Abstract
Purpose
Our aims were to evaluate the prevalence of preoperative acute sleep disruption in the hospital and to assess perioperative sleep quality and the effects of acute sleep disruption on postoperative functional recovery in a surgical setting.
Methods
This prospective observational study included 24 patients aged ≥ 20 years who underwent video-assisted thoracoscopic surgical lobectomy for lung cancer under general anesthesia at a tertiary hospital in Japan between October 2016 and May 2017. Actigraphy was performed for 7 days in the hospital, including the night before surgery. We defined acute sleep disturbance as less than 85% preoperative sleep efficiency and analyzed its effect on postoperative functional disability using the 12-item World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) and Mann–Whitney U testing. The perioperative change in sleep efficiency was compared using a Dunn analysis. A high score on the WHODAS 2.0 is indicative of impaired function.
Results
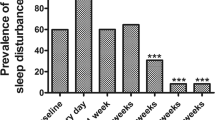
Nineteen (79.1%) patients had low sleep efficiency in the hospital prior to surgery. Three months after surgery, the 12-item WHODAS 2.0 score was higher in patients with acute sleep disturbance than in those without it (38.8 versus 33.3, p = 0.02, effect size 0.5). Sleep efficiency decreased significantly on the 5th postoperative day in patients with acute sleep disturbance.
Conclusions
Our results showed a high prevalence of acute sleep disturbance. Patients with acute sleep disruption had low postoperative sleep efficiency and impaired functional ability three months after surgery.


Similar content being viewed by others
References
Kain ZN, Caldwell-Andrews AA. Sleeping characteristics of adults undergoing outpatient elective surgery: a cohort study. J Clin Anesth. 2003;15:505–9.
Fielden JM, Gander PH, Horne JG, Lewer BM, Green RM, Devane PA. An assessment of sleep disturbance in patients before and after total hip arthroplasty. J Arthroplasty. 2003;18:371–6.
Moore JT, Kelz MB. Opiates, sleep, and pain. The adenosinergic link. Anesthesiology. 2009;111:1175–6.
Leung JM, Sands LP, Newman S, Meckler G, Xie Y, Gay C, Lee K. Preoperative sleep disruption and postoperative delirium. J Clin Sleep Med. 2015;11:907–13.
Aspinen S, Kärkkäinen J, Harju J, Juvonen P, Kokki H, Eskelinen M. Improvement in the quality of life following cholecystectomy: a randomized multicenter study of health status (RAND-36) in patients with laparoscopic cholecystectomy versus minilaparotomy cholecystectomy. Qual Life Res. 2017;26:665–71.
Shulman MA, Myles PS, Chan MT, McIlroy DR, Wallace S, Ponsford J. Measurement of disability-free survival after surgery. Anesthesiology. 2015;122:524–36.
Myles PS, Viira D, Hunt JO. Quality of life at three years after cardiac surgery: relationship with preoperative status and quality of recovery. Anaesth Intensive Care. 2006;34:176–83.
Ustün TB, Chatterji S, Kostanjsek N, Rehm J, Kennedy C, Epping-Jordan J, Saxena S, von Korff M, Pull C, WHO/NIH Joint Project. Developing the World Health Organization Disability Assessment Schedule 2.0. Bull World Health Organ. 2010; 88:815–23.
Ida M, Naito Y, Tanaka Y, Matsunari Y, Inoue S, Kawaguchi M. Feasibility, reliability, and validity of the Japanese version of the 12-item World Health Organization Disability Assessment Schedule-2 in preoperative patients. J Anesth. 2017;31:539–44.
Buysse DJ, Reynolds CF 3rd, Monk TH, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–13.
Palesh O, Aldridge-Gerry A, Zeitzer JM, Koopman C, Neri E, Giese-Davis J, Jo B, Kraemer H, Nouriani B, Spiegel D. Actigraphy-measured sleep disruption as a predictor of survival among women with advanced breast cancer. Sleep. 2014;37:837–42.
Shinkoda H, Matsumoto K, Hamasaki J, Seo YJ, Park YM, Park KP. Evaluation of human activities and sleep-wake identification using wrist actigraphy. Psychiatry Clin Neurosci. 1998;52:157–9.
Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). Geneva: World Health Organization; 2010. https://apps.who.int/iris/bitstream/10665/43974/1/9789241547598_eng.pdf. Accessed 20 Jan 2019.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Sullivan MJ, Bishop SR, Pivik J. Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995; 7:524–32.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85:1001–5.
Ogawa S. Development of new screening questionnaire to identify neuropathic components in Japanese patients with chronic pain. Pain Clin. 2010;31:1187–94.
Kazis LE, Anderson JJ, Meenan RF. Effect sizes for interpreting changes in health status. Med Care. 1989;27:S178–89.
Todd OM, Gelrich L, MacLullich AM, Driessen M, Thomas C, Kreisel SH. Sleep disruption at home as an independent risk factor for postoperative delirium. J Am Geriatr Soc. 2017;65:949–57.
Park MJ, Yoo JH, Cho BW, Kim KT, Jeong WC, Ha M. Noise in hospital rooms and sleep disturbance in hospitalized medical patients. Environ Health Toxicol. 2014;29:e2014006.
Krenk L, Jennum P, Kehlet H. Sleep disturbances after fast-track hip and knee arthroplasty. Br J Anaesth. 2012;109:769–75.
Liao WC, Huang CY, Huang TY, Hwang SL. A systematic review of sleep patterns and factors that disturb sleep after heart surgery. J Nurs Res. 2011;19:275–88.
Onodera H, Ida M, Yamauchi M, Kawaguchi M. Gynecological surgery and anesthesia might affect postoperative sleep quality. J Clin Anesth. 2017;41:1373–8.
Stenholm S, Kronholm E, Sainio P, Borodulin K, Era P, Fogelholm M, Partonen T, Porkka-Heiskanen T, Koskinen S. Sleep-related factors and mobility in older men and women. J Gerontol Ser A Biol Sci Med Sci. 2010;65:649–57.
Goldman SE, Stone KL, Ancoli-Israel S, Blackwell T, Ewing SK, Boudreau R, Cauley JA, Hall M, Matthews KA, Newman AB. Poor sleep is associated with poorer physical performance and greater functional limitations in older women. Sleep. 2007;30:1317–24.
Blackwell T, Yaffe K, Ancoli-Israel S, Schneider JL, Cauley JA, Hillier TA, Fink HA, Stone KL, Study of Osteoporotic Fractures Group. Poor sleep is associated with impaired cognitive function in older women: the study of osteoporotic fractures. J Gerontol Ser A Biol Sci Med Sci. 2006;61:405–10.
Cohen-Zion M, Stepnowsky C, Shochat T, Kripke DF, Ancoli-Israel S. Changes in cognitive function associated with sleep disordered breathing in older people. J Am Geriatr Soc. 2001;49:1622–7.
Ingiosi AM, Opp MR, Krueger JM. Sleep and immune function: glial contributions and consequences of aging. Curr Opin Neurobiol. 2013;23:806–11.
Westhoff D, Witlox J, Koenderman L, Kalisvaart KJ, de Jonghe JF, van Stijn MF, Houdijk AP, Hoogland IC, Maclullich AM, van Westerloo DJ, van de Beek D, Eikelenboom P, van Gool WA. Preoperative cerebrospinal fluid cytokine levels and the risk of postoperative delirium in elderly hip fracture patients. J Neuroinflamm. 2013;10:122.
Goldman SE, Ancoli-Israel S, Boudreau R, Cauley JA, Hall M, Stone KL, Rubin SM, Satterfield S, Simonsick EM, Newman AB, Health, Aging and Body Composition Study. Sleep problems and associated daytime fatigue in community-dwelling older individuals. J Gerontol Ser A Biol Sci Med Sci. 2008;3:1069–75.
Abola RE, Bennett-Guerrero E, Kent ML, Feldman LS, Fiore JF Jr, Shaw AD, Thacker JKM, Gan TJ, Miller TE, Hedrick TL, McEvoy MD, Mythen MG, Bergamaschi R, Gupta R, Holubar SD, Senagore AJ, Wischmeyer PE, Carli F, Evans DC, Guilbert S, Kozar R, Pryor A, Thiele RH, Everett S, Grocott M, Perioperative Quality Initiative (POQI) 2 Workgroup. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on patient-reported outcomes in an enhanced recovery pathway. Anesth Analg. 2018;126:1874–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Ida, M., Onodera, H., Yamauchi, M. et al. Preoperative sleep disruption and postoperative functional disability in lung surgery patients: a prospective observational study. J Anesth 33, 501–508 (2019). https://doi.org/10.1007/s00540-019-02656-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02656-y