Abstract
Purpose
To evaluate the effectiveness of non-steroidal anti-inflammatory drugs (NSAIDs) for the management of neck pain and associated disorders (NAD), whiplash-associated disorders, and non-specific low back pain (LBP) with or without radiculopathy.
Methods
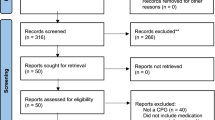
We systematically searched six databases from 2000 to 2014. Random pairs of independent reviewers critically appraised eligible systematic reviews using the Scottish Intercollegiate Guidelines Network criteria. We included systematic reviews with a low risk of bias in our best evidence synthesis.
Results
We screened 706 citations and 14 systematic reviews were eligible for critical appraisal. Eight systematic reviews had a low risk of bias. For recent-onset NAD, evidence suggests that intramuscular NSAIDs lead to similar outcomes as combined manipulation and soft tissue therapy. For NAD (duration not specified), oral NSAIDs may be more effective than placebo. For recent-onset LBP, evidence suggests that: (1) oral NSAIDs lead to similar outcomes to placebo or a muscle relaxant; and (2) oral NSAIDs with bed rest lead to similar outcomes as placebo with bed rest. For persistent LBP, evidence suggests that: (1) oral NSAIDs are more effective than placebo; and (2) oral NSAIDs may be more effective than acetaminophen. For recent-onset LBP with radiculopathy, there is inconsistent evidence on the effectiveness of oral NSAIDs versus placebo. Finally, different oral NSAIDs lead to similar outcomes for neck and LBP with or without radiculopathy.
Conclusions
For NAD, oral NSAIDs may be more effective than placebo. Oral NSAIDs are more effective than placebo for persistent LBP, but not for recent-onset LBP. Different oral NSAIDs lead to similar outcomes for neck pain and LBP.

Similar content being viewed by others
References
Cassidy JD, Carroll LJ, Cote P (1998) The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 23(17):1860–1866 (discussion 7)
Cote P, Cassidy JD, Carroll L (1998) The saskatchewan health and back pain survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 23(15):1689–1698
Hogg-Johnson S, van der Velde G, Carroll LJ et al (2008) The burden and determinants of neck pain in the general population: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine (Phila Pa 1976) 33(4 Suppl):S39–S51
Walker BF (2000) The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord 13(3):205–217
Cote P, Cassidy JD, Carroll L (2001) The treatment of neck and low back pain: who seeks care? Who goes where? Med Care 39(9):956–967
Cypress BK (1983) Characteristics of physician visits for back symptoms: a national perspective. Am J Public Health 73(4):389–395
Carey TS, Evans A, Hadler N, Kalsbeek W, McLaughlin C, Fryer J (1995) Care-seeking among individuals with chronic low back pain. Spine (Phila Pa 1976) 20(3):312–317
Makela M, Heliovaara M, Sievers K, Impivaara O, Knekt P, Aromaa A (1991) Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol 134(11):1356–1367
Carey TS, Evans AT, Hadler NM et al (1996) Acute severe low back pain. A population-based study of prevalence and care-seeking. Spine (Phila Pa 1976) 21(3):339–344
Cassidy JD, Cote P, Carroll LJ, Kristman V (2005) Incidence and course of low back pain episodes in the general population. Spine (Phila Pa 1976) 30(24):2817–2823
Cote P, Baldwin ML, Johnson WG, Frank JW, Butler RJ (2008) Patterns of sick-leave and health outcomes in injured workers with back pain. Eur Spine J 17(4):484–493
Cote P, Cassidy JD, Carroll LJ, Kristman V (2004) The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain 112(3):267–273
Hincapie CA, Cassidy JD, Cote P, Carroll LJ, Guzman J (2010) Whiplash injury is more than neck pain: a population-based study of pain localization after traffic injury. J Occup Environ Med 52(4):434–440
Haldeman S, Dagenais S (2008) A supermarket approach to the evidence-informed management of chronic low back pain. Spine J 8(1):1–7
Hurwitz EL, Carragee EJ, van der Velde G et al (2008) Treatment of neck pain: noninvasive interventions: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine (Phila Pa 1976) 33(4 Suppl):S123–S152
American Academy of Orthopaedic Surgeons (AAOS) (2009) What are NSAIDs? http://orthoinfo.aaos.org/topic.cfm?topic=a00284. Retrieved 1 Nov 2014
Rasu RS, Vouthy K, Crowl AN et al (2014) Cost of pain medication to treat adult patients with nonmalignant chronic pain in the United States. J Manag Care Pharm 20(9):921–928
Pincus T, Newman S (2001) Recall bias, pain, depression and cost in back pain patients. Br J Clin Psychol 40(Pt 2):143–156
Carmona L, Ballina J, Gabriel R, Laffon A (2001) The burden of musculoskeletal diseases in the general population of Spain: results from a national survey. Ann Rheum Dis 60(11):1040–1045
van Tulder MW, Scholten RJ, Koes BW, Deyo RA (2000) Nonsteroidal anti-inflammatory drugs for low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976) 25(19):2501–2513
Peloso P, Gross A, Haines T, Trinh K, Goldsmith CH, Burnie S (2007) Medicinal and injection therapies for mechanical neck disorders. Cochrane Database Syst Rev 3:Cd000319
Kuijpers T, van Middelkoop M, Rubinstein SM et al (2011) A systematic review on the effectiveness of pharmacological interventions for chronic non-specific low-back pain. Eur Spine J 20(1):40–50
Abdel Shaheed C, Maher CG, Williams KA, McLachlan AJ (2014) Interventions available over the counter and advice for acute low back pain: systematic review and meta-analysis. J Pain 15(1):2–15
Roelofs PD, Deyo RA, Koes BW, Scholten RJ, van Tulder MW (2008) Nonsteroidal anti-inflammatory drugs for low back pain: an updated Cochrane review. Spine (Phila Pa 1976) 33(16):1766–1774
Schnitzer TJ, Ferraro A, Hunsche E, Kong SX (2004) A comprehensive review of clinical trials on the efficacy and safety of drugs for the treatment of low back pain. J Pain Symptom Manag 28(1):72–95
Chung JW, Zeng Y, Wong TK (2013) Drug therapy for the treatment of chronic nonspecific low back pain: systematic review and meta-analysis. Pain Physician 16(6):E685–E704
Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW (2007) Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spine J 16(7):881–899
Pinto RZ, Maher CG, Ferreira ML et al (2012) Drugs for relief of pain in patients with sciatica: systematic review and meta-analysis. BMJ 344:e497
Vroomen PC, de Krom MC, Slofstra PD, Knottnerus JA (2000) Conservative treatment of sciatica: a systematic review. J Spinal Disord 13(6):463–469
Moore RA, Barden J (2008) Systematic review of dexketoprofen in acute and chronic pain. BMC Clin Pharmacol 8:11
Klinge SA, Sawyer GA (2013) Effectiveness and safety of topical versus oral nonsteroidal anti-inflammatory drugs: a comprehensive review. Phys Sports Med 41(2):64–74
Guzman J, Hurwitz EL, Carroll LJ et al (2008) A new conceptual model of neck pain: linking onset, course, and care: the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine (Phila Pa 1976) 33(4 Suppl):S14–S23
Spitzer WO, Skovron ML, Salmi LR et al (1995) Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine (Phila Pa 1976) 20(8 Suppl):1s–73s
McGowan J, Sampson M, Lefebvre C (2010) An evidence based checklist for the peer review of electronic search strategies (PRESS EBC). Evid Based Libr Inf Pract 5(1):149–154
EndNote (2013) EndNote X6. http://endnote.com/training/mats/enuserguide/eng/enguide-full.pdf. Retrieved 1 Nov 2014
Harbour R, Miller J (2001) A new system for grading recommendations in evidence based guidelines. BMJ 323(7308):334–336
Shea BJ, Grimshaw JM, Wells GA et al (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 7:10
Slavin RE (1995) Best evidence synthesis: an intelligent alternative to meta-analysis. J Clin Epidemiol 48(1):9–18
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37(5):360–363
Stauffer ME, Taylor SD, Watson DJ, Peloso PM, Morrison A (2011) Definition of nonresponse to analgesic treatment of arthritic pain: an analytical literature review of the smallest detectable difference, the minimal detectable change, and the minimal clinically important difference on the pain visual analog scale. Int J Inflam 2011:231926
Andersson G, Johansson C, Nordlander A, Asmundson GJ (2012) Chronic pain in older adults: a controlled pilot trial of a brief cognitive-behavioural group treatment. Behav Cogn Psychother 40(2):239–244
Carstensen TB, Frostholm L, Oernboel E et al (2012) Are there gender differences in coping with neck pain following acute whiplash trauma? A 12-month follow-up study. Eur J Pain 16(1):49–60
Ostelo RW, Deyo RA, Stratford P et al (2008) Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976) 33(1):90–94
Lauche R, Langhorst J, Dobos GJ, Cramer H (2013) Clinically meaningful differences in pain, disability and quality of life for chronic nonspecific neck pain—a reanalysis of 4 randomized controlled trials of cupping therapy [MCID]. Complement Ther Med 21(4):342–347
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Hahne AJ, Ford JJ, McMeeken JM (2010) Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review. Spine (Phila Pa 1976) 35(11):E488–E504
Keller A, Hayden J, Bombardier C, van Tulder M (2007) Effect sizes of non-surgical treatments of non-specific low-back pain. Eur Spine J 16(11):1776–1788
Yamamoto M, Sugano T, Kashiwazaki S, Kageyama T, Mizushima Y, Kameyama M (1983) Double-blind comparison of Piroxicam and Indomethacin in the treatment of cervicobrachial syndrome and periarthritis scapulohumeralis (stiff shoulder). Eur J Rheumatol Inflamm 6(3):266–273
McReynolds TM, Sheridan BJ (2005) Intramuscular ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc 105(2):57–68
Bakshi R, Thumb N, Broll H (2008) Treatment of acute lumbosacral back pain with Diclofenac resinate: results of a double-blind comparative trial versus Piroxicam. Drug Invest 8:288–293
Goldie I (1968) A clinical trial with Indomethacin (indomee(R)) in low back pain and sciatica. Acta Orthop Scand 39(1):117–128
Orava S (1986) Medical treatment of acute low back pain. Diflunisal compared with Indomethacin in acute lumbago. Int J Clin Pharmacol Res 6(1):45–51
Pohjolainen T, Jekunen A, Autio L, Vuorela H (2000) Treatment of acute low back pain with the COX-2-selective anti-inflammatory drug nimesulide: results of a randomized, double-blind comparative trial versus ibuprofen. Spine (Phila Pa 1976) 25(12):1579–1585
Schattenkirchner M, Milachowski KA (2003) A double-blind, multicentre, randomised clinical trial comparing the efficacy and tolerability of Aceclofenac with Diclofenac resinate in patients with acute low back pain. Clin Rheumatol 22(2):127–135
Szpalski M, Hayez JP (1994) Objective functional assessment of the efficacy of tenoxicam in the treatment of acute low back pain. A double-blind placebo-controlled study. Br J Rheumatol 33(1):74–78
Videman T, Heikkila J, Partnaen T (1984) Double-blind parallel study of meptazinol versus diflunisal in the treatment of lumbago. Curr Med Res Opin 9:246–252
Ximenes A, Robles M, Sands G, Vinueza R (2007) Valdecoxib is as efficacious as Diclofenac in the treatment of acute low back pain. Clin J Pain 23(3):244–250
Yakhno N, Guekht A, Skoromets A et al (2006) Analgesic efficacy and safety of lornoxicam quick-release formulation compared with Diclofenac potassium: randomised, double-blind trial in acute low back pain. Clin Drug Investig 26(5):267–277
Berry H, Bloom B, Hamilton EB, Swinson DR (1982) Naproxen sodium, diflunisal, and placebo in the treatment of chronic back pain. Ann Rheum Dis 41(2):129–132
Birbara CA, Puopolo AD, Munoz DR et al (2003) Treatment of chronic low back pain with Etoricoxib, a new cyclo-oxygenase-2 selective inhibitor: improvement in pain and disability—a randomized, placebo-controlled, 3-month trial. J Pain 4(6):307–315
Chrubasik S, Model A, Black A, Pollak S (2003) A randomized double-blind pilot study comparing Doloteffin and Vioxx in the treatment of low back pain. Rheumatology (Oxford) 42(1):141–148
Coats TL, Borenstein DG, Nangia NK, Brown MT (2004) Effects of Valdecoxib in the treatment of chronic low back pain: results of a randomized, placebo-controlled trial. Clin Ther 26(8):1249–1260
Hickey RF (1982) Chronic low back pain: a comparison of diflunisal with paracetamol. N Z Med J 95(707):312–314
Matsumo S, Kaneda K, Nohara Y (1991) Clinical evaluation of Ketoprofen (Orudis) in lumbago: a double blind comparison with Diclofenac sodium. Br J Clin Pract 35:266
Zerbini C, Ozturk ZE, Grifka J et al (2005) Efficacy of Etoricoxib 60 mg/day and Diclofenac 150 mg/day in reduction of pain and disability in patients with chronic low back pain: results of a 4-week, multinational, randomized, double-blind study. Curr Med Res Opin 21(12):2037–2049
Pallay R, Seger W, Adler J (2007) Etoricoxib reduced pain and disability and improved quality of life in patients with chronic low back pain: a 3 month, randomized, controlled trial. Scand J Rheumatol 33:257–266
Jaffe G (1974) A double-blind, between-patient comparison of alclofenac (‘Prinalgin’) and Indomethacin in the treatment of low back pain and sciatica. Curr Med Res Opin 2(7):424–429
Babej-Dolle R, Freytag S, Eckmeyer J et al (1994) Parenteral Dipyrone versus Diclofenac and placebo in patients with acute lumbago or sciatic pain: randomized observer-blind multicenter study. Int J Clin Pharmacol Ther 32(4):204–209
Blazek M, Keszthelyi B, Varhelyi M, Korosi O (1986) Comparative study of Biarison and Voltaren in acute lumbar pain and lumbo-ischialgia. Ther Hung 34(3):163–166
Herrmann W, Geertsen M (2009) Efficacy and safety of lornoxicam compared with placebo and Diclofenac in acute sciatica/lumbo-sciatica: an analysis from a randomised, double-blind, multicentre, parallel-group study. Int J Clin Pract 63:1613–1621
Dreisser RL, Le Parc JM, Velicitat P, Lleu PL (2001) Oral meloxicam is effective in acute sciatica: two randomised, double-blind trials versus placebo or Diclofenac. Inflamm Res 50(1):S17–S23
Weber H, Aasand G (1980) The effect of Phenylbutazone on patients with acute lumbago-sciatica. A double blind trial. J Oslo City Hosp 30(5):69–72
Weber H, Holme I, Amlie E (1993) The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of Piroxicam. Spine (Phila Pa 1976) 18(11):1433–1438
Weber H (1983) Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine 8:131–140
Waddell G, Feder G, Lewis M (1997) Systematic reviews of bed rest and advice to stay active for acute low back pain. Br J Gen Pract 47(423):647–652
Huang HY, Andrews E, Jones J, Skovron ML, Tilson H (2011) Pitfalls in meta-analyses on adverse events reported from clinical trials. Pharmacoepidemiol Drug Saf 20(10):1014–1020
Juni P, Holenstein F, Sterne J, Bartlett C, Egger M (2002) Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol 31(1):115–123
Moher D, Fortin P, Jadad AR et al (1996) Completeness of reporting of trials published in languages other than English: implications for conduct and reporting of systematic reviews. Lancet 347(8998):363–366
Moher D, Pham B, Lawson ML, Klassen TP (2003) The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technol Assess 7(41):1–90
Morrison A, Polisena J, Husereau D et al (2012) The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care 28(2):138–144
Sutton AJ, Duval SJ, Tweedie RL, Abrams KR, Jones DR (2000) Empirical assessment of effect of publication bias on meta-analyses. BMJ 320(7249):1574–1577
Acknowledgments
The authors acknowledge the invaluable contributions to this review from: Angela Verven, J. David Cassidy, Douglas Gross, Gail Lindsay, John Stapleton, Leslie Verville, Margareta Nordin, Michel Lacerte, Mike Paulden, Murray Krahn, Patrick Loisel, and Roger Salhany. The authors also thank Trish Johns-Wilson at the University of Ontario Institute of Technology for her review of the search strategy. This study was funded by the Ontario Ministry of Finance and the Financial Services Commission of Ontario (RFP No.: OSS_00267175). The funding agency was not involved in the collection of data, data analysis, interpretation of data, or drafting of the manuscript. The research was undertaken, in part, thanks to funding from the Canada Research Chairs program to Dr. Pierre Côté, Canada Research Chair in Disability Prevention and Rehabilitation at the University of Ontario Institute of Technology.
Conflict of interest
Dr. Pierre Côté has received a grant from the Ontario Government, Ministry of Finance; a grant from Aviva Canada; and funding from the Canada Research Chairs program. Dr. Robert Brison and Dr. Silvano Mior have received an honorarium as a guideline expert panel member. For the remaining authors, no conflicts of interest were declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Systematic Review Registration Number: CRD42014009782.
Appendix I: MEDLINE (Ovid Technologies Inc.) search strategy for whiplash-associated disorders, neck pain and associated disorders, non-specific low back pain, and non-steroidal anti-inflammatory drugs (NSAIDs)
Appendix I: MEDLINE (Ovid Technologies Inc.) search strategy for whiplash-associated disorders, neck pain and associated disorders, non-specific low back pain, and non-steroidal anti-inflammatory drugs (NSAIDs)
-
1.
Whiplash Injuries/
-
2.
Neck Injuries/
-
3.
Neck Pain/
-
4.
Neck Muscles/in [Injuries]
-
5.
exp Cervical Vertebrae/in [Injuries]
-
6.
Radiculopathy/
-
7.
exp Brachial Plexus Neuropathies/
-
8.
Torticollis/
-
9.
whiplash.ab,ti.
-
10.
“neck injur*”.ab,ti.
-
11.
“neck pain*”.ab,ti.
-
12.
“cervical pain*”.ab,ti.
-
13.
“neck ache*”.ab,ti.
-
14.
“neckache*”.ab,ti.
-
15.
“cervicalgia*”.ab,ti.
-
16.
“cervicodynia*”.ab,ti.
-
17.
“radiculopath*”.ab,ti.
-
18.
“brachial plexus neuropath*”.ab,ti.
-
19.
torticollis.ab,ti.
-
20.
or/1-19
-
21.
exp Back/
-
22.
exp Back Injuries/
-
23.
exp Back Pain/
-
24.
Coccyx/in [Injuries]
-
25.
Intervertebral Disc Degeneration/
-
26.
Intervertebral Disc Displacement/
-
27.
Lumbar Vertebrae/in [Injuries]
-
28.
exp Lumbosacral Plexus/
-
29.
Lumbosacral Region/in [Injuries]
-
30.
Osteoarthritis, Spine/
-
31.
Piriformis Muscle Syndrome/
-
32.
Polyradiculopathy/
-
33.
Sacrococcygeal Region/
-
34.
Sacroiliac Joint/
-
35.
Sacrum/
-
36.
Sciatica/
-
37.
Spinal Diseases/
-
38.
Spinal Stenosis/
-
39.
(avulsed lumbar adj3 (disc* or disk*)).ab,ti.
-
40.
(back adj3 (ache* or injur* or pain*)).ab,ti.
-
41.
(backache* adj3 (injur* or pain*)).ab,ti.
-
42.
(back pain or back-pain).ab,ti.
-
43.
coccydynia.ab,ti.
-
44.
coccyx.ab,ti.
-
45.
dorsalgia.ab,ti.
-
46.
(lumbar disc* adj3 (extruded or degenerat* or herniat* or prolapse* or sequestered or slipped)).ab,ti.
-
47.
(lumbar disk* adj3 (extruded or degenerat* or herniat* or prolapse* or sequestered or slipped)).ab,ti.
-
48.
“low* back pain”.ab,ti.
-
49.
“low*-back-pain*”.ab,ti.
-
50.
(lumbar adj3 (pain or facet or nerve root* or osteoarthritis or radicul* or spinal stenosis or spondylo* or zygapophys*)).ab,ti.
-
51.
“lumbarsacr*”.ab,ti.
-
52.
lumboischialgia.ab,ti.
-
53.
“lumbosacr*”.ab,ti.
-
54.
“Piriformis syndrome*”.ab,ti.
-
55.
radiculalgia.ab,ti.
-
56.
(sacral adj2 pain*).ab,ti.
-
57.
(sacrococcygeal adj2 pain*).ab,ti.
-
58.
(sacroiliac or sacro-iliac).ab,ti.
-
59.
“sciatic*”.ab,ti.
-
60.
(SI adj joint).ab,ti.
-
61.
(spinal adj stenos?s).ab,ti.
-
62.
spondylosis.ab,ti.
-
63.
“tailbone adj3 pain*”.ab,ti.
-
64.
“vertebrogenic adj3 pain*”.ab,ti.
-
65.
or/21-64
-
66.
20 or 65
-
67.
exp Anti-Inflammatory Agents, Non-Steroidal/
-
68.
alclofenac.ab,hw,ti,nm.
-
69.
Aspirin.ab,hw,ti,nm.
-
70.
Cyclooxygenase 2.ab,hw,ti,nm.
-
71.
benoxaprofen.ab,hw,ti,nm.
-
72.
Benzydamine.ab,hw,ti,nm.
-
73.
Bufexamac.ab,hw,ti,nm.
-
74.
celecoxib.ab,hw,ti,nm.
-
75.
dexibuprofen.ab,hw,ti,nm.
-
76.
dexketoprofen trometamol.ab,hw,ti,nm.
-
77.
Diclofenac.ab,hw,ti,nm.
-
78.
Dipyrone.ab,hw,ti,nm.
-
79.
Diflunisal.ab,hw,ti,nm.
-
80.
droxicam.ab,hw,ti,nm.
-
81.
Etodolac.ab,hw,ti,nm.
-
82.
etofenamate.ab,hw,ti,nm.
-
83.
etoricoxib.ab,hw,ti,nm.
-
84.
Fenoprofen.ab,hw,ti,nm.
-
85.
firocoxib.ab,hw,ti,nm.
-
86.
Flufenamic Acid.ab,hw,ti,nm.
-
87.
Flurbiprofen.ab,hw,ti,nm.
-
88.
Ibuprofen.ab,hw,ti,nm.
-
89.
Indomethacin.ab,hw,ti,nm.
-
90.
isoxicam.ab,hw,ti,nm.
-
91.
Ketoprofen.ab,hw,ti,nm.
-
92.
Ketorola.ab,hw,ti,nm.
-
93.
loxoprofen.ab,hw,ti,nm.
-
94.
lumiracoxib.ab,hw,ti,nm.
-
95.
lysine clonixinate.ab,hw,ti,nm.
-
96.
Magnesium Salicylate.ab,hw,ti,nm.
-
97.
Meclofenamic Acid.ab,hw,ti,nm.
-
98.
Mefenamic Acid.ab,hw,ti,nm.
-
99.
meloxicam.ab,hw,ti,nm.
-
100.
morniflumate.ab,hw,ti,nm.
-
101.
Naproxen.ab,hw,ti,nm.
-
102.
Niflumic Acid.ab,hw,ti,nm.
-
103.
Oxyphenbutazone.ab,hw,ti,nm.
-
104.
piketoprofen.ab,hw,ti,nm.
-
105.
Piroxicam.ab,hw,ti,nm.
-
106.
salicylsalicylic acid.ab,hw,ti,nm.
-
107.
Sulindac.ab,hw,ti,nm.
-
108.
tenoxicam.ab,hw,ti,nm.
-
109.
Tolmetin.ab,hw,ti,nm.
-
110.
valdecoxib.ab,hw,ti,nm.
-
111.
or/67-110
-
112.
Actron.ti,ab.
-
113.
Acular.ti,ab.
-
114.
Advil.ti,ab.
-
115.
Afrolate.ti,ab.
-
116.
Aleve.ti,ab.
-
117.
Algesalona.ti,ab.
-
118.
Amigesic.ti,ab.
-
119.
Anacin.ti,ab.
-
120.
Anaflex 750.ti,ab.
-
121.
Anaprox.ti,ab.
-
122.
Ansaid.ti,ab.
-
123.
Arthitab.ti,ab.
-
124.
Arthropam.ti,ab.
-
125.
Arthrotec.ti,ab.
-
126.
Ascriptin.ti,ab.
-
127.
Bayer.ti,ab.
-
128.
Bayro.ti,ab.
-
129.
Bextra.ti,ab.
-
130.
Bufferin.ti,ab.
-
131.
Cambia.ti,ab.
-
132.
Cataflam.ti,ab.
-
133.
celebrex.ti,ab.
-
134.
Clinoril.ti,ab.
-
135.
Cuprofen.ti,ab.
-
136.
Daypro.ti,ab.
-
137.
Diflamil.ti,ab.
-
138.
Dignodolin.ti,ab.
-
139.
Disalcid.ti,ab.
-
140.
Doan’s Pills.ti,ab.
-
141.
Dolinac.ti,ab.
-
142.
Dolobid.ti,ab.
-
143.
Duexis.ti,ab.
-
144.
Ecotrin.ti,ab.
-
145.
Feldene.ti,ab.
-
146.
Fenbid.ti,ab.
-
147.
Fenomel.ti,ab.
-
148.
Fentiazac.ti,ab.
-
149.
Flector.ti,ab.
-
150.
Flexidol.ti,ab.
-
151.
Flexium.ti,ab.
-
152.
Flogoprofen.ti,ab.
-
153.
Flurwood.ti,ab.
-
154.
Froben.ti,ab.
-
155.
Hifenac.ti,ab.
-
156.
Ibuprofen.ti,ab.
-
157.
Indocin.ti,ab.
-
158.
Indomethegan.ti,ab.
-
159.
Ketofen.ti,ab.
-
160.
Lodine.ti,ab.
-
161.
Magan.ti,ab.
-
162.
Marthritic.ti,ab.
-
163.
Meclomen.ti,ab.
-
164.
Mobic.ti,ab.
-
165.
Mobidin.ti,ab.
-
166.
Mobogesic.ti,ab.
-
167.
Mono-Gesic.ti,ab.
-
168.
Motrin.ti,ab.
-
169.
Nalfon.ti,ab.
-
170.
Naprelan.ti,ab.
-
171.
Naprosyn.ti,ab.
-
172.
Niflatol.ti,ab.
-
173.
Niflugel.ti,ab.
-
174.
Nifluril.ti,ab.
-
175.
Nixyn.ti,ab.
-
176.
Nuprin.ti,ab.
-
177.
Oftalar.ti,ab.
-
178.
Orudis.ti,ab.
-
179.
Oruvail.ti,ab.
-
180.
Paraderm.ti,ab.
-
181.
Parfenac.ti,ab.
-
182.
Pennsaid.ti,ab.
-
183.
Ponstel.ti,ab.
-
184.
Pranox.ti,ab.
-
185.
Relafen.ti,ab.
-
186.
Salflex.ti,ab.
-
187.
Salsitab.ti,ab.
-
188.
Sastridex.ti,ab.
-
189.
Solaraze.ti,ab.
-
190.
Solpaflex.ti,ab.
-
191.
Sprix.ti,ab.
-
192.
Suxibuzone.ti,ab.
-
193.
Tiloket.ti,ab.
-
194.
Tolectin.ti,ab.
-
195.
Toradol.ti,ab.
-
196.
Transact Lat.ti,ab.
-
197.
Traumalix.ti,ab.
-
198.
Traumon.ti,ab.
-
199.
Traxam.ti,ab.
-
200.
Trilisate.ti,ab.
-
201.
Triparsean.ti,ab.
-
202.
Triscosal.ti,ab.
-
203.
Vimovo.ti,ab.
-
204.
Vioxx.ti,ab.
-
205.
voltaren*.ti,ab.
-
206.
Voltarol.ti,ab.
-
207.
or/112-206
-
208.
111 or 207
-
209.
acetylsalicyl*.ti,ab.
-
210.
COX 1.ti,ab.
-
211.
COX 2.ti,ab.
-
212.
COX I.ti,ab.
-
213.
COX II.ti,ab.
-
214.
COX-1.ti,ab.
-
215.
COX-2.ti,ab.
-
216.
COX-I.ti,ab.
-
217.
COX-II.ti,ab.
-
218.
cyclooxygenase.ti,ab.
-
219.
cyclo-oxygenase.ti,ab.
-
220.
non-steroidal anti-inflammatory agent*.ti,ab.
-
221.
nonsteroidal anti-inflammatory agent*.ti,ab.
-
222.
NSAIA*.ti,ab.
-
223.
NSAID*.ti,ab.
-
224.
NSAIM*.ti,ab.
-
225.
salicylate*.ti,ab.
-
226.
or/209-225
-
227.
208 or 226
-
228.
66 and 227
-
229.
Meta-Analysis as Topic/
-
230.
Meta-Analysis.pt.
-
231.
(meta adj analy*).ti,ab.
-
232.
metaanaly*.ti,ab.
-
233.
(systematic adj3 (review* or overview*)).ti,ab.
-
234.
(methodologic* adj3 (review* or overview*)).ti,ab.
-
235.
(integrative adj3 (review* or overview*)).ti,ab.
-
236.
(collaborative adj3 (review* or overview*)).ti,ab.
-
237.
exp Review Literature as Topic/
-
238.
medline.ab.
-
239.
pubmed.ab.
-
240.
cochrane.ab.
-
241.
embase.ab.
-
242.
(psychlit or psyclit).ab.
-
243.
(psychinfo or psycinfo).ab.
-
244.
(cinahl or cinhal).ab.
-
245.
science citation index.ab.
-
246.
(reference adj list*).ab.
-
247.
bibliograph*.ab.
-
248.
(hand-search* or handsearch).ab.
-
249.
manual search*.ab.
-
250.
or/229-249
-
251.
Review/
-
252.
(selection adj3 criteria).ab.
-
253.
(data adj3 (extraction or synthes*)).ab.
-
254.
251 and (252 or 253)
-
255.
250 or 254
-
256.
228 and 255
-
257.
limit 256 to (english language and humans and yr = “2000 -Current”)
Rights and permissions
About this article
Cite this article
Wong, J.J., Côté, P., Ameis, A. et al. Are non-steroidal anti-inflammatory drugs effective for the management of neck pain and associated disorders, whiplash-associated disorders, or non-specific low back pain? A systematic review of systematic reviews by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur Spine J 25, 34–61 (2016). https://doi.org/10.1007/s00586-015-3891-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3891-4