
Gamma-aminobutyric acid (GABA)
The balance between GABA and GLU, inhibitory and excitatory neurotransmitters, respectively, is very important for brain function, and many psychiatric and neurological disorders may be the result of imbalance between GABA and GLU (Erickson et al. 2013; Rojas 2014; Robertson et al. 2016). Reduced GABAergic action in human and animal models of ASD has been proposed to be one of the reasons for an imbalance between excitation and inhibition (Rubenstein and Merzenich 2003; Gogolla et al. 2009; Blatt and Fatemi 2011; Ito 2016; Robertson et al. 2016). However, compared with HCs, GABA levels in plasma have been reported to be increased in ASD subjects (Dhossche et al. 2002; El-Ansary and Al-Ayadhi 2014). Dhossche et al. (2002) reported that plasma GABA levels tended to decrease with age in ASD. Compared with HCs, GABA levels in platelets have been reported to be decreased in ASD (Rolf et al. 1993) while those in urine samples increased (Cohen 2002). Neuroimaging techniques reported decreased GABA in brains of ASD patients (Kubas et al. 2012; Gaetz et al. 2014; Rojas et al. 2014; Omura et al. 2015; Cochran et al. 2015). Rojas et al. (2014) reported that the left perisylvian GABA levels were decreased in patients with ASD and their unaffected siblings. Recently, studies using oxytocin to treat animal models of ASD reported that oxytocin can increase excitatory GABA and enhance hyperglutamatergic activity (Tyzio et al. 2014; Young and Barrett 2015).
Glycine (GLY)
GABA and GLY are major inhibitory neurotransmitters in the central nervous system (CNS). They act on receptors coupled to chloride channels which play an important role in normal function of the CNS (Ito 2016). GABA and GLY depolarize membrane potentials, acting as excitatory neurotransmitters during early development (Wang et al. 2002; Yamada et al. 2004; Kaila et al. 2014). They shift from excitatory to inhibitory neurotransmitters at birth and in maturation, and if that does not happen it may result in neurological disorders, including ASD (Tyzio et al. 2006, 2014). However, in some parts of the brain, GLY acts as a coagonist at NMDA GLU receptors (Martina et al. 2003; Baptista and Varanda 2005; Kim et al. 2005; Basu et al. 2009), and it has been suggested that the GLY/d-serine site on the NMDA receptor could be a target for ASD therapy. Compared with HCs, GLY levels in plasma (Tirouvanziam et al. 2011) and serum (Shinohe et al. 2006) of ASD subjects have been reported to be unchanged, and levels in urine samples reported to be increased (Nadal-Desbarats et al. 2014; Noto et al. 2014) or decreased (Evans et al. 2008; Ming et al. 2012).
Tryptophan (TRP)
Serotonin (5-hydroxtryptamine, 5-HT) is an important neurotransmitter, and TRP is the precursor of serotonin (Zhang et al. 2015). Dysfunction of serotonin systems are implicated in some forms of ASD, and may contribute to social interaction impairments (Lam et al. 2006; Rubin et al. 2013; Yang et al. 2014). Whole blood serotonin has been reported to be elevated in at least 25 % of ASD children (Muller et al. 2016). However, reducing TRP in the diet can impair social behavior in patients (McDougle et al. 1996) and mice (Zhang et al. 2015) and increasing TRP in the diet has been reported to improve social behavior in mice (Zhang et al. 2015). Compared with HCs, TRP levels in plasma have been reported to be decreased in ASD (Tirouvanziam et al. 2011; Tu et al. 2012; Naushad et al. 2013), while Noto et al. (2014) reported levels to be increased in urine samples and Kałużna-Czaplińska et al. (2014) reported them to be decreased.
d-Serine
In the recent years, d-serine in the brain has been the subject of extensive research (Fuchs et al. 2005, 2011; Nunes et al. 2012; Billard 2015; Sacchi et al. 2016). d-Serine is an important amino acid in glutamatergic transmission (Fuchs et al. 2005) and is a potent coagonist at NMDA receptors in some mammalian brain areas and possibly involved in the pathogenesis of several psychiatric and neurological disorders, such as schizophrenia (Labrie et al. 2008; Nunes et al. 2012; Balu and Coyle 2015; Ozeki et al. 2016), bipolar disorder (Yamada et al. 2004; Young and Barrett 2015), depression (Hashimoto et al. 2015, 2016; Deutschenbaur et al. 2016), Alzheimer’s disease (Paula-Lima et al. 2013; Madeira et al. 2015), and addiction (D’Ascenzo et al. 2014; Seif et al. 2015; Liu et al. 2016). GLY has high affinity for extrasynaptic NMDA receptors, while d-serine has high affinity for synaptic NMDA receptors (Vizi et al. 2013).
There is a paucity of studies on body fluid levels of d-serine in ASD. In 2006, Shinohe et al. (2006) showed that d-serine and l-serine levels in serum were no different between adult patients with ASD and HCs. Comparing with HCs, Tirouvanziam et al. (2011) showed that combined serine levels in plasma were decreased in ASD. In studies on urine samples, Kałużna-Czaplińska et al. (2014) reported that l-serine levels were decreased in ASD, and Noto et al. (2014) reported that l-serine levels were increased, while Evans et al. (2008) and Ming et al. (2012) showed that the combined serine levels were decreased. In the studies in which combined serine levels were reported, the d-serine and l- serine were not measured separately.
Other amino acids
The metabolism of homocysteine is associated closely with folic acid and Vitamin B12 (Ghanizadeh et al. 2012; Desai et al. 2016). Desai et al. (2016) showed that a lack of folic acid may be involved in the pathogenesis of ASD. Bala et al. (2016) reported low plasma levels of Vitamin B12 in ASD compared to values in HCs. James et al. (2004), and Bala et al. (2016) reported that the concentration of homocysteine in plasma with ASD patients is low. However, other studies showed that homocysteine levels were increased in ASD patients compared with HCs: Tu et al. (2012) reported levels in plasma, Ali et al. (2011) and Paşca et al. (2006) reported levels in serum, and Noto et al. (2014) and Puig-Alcaraz et al. (2015) reported levels in urine samples, and all were reported to be increased. Puig-Alcaraz et al. (2015) found that increased urinary levels of homocysteine correlated directly with the severity of deficit in communication skills in ASD.
Arginine is an essential precursor for the synthesis of proteins and nitric oxide, and it can spare GLN, detoxify ammonia, and increase brain blood flow (Good 2011a). Compared with HCs, arginine levels in plasma of ASD patients have been reported to be increased (Kuwabara et al. 2013) or no different (Tirouvanziam et al. 2011).
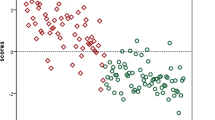
Table 1 shows the reported levels of neuroactive amino acids in patients with ASD in comparison with HCs and includes some other amino acids not mentioned previously in this review (leucine, lysine, citrulline, alanine, valine, isoleucine, threonine, proline, methionine, aspartate, asparagine, phenylalanine, tyrosine, and histidine). Leucine, isoleucine, and valine are all termed branched-chain amino acids (BCAAs) and share a transport system with large, neutral amino acids (LNAAs), such as tryptophan, tyrosine, and phenylalanine which are the precursors of the neurotransmitter amines 5-hydroxytryptamine (5-HT, serotonin) and the catecholamines (Fernstrom 2005). Arnold et al. (2003) reported that the level of the essential amino acids valine, leucine, phenylalanine, and lysine in ASD was 58 % compared to HCs. Although there is a paucity of studies on the levels of BCCAs in ASD, most of the studies report a reduction of BCAA levels in autistic subjects (see Table 1 and the references mentioned therein), suggesting that future research in this area is warranted.
Discussion
Overall, the results on amino acid levels in ASD reported in the literature are, with the possible exception of the BCAAs, inconclusive, and contradictory. Table 1 is a summary of reported differences between ASD patients and HCs in the levels of amino acids. BCAAs are essential amino acids that make up about 1/3 of muscle protein, and these deficiencies may affect muscle and connective tissue integrity in ASD subjects (Evans et al. 2008). It has been suggested that BCAA deficiencies may be related to poor nutrition due to unusual food preferences in ASD children (Arnold et al. 2003).
In studies on amino acids levels in ASD subjects reported in the literature, there has been considerable variation in terms of factors such as age, gender, number of subjects, IQ, and psychoactive medication being taken. Future studies could be improved by standardizing these factors and analyzing levels of several amino acids (including d-serine and BCAAs) simultaneously.
Recently, many studies have focused on saliva samples to detect cortisol which is a good indicator of stress pressure and behavior recovery in patients with ASD (Putnam et al. 2012; Tordjman et al. 2014; Abdulla and Hegde 2015; Edmiston et al. 2015). Because of the ease of collecting saliva, it is convenient for caregivers to help patients, even infants and toddlers (Putnam et al. 2012), to collect samples at home. There should be reduced emotional changes compared to collecting blood samples and thus possibly increased accuracy of results (Woods et al. 2008). Unfortunately, few studies on amino acids in saliva with ASD patients have been done. It may be useful to employ saliva sampling combined with standardized conditions as mentioned in the discussion above to detect amino acids in ASD patients routinely in the future—this is noninvasive testing that can be readily done more frequently than other sampling, thus providing more dynamic monitoring.
References
Abdulla AM, Hegde AM (2015) Salivary cortisol levels and its implication on behavior in children with autism during dental treatment. J Clin Pediatr Dent 39:128–132
Aldred S, Moore KM, Fitzgerald M, Waring RH (2003) Plasma amino acid levels in children with autism and their families. J Autism Dev Disord 33:93–97
Ali A, Waly MI, Al-Farsi YM et al (2011) Hyperhomocysteinemia among Omani autistic children: a case-control study. Acta Biochim Pol 58:547–551
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric, Washington, DC
Aoki Y, Kasai K, Yamasue H (2012) Age-related change in brain metabolite abnormalities in autism: a meta-analysis of proton magnetic resonance spectroscopy studies. Transl Psychiatry 2(e69):1–12
Arnold GL, Hyman SL, Mooney RA, Kirby RS (2003) Plasma amino acids profiles in children with autism: potential risk of nutritional deficiencies. J Autism Dev Disord 33:449–454
Bala KA, Dogan M, Mutluer T et al (2016) Plasma amino acid profile in autism spectrum disorder (ASD). Eur Rev Med Pharcol Sci 20:923–929
Balu DT, Coyle JT (2015) The NMDA receptor “glycine modulatory site” in schizophrenia: d-serine, glycine, and beyond. Curr Opin Pharmacol 20:109–115
Baptista V, Varanda WA (2005) Glycine binding site of the synaptic NMDA receptor in subpostremal NTS neurons. J Neurophysiol 94:147–152
Baron-Cohen S, Scott FJ, Allison C et al (2009) Prevalence of autism-spectrum conditions: UK school-based population study. Br J Psychiatry 194:500–509
Basu AC, Tsai GE, Ma C-L et al (2009) Targeted disruption of serine racemase affects glutamatergic neurotransmission and behavior. Mol Psychiatry 14:719–727
Billard J-M (2015) d-Serine in the aging hippocampus. J Pharm Biomed Anal 116:18–24
Blatt GJ, Fatemi SH (2011) Alterations in GABAergic biomarkers in the autism brain: research findings and clinical implications. Anat Rec (Hoboken) 294:1646–1652
Blaylock RL (2008) A possible central mechanism in autism spectrum disorders, part 1. Altern Ther Health Med 14:46–53
Blaylock RL, Strunecka A (2009) Immune-glutamatergic dysfunction as a central mechanism of the autism spectrum disorders. Curr Med Chem 16:157–170
Blumberg SJ, Bramlett MD, Kogan MD et al (2013) Changes in prevalence of parent-reported autism spectrum disorder in school-aged U.S. children: 2007 to 2011–2012. Natl Health Stat Rep 65:1–11
Brian J, Bryson SE, Smith IM et al (2016) Stability and change in autism spectrum disorder diagnosis from age 3 to middle childhood in a high-risk sibling cohort. Autism 20:888–892
Cai J, Ding L, Zhang J-S et al (2016) Elevated plasma levels of glutamate in children with autism spectrum disorders. NeuroReport 27:272–276
Cochran DM, Sikoglu EM, Hodge SM et al (2015) Relationship among glutamine, γ-aminobutyric acid, and social cognition in autism spectrum disorders. J Child Adolesc Psychopharmacol 25:314–322
Cohen BI (2002) The significance of ammonia/gamma-aminobutyric acid (GABA) ratio for normality and liver disorders. Med Hypotheses 59:757–758
Coyle JT (2006) Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell Mol Neurobiol 26:365–384
D’Ascenzo M, Podda MV, Grassi C (2014) The role of d-serine as co-agonist of NMDA receptors in the nucleus accumbens: relevance to cocaine addiction. Front Synaptic Neurosci 6:16
Desai A, Sequeira JM, Quadros EV (2016) The metabolic basis for developmental disorders due to defective folate transport. Biochimie 126:31–42
Deutschenbaur L, Beck J, Kiyhankhadiv A et al (2016) Role of calcium, glutamate and NMDA in major depression and therapeutic application. Prog Neuropsychopharmacol Biol Psychiatry 64:325–333
Dhossche D, Applegate H, Abraham A et al (2002) Elevated plasma gamma-aminobutyric acid (GABA) levels in autistic youngsters: stimulus for a GABA hypothesis of autism. Med Sci Monit 8:1–6
Durrant AR, Heresco-Levy U (2014) d-Serine in neuropsychiatric disorders: new advances. Adv Psychiatry 2014:1–16
Edmiston EK, Merkle K, Corbett BA (2015) Neural and cortisol responses during play with human and computer partners in children with autism. Soc Cogn Affect Neurosci 10:1074–1083
El-Ansary A (2016) Data of multiple regressions analysis between selected biomarkers related to glutamate excitotoxicity and oxidative stress in Saudi autistic patients. Data Brief 7:111–116
El-Ansary A, Al-Ayadhi L (2014) GABAergic/glutamatergic imbalance relative to excessive neuroinflammation in autism spectrum disorders. J Neuroinflammation 11:189
Erickson CA, Wink LK, Early MC et al (2013) Brief report: pilot single-blind placebo lead-in study of acamprosate in youth with autistic disorder. J Autism Dev Disord 44:981–987
Evans C, Dunstan HR, Rothkirch T et al (2008) Altered amino acid excretion in children with autism. Nutr Neurosci 11:9–17
Fatemi SH (2008) The hyperglutamatergic hypothesis of autism. Prog Neuropsychopharmacol Biol Psychiatry 32:911
Fatemi SH, Halt AR, Stary JM et al (2002) Glutamic acid decarboxylase 65 and 67 kDa proteins are reduced in autistic parietal and cerebellar cortices. Biol Psychiatry 52:805–810
Feng L, Li C, Chiu H et al (2013) Autism spectrum disorder in Chinese populations: a brief review. Asia Pac Psychiatry 5:54–60
Fernstrom JD (2005) Branched-chain amino acids and brain function. J Nutr 135:1539–1546
Fuchs SA, Berger R, Klomp LWJ, de Koning TJ (2005) d-Amino acids in the central nervous system in health and disease. Mol Genet Metab 85:168–180
Fuchs SA, Berger R, de Koning TJ (2011) d-Serine: the right or wrong isoform? Brain Res 1401:104–117
Gaetz W, Bloy L, Wang DJ et al (2014) GABA estimation in the brains of children on the autism spectrum: measurement precision and regional cortical variation. Neuroimage 86:1–9
Geier DA, Kern JK, Garver CR et al (2009) A prospective study of transsulfuration biomarkers in autistic disorders. Neurochem Res 34:386–393
Ghanizadeh A (2010) Methionine sulfoximine may improve inflammation in autism, a novel hypothesized treatment for autism. Arch Med Res 41:651–652
Ghanizadeh A (2011) Could fever and neuroinflammation play a role in the neurobiology of autism? A subject worthy of more research. Int J Hyperthermia 27:737–738
Ghanizadeh A, Namazi MR (2010) A possible research and clinical implication of association of homocysteine and glutamate levels in brain for management of aggression. Int J Dev Neurosci 28:125
Ghanizadeh A, Akhondzadeh S, Hormozi M et al (2012) Glutathione-related factors and oxidative stress in autism, a review. Curr Med Chem 19:4000–4005
Gogolla N, Leblanc JJ, Quast KB et al (2009) Common circuit defect of excitatory-inhibitory balance in mouse models of autism. J Neurodev Disord 1:172–181
Good P (2011a) Do salt cravings in children with autistic disorders reveal low blood sodium depleting brain taurine and glutamine? Med Hypotheses 77:1015–1021
Good P (2011b) Does fever relieve autistic behavior by improving brain blood flow? Neuropsychol Rev 21:66–67
Grant SL, Shulman Y, Tibbo P et al (2006) Determination of d-serine and related neuroactive amino acids in human plasma by high-performance liquid chromatography with fluorimetric detection. J Chromatogr B 844:278–282
Hashimoto K, Yoshida T, Ishikawa M et al (2015) Increased serum levels of serine enantiomers in patients with depression. Acta Neuropsychiatr 28:173–178
Hashimoto K, Bruno D, Nierenberg J et al (2016) Abnormality in glutamine-glutamate cycle in the cerebrospinal fluid of cognitively intact elderly individuals with major depressive disorder: a 3-year follow-up study. Transl Psychiatry 6:744–749
Hassan TH, Abdelrahman HM, Abdel Fattah NR et al (2013) Blood and brain glutamate levels in children with autistic disorder. Res Autism Spectr Disord 7:541–548
Howlin P, Asgharian A (1999) The diagnosis of autism and Asperger syndrome: findings from a survey of 770 families. Dev Med Child Neurol 41:834–839
Ito S (2016) GABA and glycine in the developing brain. J Physiol Sci 66:375–379
James SJ, Cutler P, Melnyk S et al (2004) Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am J Clin Nutr 80:1611–1617
Joshi G, Biederman J, Wozniak J et al (2012) Magnetic resonance spectroscopy study of the glutamatergic system in adolescent males with high-functioning autistic disorder: a pilot study at 4T. Eur Arch Psychiatry Clin Neurosci 263:379–384
Kaila K, Price TJ, Payne JA et al (2014) Cation-chloride cotransporters in neuronal development, plasticity and disease. Nat Rev Neurosci 15:637–654
Kałużna-Czaplińska J, Żurawicz E, Struck W, Markuszewski M (2014) Identification of organic acids as potential biomarkers in the urine of autistic children using gas chromatography/mass spectrometry. J Chromatogr B 966:70–76
Kern JK, Geier DA, Adams JB et al (2011) A clinical trial of glutathione supplementation in autism spectrum disorders. Med Sci Monit 17:677–682
Kim PM, Aizawa H, Kim PS et al (2005) Serine racemase: activation by glutamate neurotransmission via glutamate receptor interacting protein and mediation of neuronal migration. Proc Natl Acad Sci USA 102:2105–2110
Kubas B, Kułak W, Sobaniec W et al (2012) Metabolite alterations in autistic children: a 1H MR spectroscopy study. Adv Med Sci 57:152–156
Kuwabara H, Yamasue H, Koike S et al (2013) Altered metabolites in the plasma of autism spectrum disorder: a capillary electrophoresis time-of-flight mass spectroscopy study. PLoS One 8:73814
Labrie V, Lipina T, Roder JC (2008) Mice with reduced NMDA receptor glycine affinity model some of the negative and cognitive symptoms of schizophrenia. Psychopharmacology 200:217–230
Lam KSL, Aman MG, Arnold LE (2006) Neurochemical correlates of autistic disorder: a review of the literature. Res Dev Disabil 27:254–289
Liu Z-Q, Gu X-H, Yang Y-J et al (2016) d-Serine in the nucleus accumbens region modulates behavioral sensitization and extinction of conditioned place preference. Pharmacol Biochem Behav 143:44–56
Lozano R, Martinez-Cerdeno V, Hagerman RJ (2015) Advances in the understanding of the Gabaergic neurobiology of FMR1expanded alleles leading to targeted treatments for fragile X spectrum disorder. Curr Pharm Des 21(34):4972–4979
MacDermot KD, Bonora E, Sykes N et al (2005) Identification of FOXP2 truncation as a novel cause of developmental speech and language deficits. Am J Hum Genet 76:1074–1080
Madeira C, Lourenco MV, Vargas-Lopes C et al (2015) d-Serine levels in Alzheimer’s disease: implications for novel biomarker development. Transl Psychiatry 5:561
Magistretti PJ, Pellerin L (1999) Cellular mechanisms of brain energy metabolism and their relevance to functional brain imaging. Philos Trans R Soc Lond B Biol Sci 354:1155–1163
Manev H, Favaron M, Guidotti A, Costa E (1989) Delayed increase of Ca2+ influx elicited by glutamate: role in neuronal death. Mol Pharmacol 36:106–112
Martin BS, Martinez-Botella G, Loya CM, Salituro FG, Robichaud AJ, Huntsman MM, Ackley MA, Doherty JJ, Corbin JG (2016) Rescue of deficient amygdala tonic γ-aminobutyric acidergic currents in the Fmr −/y mouse model of fragile X syndrome by a novel γ-aminobutyric acid type A receptor-positive allosteric modulator. J Neurosci Res 94:568–578
Martina M, Krasteniakov NV, Bergeron R (2003) d-Serine differently modulates NMDA receptor function in rat CA1 hippocampal pyramidal cells and interneurons. J Physiol 548:411–423
McDougle CJ, Naylor ST, Cohen DJ et al (1996) Effects of tryptophan depletion in drug-free adults with autistic disorder. Arch Gen Psychiatry 53:993–1000
Ming X, Stein TP, Barnes V et al (2012) Metabolic perturbance in autism spectrum disorders: a metabolomics study. J Proteome Res 11:5856–5862
Moreno H, Borjas L, Arrieta A et al (1992) Clinical heterogeneity of the autistic syndrome: a study of 60 families. Invest Clin 33:13–31
Moreno-Fuenmayor H, Borjas L, Arrieta A et al (1996) Plasma excitatory amino acids in autism. Invest Clin 37:113–128
Muller CL, Anacker AMJ, Veenstra-Vanderweele J (2016) The serotonin system in autism spectrum disorder: from biomarker to animal models. Neuroscience 321:24–41
Naaijen J, Lythgoe DJ, Amiri H et al (2015) Fronto-striatal glutamatergic compounds in compulsive and impulsive syndromes: a review of magnetic resonance spectroscopy studies. Neurosci Biobehav Rev 52:74–88
Nadal-Desbarats L, Aïdoud N, Emond P et al (2014) Combined 1H-NMR and 1H–13C HSQC-NMR to improve urinary screening in autism spectrum disorders. Analyst 139:3460–3468
Naushad SM, Jain JMN, Prasad CK et al (2013) Autistic children exhibit distinct plasma amino acid profile. Indian J Biochem Biophys 50:474–478
Noto A, Fanos V, Barberini L et al (2014) The urinary metabolomics profile of an Italian autistic children population and their unaffected siblings. J Matern Fetal Neonatal Med 27:46–52
Nunes EA, MacKenzie EM, Rossolatos D et al (2012) d-Serine and schizophrenia: an update. Expert Rev Neurother 12:801–812
Olney JW (1969) Brain lesions, obesity, and other disturbances in mice treated with monosodium glutamate. Science 164:719–721
Omura Y, Lu D, Jones MK et al (2015) Early detection of autism (ASD) by a non-invasive quick measurement of markedly reduced acetylcholine & DHEA and increased β-Amyloid (1-42), asbestos (chrysotile), titanium dioxide, Al, Hg & often coexisting virus infections (CMV, HPV 16 and 18), bacterial infections etc. in the brain and corresponding safe individualized effective treatment. Acupunct Electrother Res 40:157–187
Ongür D, Jensen JE, Prescot AP et al (2008) Abnormal glutamatergic neurotransmission and neuronal-glial interactions in acute mania. Biol Psychiatry 64:718–726
Ozeki Y, Sekine M, Fujii K et al (2016) Phosphoserine phosphatase activity is elevated and correlates negatively with plasma d-serine concentration in patients with schizophrenia. Psychiatry Res 237:344–350
Page LA, Daly E, Schmitz N et al (2006) In vivo 1H-magnetic resonance spectroscopy study of amygdala-hippocampal and parietal regions in autism. Am J Psychiatry 163:2189–2192
Pardo CA, Eberhart CG (2007) The neurobiology of autism. Brain Pathol 17:434–447
Parellada M, Penzol MJ, Pina L, Moreno C, Gonzalez-Vioque D, Zalsman G, Arango C (2014) The neurobiology of autism spectrum disorders. Eur Psychiatry 29:11–19
Park HR, Lee JM, Moon HE, Lee DS, Kim B-N, Kim J, Kim DG, Paek SH (2016) A short review on the current understanding of autism spectrum disorders. Exp Neurobiol 25(1):1–13
Paşca SP, Nemeş B, Vlase L et al (2006) High levels of homocysteine and low serum paraoxonase 1 arylesterase activity in children with autism. Life Sci 78:2244–2248
Paula-Lima AC, Brito-Moreira J, Ferreira ST (2013) Deregulation of excitatory neurotransmission underlying synapse failure in Alzheimer’s disease. J Neurochem 126:191–202
Perry TL, Hansen S, Christie RG (1978) Amino compounds and organic acids in CSF, plasma, and urine of autistic children. Biol Psychiatry 13:575–586
Puig-Alcaraz C, Fuentes-Albero M, Calderón J et al (2015) Increased homocysteine levels correlate with the communication deficit in children with autism spectrum disorder. Psychiatry Res 229:1031–1037
Putnam SK, Lopata C, Fox JD et al (2012) Comparison of saliva collection methods in children with high-functioning autism spectrum disorders: acceptability and recovery of cortisol. Child Psychiatry Hum Dev 43:560–573
Robertson CE, Ratai E-M, Kanwisher N (2016) Reduced GABAergic action in the autistic brain. Curr Biol 26:80–85
Rojas DC (2014) The role of glutamate and its receptors in autism and the use of glutamate receptor antagonists in treatment. J Neural Transm 121:891–905
Rojas DC, Singel D, Steinmetz S et al (2014) Decreased left perisylvian GABA concentration in children with autism and unaffected siblings. Neuroimage 86:28–34
Rolf LH, Haarmann FY, Grotemeyer K-H, Kehrer H (1993) Serotonin and amino acid content in platelets of autistic children. Acta Psychiatr Scand 87:312–316
Rozas NS, Redell JB, McKenna J III, Moore AN, Gambello MJ, Dash PK (2015) Prolonging the survival of Tsc2 conditional knockout mice by glutamine supplementation. Biochem Biophys Res Commun 457(4):635–639
Rubenstein JLR, Merzenich MM (2003) Model of autism: increased ratio of excitation/inhibition in key neural systems. Genes Brain Behav 2:255–267
Rubin DH, Althoff RR, Ehli EA et al (2013) Candidate gene associations with withdrawn behavior. J Child Psychol Psychiatry 54:1337–1345
Sacchi S, Binelli G, Pollegioni L (2016) G72 primate-specific gene: a still enigmatic element in psychiatric disorders. Cell Mol Life Sci 73:2029–2039
Sacrey L-AR, Bennett JA, Zwaigenbaum L (2015) Early infant development and intervention for autism spectrum disorder. J Child Neurol 30:1921–1929
Santini AC, Pierantoni GM, Gerlini R et al (2014) Glix 13, a new drug acting on glutamatergic pathways in children and animal models of autism spectrum disorders. BioMed Res Int 2014:234295
Seif T, Simms JA, Lei K et al (2015) d-Serine and d-cycloserine reduce compulsive alcohol intake in rats. Neuropsychopharmacol 40:2357–2367
Sheldon AL, Robinson MB (2007) The role of glutamate transporters in neurodegenerative diseases and potential opportunities for intervention. Neurochem Int 51:333–355
Shimmura C, Suda S, Tsuchiya KJ et al (2011) Alteration of plasma glutamate and glutamine levels in children with high-functioning autism. PLoS One 6:25340
Shinohe A, Hashimoto K, Nakamura K et al (2006) Increased serum levels of glutamate in adult patients with autism. Prog Neuropsychopharmacol Biol Psychiatry 30:1472–1477
Subramanian M, Timmerman CK, Schwartz JL, Pham DL, Meffert KM (2015) Characterizing autism spectrum disorders by key biochemical pathways. Front Neurosci 9(art. 313):1–18
Tirouvanziam R, Obukhanych TV, Laval J et al (2011) Distinct plasma profile of polar neutral amino acids, leucine, and glutamate in children with autism spectrum disorders. J Autism Dev Disord 42:827–836
Tordjman S, Anderson GM, Kermarrec S et al (2014) Altered circadian patterns of salivary cortisol in low-functioning children and adolescents with autism. Psychoneuroendocrinology 50:227–245
Tu W-J, Chen H, He J (2012) Application of LC-MS/MS analysis of plasma amino acids profiles in children with autism. J Clin Biochem Nutr 51:248–249
Tyzio R, Cossart R, Khalilov I et al (2006) Maternal oxytocin triggers a transient inhibitory switch in GABA signaling in the fetal brain during delivery. Science 314:1788–1792
Tyzio R, Nardou R, Ferrari DC et al (2014) Oxytocin-mediated GABA inhibition during delivery attenuates autism pathogenesis in rodent offspring. Science 343:675–679
van Elst LT, Maier S, Fangmeier T et al (2014) Disturbed cingulate glutamate metabolism in adults with high-functioning autism spectrum disorder: evidence in support of the excitatory/inhibitory imbalance hypothesis. Mol Psychiatry 19:1314–1325
Vizi ES, Kisfali M, Lőrincz T (2013) Role of nonsynaptic GluN2B-containing NMDA receptors in excitotoxicity: evidence that fluoxetine selectively inhibits these receptors and may have neuroprotective effects. Brain Res Bull 93:32–38
Wang C, Shimizu-Okabe C, Watanabe K et al (2002) Developmental changes in KCC1, KCC2, and NKCC1 mRNA expressions in the rat brain. Dev Brain Res 139:59–66
Woods DL, Kovach CR, Raff H et al (2008) Using saliva to measure endogenous cortisol in nursing home residents with advanced dementia. Res Nurs Health 31:283–294
Yamada J, Okabe A, Toyoda H et al (2004) Cl− uptake promoting depolarizing GABA actions in immature rat neocortical neurones is mediated by NKCC1. J Physiol 557:829–841
Yang C-J, Tan H-P, Du Y-J (2014) The developmental disruptions of serotonin signaling may involved in autism during early brain development. Neuroscience 267:1–10
Yap IKS, Angley M, Veselkov KA et al (2010) Urinary metabolic phenotyping differentiates children with autism from their unaffected siblings and age-matched controls. J Proteome Res 9:2996–3004
Young LJ, Barrett CE (2015) Can oxytocin treat autism? Science 347:825–826
Yüksel C, Öngür D (2010) Magnetic resonance spectroscopy studies of glutamate-related abnormalities in mood disorders. Biol Psychiatry 68:785–794
Zhang WQ, Smolik CM, Barba-Escobedo PA et al (2015) Acute dietary tryptophan manipulation differentially alters social behavior, brain serotonin and plasma corticosterone in three inbred mouse strains. Neuropharmacology 90:1–8
Zwaigenbaum L, Bryson SE, Brian J et al (2015) Stability of diagnostic assessment for autism spectrum disorder between 18 and 36 months in a high-risk cohort. Autism Res 9:790–800
Acknowledgments
The authors are grateful for funding from Xiamen Xianyue Hospital (China), University of Alberta (Canada) (Grant No. PSY25), and the VPR Office, University of Alberta (Grant No. PSY92).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Not applicable since this a review of the literature.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human or animals conducted by the authors.
Additional information
Handling Editor: J. D. Wade.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zheng, HF., Wang, WQ., Li, XM. et al. Body fluid levels of neuroactive amino acids in autism spectrum disorders: a review of the literature. Amino Acids 49, 57–65 (2017). https://doi.org/10.1007/s00726-016-2332-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-016-2332-y