Abstract
Purpose
Exercise is beneficial for prostate cancer patients’ physical functioning; however, effects on social and cognitive functioning are inconsistent. This meta-analysis of exercise interventions for prostate cancer patients had two aims: the primary aim was to evaluate the effects of exercise interventions on social functioning; the secondary aim was to consider additional outcomes of cognitive functioning as well as adverse events.
Methods
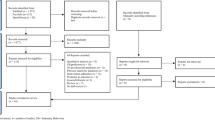
Electronic databases (Embase, MEDLINE, PubMed, PsycINFO, and the Chinese database Airti Library) were searched for relevant papers (1987–2019), which included hand searching. After careful inspection, 10 relevant randomized controlled trials were analyzed using Comprehensive Meta-Analysis software; pooled means determined social and cognitive functioning.
Results
Meta-analysis of summary scores (fixed-effects model) showed an overall beneficial effect of exercise on social functioning (Hedges’ g = 0.35, 95% CI [0.193, 0.515], p < 0.001) and cognitive functioning (Hedges’ g = 0.35, 95% CI [0.123, 0.575], p < 0.01) in men with prostate cancer when compared to controls. Intervention durations of 12–16 and 24–48 weeks that provided supervised aerobic exercise combined with resistance exercise sessions had a small to medium effect on social functioning compared to controls. One exercise group experienced one serious, but non-fatal, adverse event due to a higher exercise intensity (50–75% VO2max).
Discussion and recommendations
To the best of our knowledge, this is the first meta-analysis to examine the effects of exercise interventions on cognitive functioning among prostate cancer patients. We suggest further research be conducted to confirm these findings.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.




Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
American Cancer Society [ACS] (2017) Survival rates for prostate cancer Retrieved from https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/survival-rates.html
Rhee H, Gunter JH, Heathcote P, Ho K, Stricker P, Corcoran NM, Nelson CC (2015) Adverse effects of androgen-deprivation therapy in prostate cancer and their management. BJU Int 115(Suppl 5):3–13. https://doi.org/10.1111/bju.12964
Mundell NL, Daly RM, Macpherson H, Fraser SF (2017) Cognitive decline in prostate cancer patients undergoing ADT: a potential role for exercise training. Endocr Relat Cancer 24:R145–r155. https://doi.org/10.1530/erc-16-0493
O'Higgins CM, Brady B, O'Connor B, Walsh D, Reilly RB (2018) The pathophysiology of cancer-related fatigue: current controversies. Support Care Cancer 26:3353–3364. https://doi.org/10.1007/s00520-018-4318-7
Watts S, Leydon G, Birch B, Prescott P, Lai L, Eardley S, Lewith G (2014) Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 4:e003901. https://doi.org/10.1136/bmjopen-2013-003901
Forsythe LP, Kent EE, Weaver KE, Buchanan N, Hawkins NA, Rodriguez JL, Ryerson AB, Rowland JH (2013) Receipt of psychosocial care among cancer survivors in the United States. J Clin Oncol Off J Am Soc Clin Oncol 31:1961–1969. https://doi.org/10.1200/jco.2012.46.2101
Medina-Perucha L, Yousaf O, Hunter MS, Grunfeld EA (2017) Barriers to medical help-seeking among older men with prostate cancer. J Psychosoc Oncol 35:531–543. https://doi.org/10.1080/07347332.2017.1312661
Cormie P, Turner B, Kaczmarek E, Drake D, Chambers SK (2015) A qualitative exploration of the experience of men with prostate cancer involved in supervised exercise programs. Oncol Nurs Forum 42:24–32. https://doi.org/10.1188/15.Onf.24-32
Trinh L, Arbour-Nicitopoulos KP, Sabiston CM, Alibhai SM, Jones JM, Berry SR, Loblaw A, Faulkner GE (2015) A qualitative study exploring the perceptions of sedentary behavior in prostate cancer survivors receiving androgen-deprivation therapy. Oncol Nurs Forum 42:398–406. https://doi.org/10.1188/15.Onf.398-406
Fox L, Cahill F, Burgess C, Peat N, Rudman S, Kinsella J, Cahill D, George G, Santaolalla A, Van Hemelrijck M (2017) Real world evidence: a quantitative and qualitative glance at participant feedback from a free-response survey investigating experiences of a structured exercise intervention for men with prostate cancer. Biomed Res Int 2017:3507124. https://doi.org/10.1155/2017/3507124
Lee CE, Kilgour A, Lau YK (2012) Efficacy of walking exercise in promoting cognitive-psychosocial functions in men with prostate cancer receiving androgen deprivation therapy. BMC Cancer 12:324. https://doi.org/10.1186/1471-2407-12-324
Zopf EM, Bloch W, Machtens S, Zumbe J, Rubben H, Marschner S, Kleinhorst C, Schulte-Frei B, Herich L, Felsch M, Predel HG, Braun M, Baumann FT (2015) Effects of a 15-month supervised exercise program on physical and psychological outcomes in prostate cancer patients following prostatectomy: the ProRehab study. Integr Cancer Ther 14:409–418. https://doi.org/10.1177/1534735415583552
Schmid D, Leitzmann MF (2014) Association between physical activity and mortality among breast cancer and colorectal cancer survivors: a systematic review and meta-analysis. Ann Oncol 25:1293–1311. https://doi.org/10.1093/annonc/mdu012
Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM (2012) Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst 104:815–840. https://doi.org/10.1093/jnci/djs207
Li T, Wei S, Shi Y, Pang S, Qin Q, Yin J, Deng Y, Chen Q, Wei S, Nie S, Liu L (2016) The dose-response effect of physical activity on cancer mortality: findings from 71 prospective cohort studies. Br J Sports Med 50:339–345. https://doi.org/10.1136/bjsports-2015-094927
Bourke L, Smith D, Steed L, Hooper R, Carter A, Catto J, Albertsen PC, Tombal B, Payne HA, Rosario DJ (2016) Exercise for men with prostate cancer: a systematic review and meta-analysis. Eur Urol 69:693–703. https://doi.org/10.1016/j.eururo.2015.10.047
Teleni L, Chan RJ, Chan A, Isenring EA, Vela I, Inder WJ, McCarthy AL (2016) Exercise improves quality of life in androgen deprivation therapy-treated prostate cancer: systematic review of randomised controlled trials. Endocr Relat Cancer 23:101–112. https://doi.org/10.1530/erc-15-0456
Gardner JR, Livingston PM, Fraser SF (2014) Effects of exercise on treatment-related adverse effects for patients with prostate cancer receiving androgen-deprivation therapy: a systematic review. J Clin Oncol Off J Am Soc Clin Oncol 32:335–346. https://doi.org/10.1200/jco.2013.49.5523
Menichetti J, Villa S, Magnani T, Avuzzi B, Bosetti D, Marenghi C, Morlino S, Rancati T, Van Poppel H, Salvioni R, Valdagni R, Bellardita L (2016) Lifestyle interventions to improve the quality of life of men with prostate cancer: a systematic review of randomized controlled trials. Crit Rev Oncol Hematol 108:13–22. https://doi.org/10.1016/j.critrevonc.2016.10.007
Baumann FT, Zopf EM, Bloch W (2012) Clinical exercise interventions in prostate cancer patients--a systematic review of randomized controlled trials. Support Care Cancer 20:221–233. https://doi.org/10.1007/s00520-011-1271-0
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Bmj 343:d5928. https://doi.org/10.1136/bmj.d5928
Cormie P, Galvao DA, Spry N, Joseph D, Chee R, Taaffe DR, Chambers SK, Newton RU (2015) Can supervised exercise prevent treatment toxicity in patients with prostate cancer initiating androgen-deprivation therapy: a randomised controlled trial. BJU Int 115:256–266. https://doi.org/10.1111/bju.12646
Cormie P, Newton RU, Spry N, Joseph D, Taaffe DR, Galvao DA (2013) Safety and efficacy of resistance exercise in prostate cancer patients with bone metastases. Prostate Cancer Prostatic Dis 16:328–335. https://doi.org/10.1038/pcan.2013.22
Galvao DA, Spry N, Denham J, Taaffe DR, Cormie P, Joseph D, Lamb DS, Chambers SK, Newton RU (2014) A multicentre year-long randomised controlled trial of exercise training targeting physical functioning in men with prostate cancer previously treated with androgen suppression and radiation from TROG 03.04 RADAR. Eur Urol 65:856–864. https://doi.org/10.1016/j.eururo.2013.09.041
Galvao DA, Taaffe DR, Spry N, Joseph D, Newton RU (2010) Combined resistance and aerobic exercise program reverses muscle loss in men undergoing androgen suppression therapy for prostate cancer without bone metastases: a randomized controlled trial. J Clin Oncol Off J Am Soc Clin Oncol 28:340–347. https://doi.org/10.1200/jco.2009.23.2488
Livingston PM, Craike MJ, Salmon J, Courneya KS, Gaskin CJ, Fraser SF, Mohebbi M, Broadbent S, Botti M, Kent B (2015) Effects of a clinician referral and exercise program for men who have completed active treatment for prostate cancer: a multicenter cluster randomized controlled trial (ENGAGE). Cancer 121:2646–2654. https://doi.org/10.1002/cncr.29385
Nilsen TS, Raastad T, Skovlund E, Courneya KS, Langberg CW, Lilleby W, Fossa SD, Thorsen L (2015) Effects of strength training on body composition, physical functioning, and quality of life in prostate cancer patients during androgen deprivation therapy. Acta Oncol 54:1805–1813. https://doi.org/10.3109/0284186x.2015.1037008
Jones LW, Hornsby WE, Freedland SJ, Lane A, West MJ, Moul JW, Ferrandino MN, Allen JD, Kenjale AA, Thomas SM, Herndon JE 2nd, Koontz BF, Chan JM, Khouri MG, Douglas PS, Eves ND (2014) Effects of nonlinear aerobic training on erectile dysfunction and cardiovascular function following radical prostatectomy for clinically localized prostate cancer. Eur Urol 65:852–855
Monga U, Garber SL, Thornby J, Vallbona C, Kerrigan AJ, Monga TN, Zimmermann KP (2007) Exercise prevents fatigue and improves quality of life in prostate cancer patients undergoing radiotherapy. Arch Phys Med Rehabil 88:1416–1422. https://doi.org/10.1016/j.apmr.2007.08.110
Hojan K, Kwiatkowska-Borowczyk E, Leporowska E, Gorecki M, Ozga-Majchrzak O, Milecki T, Milecki P (2016) Physical exercise for functional capacity, blood immune function, fatigue, and quality of life in high-risk prostate cancer patients during radiotherapy: a prospective, randomized clinical study. Eur J Phys Rehabil Med 52:489–501
Hojan K, Kwiatkowska-Borowczyk E, Leporowska E, Milecki P (2017) Inflammation, cardiometabolic markers, and functional changes in men with prostate cancer. A randomized controlled trial of a 12month exercise program. Pol Arch Intern Med 127:25–35. https://doi.org/10.20452/pamw.3888
Borenstein M (2009) Introduction to meta-analysis. John Wiley & Sons, Chichester
Dwan K, Gamble C, Williamson PR, Kirkham JJ (2013) Systematic review of the empirical evidence of study publication bias and outcome reporting bias - an updated review. PLoS One 8:e66844
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Riley RD, Higgins JP, Deeks JJ (2011) Interpretation of random effects meta-analyses. BMJ 342:d549
Kriston L (2013) Dealing with clinical heterogeneity in meta-analysis. Assumptions, methods, interpretation. Int J Methods Psychiatr Res 22:1–15. https://doi.org/10.1002/mpr.1377
Borenstein M, Higgins JP (2013) Meta-analysis and subgroups. Prev Sci 14:134–143. https://doi.org/10.1007/s11121-013-0377-7
Phan K, Tian DH, Cao C, Black D, Yan TD (2015) Systematic review and meta-analysis: techniques and a guide for the academic surgeon. Ann Cardiothorac Surg 4:112–122. https://doi.org/10.3978/j.issn.2225-319X.2015.02.04
Langston B, Armes J, Levy A, Tidey E, Ream E (2013) The prevalence and severity of fatigue in men with prostate cancer: a systematic review of the literature. Support Care Cancer 21:1761–1771. https://doi.org/10.1007/s00520-013-1751-5
Keogh JW, MacLeod RD (2012) Body composition, physical fitness, functional performance, quality of life, and fatigue benefits of exercise for prostate cancer patients: a systematic review. J Pain Symptom Manag 43:96–110. https://doi.org/10.1016/j.jpainsymman.2011.03.006
Keilani M, Hasenoehrl T, Baumann L, Ristl R, Schwarz M, Marhold M, Sedghi Komandj T, Crevenna R (2017) Effects of resistance exercise in prostate cancer patients: a meta-analysis. Support Care Cancer 25:2953–2968. https://doi.org/10.1007/s00520-017-3771-z
Gao Y-F, He W-Y, He X-Y, Huang Y-L, Gou X (2017) Exercise overcome adverse effects among prostate cancer patients receiving androgen deprivation therapy: an update meta-analysis. Medicine 96:e7368. https://doi.org/10.1097/md.0000000000007368
Yang B, Wang J (2017) Effects of exercise on cancer-related fatigue and quality of life in prostate cancer patients undergoing androgen deprivation therapy: a meta-analysis of randomized clinical trials. Chin Med Sci J 32:13–21
Vashistha V, Singh B, Kaur S, Prokop LJ, Kaushik D (2016) The effects of exercise on fatigue, Quality of life, and psychological function for men with prostate cancer: systematic review and meta-analyses. Eur Urol Focus 2:284–295. https://doi.org/10.1016/j.euf.2016.02.011
Dunn J, Casey C, Sandoe D, Hyde MK, Cheron-Sauer MC, Lowe A, Oliffe JL, Chambers SK (2018) Advocacy, support and survivorship in prostate cancer. Eur J Cancer Care 27:e12644. https://doi.org/10.1111/ecc.12644
Cormie P, Oliffe JL, Wootten AC, Galvao DA, Newton RU, Chambers SK (2016) Improving psychosocial health in men with prostate cancer through an intervention that reinforces masculine values - exercise. Psycho-oncology 25:232–235. https://doi.org/10.1002/pon.3867
Hyde MK, Zajdlewicz L, Wootten AC, Nelson CJ, Lowe A, Dunn J, Chambers SK (2016) Medical help-seeking for sexual concerns in prostate cancer survivors. Sex Med 4:e7–e17. https://doi.org/10.1016/j.esxm.2015.12.004
Hyde MK, Newton RU, Galvao DA, Gardiner RA, Occhipinti S, Lowe A, Wittert GA, Chambers SK (2017) Men's help-seeking in the first year after diagnosis of localised prostate cancer Eur J Cancer Care 26 https://doi.org/10.1111/ecc.12497
Yousaf O, Grunfeld EA, Hunter MS (2015) A systematic review of the factors associated with delays in medical and psychological help-seeking among men. Health Psychol Rev 9:264–276. https://doi.org/10.1080/17437199.2013.840954
Wenger LM (2013) 'Living under assault': men making sense of cancer. Eur J Cancer Care 22:389–399. https://doi.org/10.1111/ecc.12042
Karunanithi G, Sagar RP, Joy A, Vedasoundaram P (2018) Assessment of psychological distress and its effect on quality of life and social functioning in cancer patients. Indian J Palliat Care 24:72–77. https://doi.org/10.4103/ijpc.Ijpc_104_17
Cheng S-J, Yu H-K, Chen Y-C, Chen C-Y, Lien W-C, Yang P-Y, Hu G-C (2013) Physical activity and risk of cardiovascular disease among older adults. Int J Gerontol 7:133–136. https://doi.org/10.1016/j.ijge.2013.03.001
Lachman S, Boekholdt SM, Luben RN, Sharp SJ, Brage S, Khaw K-T, Peters RJG, Wareham NJ (2018) Impact of physical activity on the risk of cardiovascular disease in middle-aged and older adults: EPIC Norfolk prospective population study. Eur J Prev Cardiol 25:200–208. https://doi.org/10.1177/2047487317737628
Fleg JL (2016) Salutary effects of high-intensity interval training in persons with elevated cardiovascular risk F1000Research 5 https://doi.org/10.12688/f1000research.8778.1
American College Of Sports Medicine [ACSM] (2014) ACSM's guidelines for exercise testing and prescription. Lippincott Williams & Wilkins, Philadelphia
Mittleman MA, Mostofsky E (2011) Physical, psychological and chemical triggers of acute cardiovascular events: preventive strategies. Circulation 124:346–354. https://doi.org/10.1161/circulationaha.110.968776
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Fang, YY., Lee, YH., Chan, JC. et al. Effects of exercise interventions on social and cognitive functioning of men with prostate cancer: a meta-analysis. Support Care Cancer 28, 2043–2057 (2020). https://doi.org/10.1007/s00520-019-05278-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05278-y