Abstract
Purpose
Pain and fatigue are common symptoms in oncology patients. In a sample of oncology outpatients receiving chemotherapy (n = 1342), the study purposes were to identify subgroups of patients with distinct worst pain and morning fatigue profiles and evaluate for differences among the subgroups in demographic and clinical characteristics, as well as the severity of common symptoms and quality of life (QOL) outcomes.
Methods
Oncology outpatients receiving chemotherapy (n = 1342) completed self-report questionnaires to assess pain and morning fatigue, a total of six times over two cycles of chemotherapy. Joint latent profile analysis was used to identify subgroups of patients with distinct pain and morning fatigue profiles. Differences among the classes were evaluated using parametric and non-parametric tests.
Results
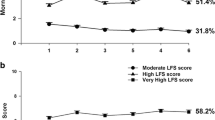
Five distinct profiles were identified (no pain and low morning fatigue (27.6%), moderate pain and low morning fatigue (28.2%), moderate pain and morning fatigue (28.0%), moderate pain and increasing and decreasing morning fatigue (6.9%), severe pain and very high morning fatigue (9.3%)). Patients with the three worst profiles had clinically meaningful levels of depression and sleep disturbance and decrements in QOL.
Conclusions
Over 44% of the sample had moderate to high levels of both pain and morning fatigue. Unrelieved pain may contribute to disturbed sleep which results in higher levels of morning fatigue. Clinicians need to assess for pain and fatigue, as well as sleep disturbance during chemotherapy.

Similar content being viewed by others
Data availability
Available with reasonable request.
Code availability
Not applicable.
References
Abdel-Kader K, Jhamb M, Mandich LA, Yabes J, Keene RM, Beach S, Buysse DJ, Unruh ML (2014) Ecological momentary assessment of fatigue, sleepiness, and exhaustion in ESKD. BMC Nephrol 15:29
Al Maqbali M (2021) Cancer-related fatigue: an overview. Br J Nurs 30:S36–S43
Al Maqbali M, Al Sinani M, Al Naamani Z, Al Badi K, Tanash MI (2021) Prevalence of fatigue in patients with cancer: a systematic review and meta-analysis. J Pain Symptom Manag 61(167–189):e114
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG (2001) AUDIT: The Alcohol Use Disorders Identification Test: guidelines for use in primary care. World Health Organization, Geneva, Switzerland
Barbour KE, Helmick CG, Boring M, Zhang X, Lu H (2014) Holt JB (2016) Prevalence of doctor-diagnosed arthritis at state and county levels - United States. MMWR Morb Mortal Wkly Rep 65:489–494
Beck SL, Dudley WN, Barsevick A (2005) Pain, sleep disturbance, and fatigue in patients with cancer: using a mediation model to test a symptom cluster. Oncol Nurs Forum 32:542
Berger AM, Mooney K, Banerjee A, Breitbart WS, Carpenter CM, Chang Y, Cleeland C, Davis E, Dest V, DuBenske LL, Esclante CP, Fernandes Robles C, Garcia S, Jankowski C, Jatoi A, Kinczewski LE, Loggers ET, Mandrell B, McInnes S, Meyer F, Murphy BA, Palesh O, Patel H, Riba MB, Roshal A, Rugo HS, Salvador C, Wagner-Johnston N, Walter MB, Webb JA (2020) NCCN Guidelines Version 1 2020 - cancer-related fatigue. In: NCCN Guidelines Version 1 2020 - Cancer-Related Fatigue. National Comprehensive Cancer Network
Bjerkeset E, Rohrl K, Schou-Bredal I (2020) Symptom cluster of pain, fatigue, and psychological distress in breast cancer survivors: prevalence and characteristics. Breast Cancer Res Treat 180:63–71
Broemer L, Hinz A, Koch U, Mehnert-Theuerkauf A (2021) Prevalence and severity of pain in cancer patients in Germany. Front Pain Res (Lausanne) 2:703165
Cimprich B, So H, Ronis DL, Trask C (2005) Pre-treatment factors related to cognitive functioning in women newly diagnosed with breast cancer. Psychooncology 14:70–78
Claros-Salinas D, Bratzke D, Greitemann G, Nickisch N, Ochs L, Schroter H (2010) Fatigue-related diurnal variations of cognitive performance in multiple sclerosis and stroke patients. J Neurol Sci 295:75–81
Daut RL, Cleeland CS, Flanery RC (1983) Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain 17:197–210
Davis MP, Rybicki LA, Samala RV, Patel C, Parala-Metz A, Lagman R (2021) Pain or fatigue: which correlates more with suffering in hospitalized cancer patients? Support Care Cancer 29:4535–4542
de Raaf PJ, de Klerk C, van der Rijt CC (2013) Elucidating the behavior of physical fatigue and mental fatigue in cancer patients: a review of the literature. Psychooncology 22:1919–1929
Deyo RA, Mirza SK, Martin BI (2006) Back pain prevalence and visit rates: estimates from US national surveys. Spine 31:2724–2727
Dhruva A, Aouizerat BE, Cooper B, Paul SM, Dodd M, West C, Wara W, Lee K, Dunn LB, Langford DJ, Merriman JD, Baggott C, Cataldo J, Ritchie C, Kober K, Leutwyler H, Miaskowski C (2013) Differences in morning and evening fatigue in oncology patients and their family caregivers. Eur J Oncol Nurs 17:841–848
Dhruva A, Aouizerat BE, Cooper B, Paul SM, Dodd M, West C, Wara W, Lee K, Dunn LB, Langford DJ, Merriman JD, Baggott C, Cataldo J, Ritchie C, Kober KM, Leutwyler H, Miaskowski C (2015) Cytokine gene associations with self-report ratings of morning and evening fatigue in oncology patients and their family caregivers. Biol Res Nurs 17:175–184
Dimsdale JE, Ancoli-Israel S, Elsmore TF, Gruen W (2003) Taking fatigue seriously: I Variations in fatigue sampled repeatedly in healthy controls. J Med Eng Technol 27:218–222
Dodd MJ, Miaskowski C, Paul SM (2001) Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum 28:465–470
Erturk M, Yildirim Y, Kilic SP, Ozer S, Aykar FS (2015) Pain and fatigue in elderly cancer patients: Turkey example Holist. Nurs Pract 29:167–173
Extermann M, Bonetti M, Sledge GW, O’Dwyer PJ, Bonomi P, Benson AB 3rd (2004) MAX2–a convenient index to estimate the average per patient risk for chemotherapy toxicity; validation in ECOG trials. Eur J Cancer 40:1193–1198
Fletcher BS, Paul SM, Dodd MJ, Schumacher K, West C, Cooper B, Lee K, Aouizerat B, Swift P, Wara W, Miaskowski CA (2008) Prevalence, severity, and impact of symptoms on female family caregivers of patients at the initiation of radiation therapy for prostate cancer. J Clin Oncol 26:599–605
Flowers E, Miaskowski C, Conley Y, Hammer MJ, Levine J, Mastick J, Paul S, Wright F, Kober K (2018) Differential expression of genes and differentially perturbed pathways associated with very high evening fatigue in oncology patients receiving chemotherapy. Support Care Cancer 26:739–750
Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS (2009) The rising prevalence of chronic low back pain. Arch Intern Med 169:251–258
Friedman DR, Patil V, Li C, Rassmussen KM, Burningham Z, Hamilton-Hill S, Kelley MJ, Halwani AS (2022) Integration of patient-reported outcome measures in the electronic health record: The Veterans Affairs Experience JCO Clin. Cancer Informatics 6:e2100086
Gay CL, Lee KA, Lee SY (2004) Sleep patterns and fatigue in new mothers and fathers. Biol Res Nurs 5:311–318
Holtzman S, Newth S, Delongis A (2004) The role of social support in coping with daily pain among patients with rheumatoid arthritis. J Health Psychol 9:677–695
Jhamb M, Abdel-Kader K, Yabes J, Wang Y, Weisbord SD, Unruh M, Steel JL (2019) Comparison of fatigue, pain, and depression in patients with advanced kidney disease and cancer-symptom burden and clusters. J Pain Symptom Manage 57:566–575
Jung T, Wickrama KAS (2008) An introduction to latent class growth analysis and growth mixture modeling Soc Personal Psychol. Compass 2:302–317
Karnofsky D, Abelmann WH, Craver LV, Burchenal JH (1948) The use of nitrogen mustards in the palliative treatment of carcinoma. Cancer 1:634–656
Kim HJ, Malone PS, Barsevick AM (2014) Subgroups of cancer patients with unique pain and fatigue experiences during chemotherapy. J Pain Symptom Manage 48:558–568
Ko HJ, Seo SJ, Youn CH, Kim HM, Chung SE (2013) The association between pain and depression, anxiety, and cognitive function among advanced cancer patients in the hospice ward. Korean J Fam Med 34:347–356
Kober KM, Cooper BA, Paul SM, Dunn LB, Levine JD, Wright F, Hammer MJ, Mastick J, Venook A, Aouizerat BE, Miaskowski C (2016) Subgroups of chemotherapy patients with distinct morning and evening fatigue trajectories. Support Care Cancer 24:1473–1485
Kober KM, Dunn L, Mastick J, Cooper B, Langford D, Melisko M, Venook A, Chen LM, Wright F, Hammer M, Schmidt BL, Levine J, Miaskowski C, Aouizerat BE (2016) Gene expression profiling of evening fatigue in women undergoing chemotherapy for breast cancer. Biol Res Nurs 18:370–385
Kober KM, Roy R, Dhruva A, Conley YP, Chan RJ, Cooper B, Olshen A, Miaskowski C (2021) Prediction of evening fatigue severity in outpatients receiving chemotherapy: less may be more Fatigue. Biomed Health Behav 9:14–32
Krebber AM, Buffart LM, Kleijn G, Riepma IC, de Bree R, Leemans CR, Becker A, Brug J, van Straten A, Cuijpers P, Verdonck-de Leeuw IM (2014) Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psychooncology 23:121–130
Kwekkeboom K, Zhang Y, Campbell T, Coe CL, Costanzo E, Serlin RC, Ward S (2018) Randomized controlled trial of a brief cognitive-behavioral strategies intervention for the pain, fatigue, and sleep disturbance symptom cluster in advanced cancer. Psychooncology 27:2761–2769
Lee KA (1992) Self-reported sleep disturbances in employed women Sleep 15:493–498
Lee KA, Hicks G, Nino-Murcia G (1991) Validity and reliability of a scale to assess fatigue. Psychiatry Res 36:291–298
Lee KA, Portillo CJ, Miramontes H (1999) The fatigue experience for women with human immunodeficiency virus. J Obstet Gynecol Neonatal Nurs 28:193–200
Lerdal A (1998) A concept analysis of energy Its meaning in the lives of three individuals with chronic illness. Scand J Caring Sci 12:3–10
Lerdal A (2002) A theoretical extension of the concept of energy through an empirical study. Scand J Caring Sci 16:197–206
Lerdal A, Gay CL, Aouizerat BE, Portillo CJ, Lee KA (2011) Patterns of morning and evening fatigue among adults with HIV/AIDS. J Clin Nurs 20:2204–2216
Lerdal A, Kottorp A, Gay C, Aouizerat BE, Lee KA, Miaskowski C (2016) A Rasch analysis of assessments of morning and evening fatigue in oncology patients using the Lee Fatigue Scale. J Pain Symptom Manage 51:1002–1012
Lerdal A, Kottorp A, Gay CL, Lee KA (2013) Lee fatigue and energy scales: exploring aspects of validity in a sample of women with HIV using an application of a Rasch model. Psychiatry Res 205:241–246
Lin Y, Bailey DE, Docherty SL, Porter LS, Cooper B, Paul S, Kober K, Hammer MJ, Wright F, Conley Y, Levine J, Miaskowski C (2021) Distinct morning and evening fatigue profiles in gastrointestinal cancer during chemotherapy. BMJ Support Palliat Care
Lin Y, Bailey DE, Xiao C, Hammer M, Paul SM, Cooper BA, Conley YP, Levine JD, Kober KM, Miaskowski C (2022) Distinct co-occurring morning and evening fatigue profiles in patients with gastrointestinal cancers receiving chemotherapy. Cancer Nurs
Loh KP, Zittel J, Kadambi S, Pandya C, Xu H, Flannery M, Magnuson A, Bautista J, McHugh C, Mustian K, Dale W, Duberstein P, Mohile SG (2018) Elucidating the associations between sleep disturbance and depression, fatigue, and pain in older adults with cancer. J Geriatr Oncol 9:464–468
Ma Y, He B, Jiang M, Yang Y, Wang C, Huang C, Han L (2020) Prevalence and risk factors of cancer-related fatigue: a systematic review and meta-analysis. Int J Nurs Stud 111:103707
Maglinte GA, Hays RD, Kaplan RM (2012) US general population norms for telephone administration of the SF-36v2. J Clin Epidemiol 65:497–502
Miaskowski C, Cooper BA, Paul SM, Dodd M, Lee K, Aouizerat BE, West C, Cho M, Bank A (2006) Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: a cluster analysis. Oncol Nurs Forum 33:E79-89
Miaskowski C, Paul SM, Snowberg K, Abbott M, Borno HT, Chang SM, Chen LM, Cohen B, Cooper BA, Hammer MJ, Kenfield SA, Kober KM, Laffan A, Levine JD, Pozzar R, Rhoads K, Tsai KK, Van Blarigan EL, Van Loon K (2021) Loneliness and symptom burden in oncology patients during the COVID-19 pandemic. Cancer 127:3246–3253
Miladinia M, Baraz S, Ramezani M, Malehi AS (2018) The relationship between pain, fatigue, sleep disorders and quality of life in adult patients with acute leukaemia: during the first year after diagnosis. Eur J Cancer Care (Engl) 27(1)
Morse L, Kober KM, Viele C, Cooper BA, Paul SM, Conley YP, Hammer M, Levine JD, Miaskowski C (2021) Subgroups of patients undergoing chemotherapy with distinct cognitive fatigue and evening physical fatigue profiles. Support Care Cancer 29:7985–7998
Muthen B, Shedden K (1999) Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics 55:463–469
Muthén L, Muthén B (2009) Mplus statistical analysis with latent variables User’s guide 7
Muthen LK, Muthen BO (1998-2020) Mplus User's Guide (8th ed.). Muthen & Muthen, Los Angeles, CA
Padilla GV, Ferrell B, Grant MM, Rhiner M (1990) Defining the content domain of quality of life for cancer patients with pain. Cancer Nurs 13:108–115
Patrick DL, Ferketich SL, Frame PS, Harris JJ, Hendricks CB, Levin B, Link MP, Lustig C, McLaughlin J, Reid LD, Turrisi AT 3rd, Unutzer J, Vernon SW, National Institutes of Health State-of-the-Science P (2004) National Institutes of Health State-of-the-Science Conference Statement: symptom management in cancer: pain, depression, and fatigue, July 15–17. J Natl Cancer Inst Monogr 2002:9–16
Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E (2011) The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthr Cartil 19:1270–1285
Pud D, Ben Ami S, Cooper BA, Aouizerat BE, Cohen D, Radiano R, Naveh P, Nikkhou-Abeles R, Hagbi V, Kachta O, Yaffe A, Miaskowski C (2008) The symptom experience of oncology outpatients has a different impact on quality-of-life outcomes. J Pain Symptom Manage 35:162–170
Radloff LS (1977) The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN (2003) The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum 49:156–163
Schepman P, Thakkar S, Robinson R, Malhotra D, Emir B, Beck C (2021) Moderate to severe osteoarthritis pain and its impact on patients in the United States: a national survey. J Pain Res 14:2313–2326
Shin J, Harris C, Oppegaard K, Kober KM, Paul SM, Cooper BA, Hammer M, Conley Y, Levine JD, Miaskowski C (2022) Worst pain severity profiles of oncology patients are associated with significant stress and multiple co-occurring symptoms. J Pain 23:74–88
Spielberger CG, Gorsuch RL, Suchene R, Vagg PR, Jacobs GA (1983) Manual for the State-Anxiety (Form Y): self evaluation questionnaire. Consulting Psychologists Press, Palo Alto, CA
Tolentino JC, Schmidt SL (2018) DSM-5 Criteria and depression severity: implications for clinical practice Front Psychiatry 9:450
van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ (2016) Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage 51(1070–1090):e1079
Van Looveren E, Bilterys T, Munneke W, Cagnie B, Ickmans K, Mairesse O, Malfliet A, De Baets L, Nijs J, Goubert D, Danneels L, Moens M, Meeus M (2021) The association between sleep and chronic spinal pain: a systematic review from the last decade J Clin Med 10(17):3836
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Wright F, Cooper BA, Conley YP, Hammer MJ, Chen LM, Paul SM, Levine JD, Miaskowski C, Kober KM (2017) Distinct evening fatigue profiles in oncology outpatients receiving chemotherapy Fatigue. Biomed Health Behav 5:131–144
Wright F, D’Eramo Melkus G, Hammer M, Schmidt BL, Knobf MT, Paul SM, Cartwright F, Mastick J, Cooper BA, Chen LM, Melisko M, Levine JD, Kober K, Aouizerat BE, Miaskowski C (2015) Predictors and trajectories of morning fatigue are distinct from evening fatigue. J Pain Symptom Manage 50:176–189
Wright F, D’Eramo Melkus G, Hammer M, Schmidt BL, Knobf MT, Paul SM, Cartwright F, Mastick J, Cooper BA, Chen LM, Melisko M, Levine JD, Kober K, Aouizerat BE, Miaskowski C (2015) Trajectories of evening fatigue in oncology outpatients receiving chemotherapy. J Pain Symptom Manage 50:163–175
Wright F, Dunn LB, Paul SM, Conley YP, Levine JD, Hammer MJ, Cooper BA, Miaskowski C, Kober KM (2019) Morning fatigue severity profiles in oncology outpatients receiving chemotherapy. Cancer Nurs 42:355–364
Wright F, Hammer M, Paul SM, Aouizerat BE, Kober KM, Conley YP, Cooper BA, Dunn LB, Levine JD, Melkus GD, Miaskowski C (2017) Inflammatory pathway genes associated with inter-individual variability in the trajectories of morning and evening fatigue in patients receiving chemotherapy. Cytokine 91:187–210
Wright F, Kober KM, Cooper BA, Paul SM, Conley YP, Hammer M, Levine JD, Miaskowski C (2020) Higher levels of stress and different coping strategies are associated with greater morning and evening fatigue severity in oncology patients receiving chemotherapy. Support Care Cancer 28:4697–4706
Funding
This work was supported by a grant from the National Cancer Institute (NCI, CA134900). Dr. Miaskowski is an American Cancer Society Clinical Research Professor.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Dr. Miaskowski, Dr. Cooper, and Dr. Paul. The first draft of the manuscript was written by Ms. Bouvron and Dr. Miaskowski. All of the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study procedures were approved by the Committee on Human Research at the University of California, San Francisco and the Institutional Review Board at each of the study sites. This study was performed in accordance with the ethical standards as laid down in the 1964 Helsinki Declaration.
Consent to participate
Informed consent was obtained from all individual participants included in this study.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bouvron, B., Mackin, L., Kober, K.M. et al. Impact of worst pain severity and morning fatigue profiles on oncology outpatients’ symptom burden and quality of life. Support Care Cancer 30, 9929–9944 (2022). https://doi.org/10.1007/s00520-022-07431-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07431-6