Abstract
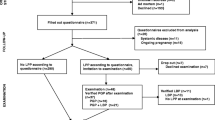
Pelvic girdle pain (PGP) has a high incidence during pregnancy and in some women pain will persist for years. Most studies have used pain as the outcome measure, and little attention is given to functioning or disability. A better understanding of prognostic factors for recovery seems important for clinical care and treatment. The aim of the present paper was to identify prognostic factors for recovery from postpartum PGP and disability, and to determine the impacts of prognostic factors when pain intensity and disability are used as outcome measures. Seventy-eight women with diagnosed PGP were included 6–16 weeks postpartum. Possible prognostic factors were obtained through clinical tests and questionnaires at baseline. The clinical tests were posterior pelvic pain provocation (P4) test, active straight leg raise (ASLR) test and pain provocation of long dorsal sacroiliac ligament (LDL). One year postpartum outcome measures were obtained by Oswestry disability index (ODI ver 2.0) and worst evening pain (VAS 0–100). Multiple linear regression and logistic regression analyses were used to identify significant prognostic factors. At baseline 60% believed they would recover and 40% were uncertain or believed they would not recover. Fifty per cent had a history of low back pain (LBP), and 20% had high emotional distress (HSCL25-item ≥1.75). About 75% had positive LDL and P4 at both sides and 24% had pain located to all three pelvic joints. Forty per cent had ASLR scores of at least 4 (sum score range 0–10). Multivariate analyses showed consistently that ASLR and belief in improvement were statistical significant predictors for both disability and pain as outcome measures. ASLR score <4 predicted 10 points lower ODI and 19 points lower evening pain compared with having ASLR score of at least 4. Pain location was a statistical significant predictor in only one analysis. History of LBP or high psychological distress was not prognostic for recovery. ASLR test and belief in improvement are predictors of clinical significance in women having PGP postpartum.


Similar content being viewed by others
References
Albert H, Godskesen M, Westergaard J (2001) Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet Gynecol Scand 80:505–510
Albert HB, Godskesen M, Korsholm L, Westergaard JG (2006) Risk factors in developing pregnancy-related pelvic girdle pain. Acta Obstet Gynecol Scand 85:539–544
Albert HB, Godskesen M, Westergaard JG (2002) Incidence of four syndromes of pregnancy-related pelvic joint pain. Spine 27:2831–2834
Bandura A, Locke EA (2003) Negative self-efficacy and goal effects revisited. J Appl Psychol 88:87–99
Bastiaenen CH, De Bie RA, Wolters PM, Vlaeyen JW, Leffers P, Stelma F, Bastiaanssen JM, Essed GG, van den Brandt PA (2006) Effectiveness of a tailor-made intervention for pregnancy-related pelvic girdle and/or low back pain after delivery: short-term results of a randomized clinical trial [ISRCTN08477490]. BMC Musculoskelet Disord 7:19
Breen TW, Ransil BJ, Groves PA, Oriol NE (1994) Factors associated with back pain after childbirth. Anesthesiology 81:29–34
Buchner M, Neubauer E, Zahlten-Hinguranage A, Schiltenwolf M (2007) Age as a predicting factor in the therapy outcome of multidisciplinary treatment of patients with chronic low back pain—a prospective longitudinal clinical study in 405 patients. Clin Rheumatol 26:385–392
Cedraschi C, Allaz AF (2005) How to identify patients with a poor prognosis in daily clinical practice. Best Pract Res Clin Rheumatol 19:577–591
Coste J, Delecoeuillerie G, de Cohen LA, Le Parc JM, Paolaggi JB (1994) Clinical course and prognostic factors in acute low back pain: an inception cohort study in primary care practice. Br Med J 308:577–580
Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine 25:2940–2952
Grotle M, Brox JI, Veierod MB, Glomsrod B, Lonn JH, Vollestad NK (2005) Clinical course and prognostic factors in acute low back pain: patients consulting primary care for the first time. Spine 30:976–982
Grotle M, Brox JI, Vollestad NK (2004) Concurrent comparison of responsiveness in pain and functional status measurements used for patients with low back pain. Spine 29:E492–E501
Grotle M, Brox JI, Vollestad NK (2005) Functional status and disability questionnaires: what do they assess? A systematic review of back-specific outcome questionnaires. Spine 30:130–140
Gutke A, Ostgaard HC, Oberg B (2008) Predicting persistent pregnancy-related low back pain. Spine 33:E386–E393
Hicks GE, Fritz JM, Delitto A, McGill SM (2005) Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil 86:1753–1762
Mens JM, Snijders CJ, Stam HJ (2000) Diagonal trunk muscle exercises in peripartum pelvic pain: a randomized clinical trial. Phys Ther 80:1164–1173
Mens JM, Vleeming A, Snijders CJ, Koes BW, Stam HJ (2001) Reliability and validity of the active straight leg raise test in posterior pelvic pain since pregnancy. Spine 26:1167–1171
Mens JM, Vleeming A, Snijders CJ, Koes BW, Stam HJ (2002) Validity of the active straight leg raise test for measuring disease severity in patients with posterior pelvic pain after pregnancy. Spine 27:196–200
Mens JM, Vleeming A, Snijders CJ, Stam HJ, Ginai AZ (1999) The active straight leg raising test and mobility of the pelvic joints. Eur Spine J 8:468–473
Mogren IM (2006) BMI, pain and hyper-mobility are determinants of long-term outcome for women with low back pain and pelvic pain during pregnancy. Eur Spine J 15:1093–1102
Ostgaard HC, Andersson GB (1992) Postpartum low-back pain. Spine 17:53–55
Ostgaard HC, Andersson GB, Karlsson K (1991) Prevalence of back pain in pregnancy. Spine 16:549–552
Ostgaard HC, Roos-Hansson E, Zetherstrom G (1996) Regression of back and posterior pelvic pain after pregnancy. Spine 21:2777–2780
Ostgaard HC, Zetherstrom G, Roos-Hansson E (1994) The posterior pelvic pain provocation test in pregnant women. Eur Spine J 3:258–260
Robinson HS, Eskild A, Heiberg E, Eberhard-Gran M (2006) Pelvic girdle pain in pregnancy: the impact on function. Acta Obstet Gynecol Scand 85:160–164
Rost CC, Jacqueline J, Kaiser A, Verhagen AP, Koes BW (2006) Prognosis of women with pelvic pain during pregnancy: a long-term follow-up study. Acta Obstet Gynecol Scand 85:771–777
Stuge B, Laerum E, Kirkesola G, Vollestad N (2004) The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a randomized controlled trial. Spine 29:351–359
Thomas E, Silman AJ, Croft PR, Papageorgiou AC, Jayson MI, Macfarlane GJ (1999) Predicting who develops chronic low back pain in primary care: a prospective study. Br Med J 318:1662–1667
To WW, Wong MW (2003) Factors associated with back pain symptoms in pregnancy and the persistence of pain 2 years after pregnancy. Acta Obstet Gynecol Scand 82:1086–1091
Turgut F, Turgut M, Cetinsahin M (1998) A prospective study of persistent back pain after pregnancy. Eur J Obstet Gynecol Reprod Biol 80:45–48
Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B (2008) European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 17:794–819
Vleeming A, de Vries HJ, Mens JM, van Wingerden JP (2002) Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta Obstet Gynecol Scand 81:430–436
Wu WH, Meijer OG, Uegaki K, Mens JMA, van Dieën JH, Wuisman PIJM, Ostgaard HC (2004) Pregnancy-related pelvic girdle pain (PPP), I: terminology, clinical presentation, and prevalence. Eur Spine J 13:575–589
Acknowledgments
We thank the Norwegian Foundation for Health and Rehabilitation and the Norwegian Women’s Public Health Association for financial support to the study. The study complies with the current laws and requirements of medical research in Norway and has been approved by the regional ethics committee.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vøllestad, N.K., Stuge, B. Prognostic factors for recovery from postpartum pelvic girdle pain. Eur Spine J 18, 718–726 (2009). https://doi.org/10.1007/s00586-009-0911-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-0911-2