Abstract
Purpose
Cancer diagnosis and treatment can generate substantial distress for both survivors and their family caregivers. The primary aim of this investigation is to test a model of dyadic interdependence in distress experienced by cancer survivors and their caregivers to determine if each influences the other.
Methods
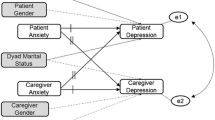
To test this prediction, 209 Latinas with breast cancer and their family caregivers (dyads) were followed for 4 waves of assessment over the course of 6 months. Both psychological (depression, anxiety, perceived stress) and physical (number of symptoms, symptom distress) indicators of distress were assessed. Longitudinal analyses of dyadic data were performed in accordance with the actor-partner interdependence model.
Results
Findings indicated that psychological distress was interdependent between cancer survivors and their caregivers over the 6 months of observation. However, there was no such evidence of interdependence on indicators of physical distress.
Conclusions
These findings are consistent with emotional contagion processes and point to the potential importance of caregiver well-being for the welfare of Latina breast cancer survivors.

Similar content being viewed by others
References
Guo F, Kuo YF, Shih YCT, Giordano SH, Berenson AB (2018) Trends in breast cancer mortality by stage at diagnosis among young women in the United States. Cancer 124(17):3500–3509. https://doi.org/10.1002/cncr.31638
Crocetti E, Bossard N, Uhry Z, Roche L, Rossi S, Capocaccia R, Faivre J, Group GE-W (2017) Trends in net survival from 15 cancers in six European Latin countries: the SUDCAN population-based study material. Eur J Cancer Prev 26:S3-S8. https://doi.org/10.1097/CEJ.0000000000000300
Mitchell A, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N (2011) Prevalence of depression, anxity and adjustment disorder in oncological, haematological and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 12:160–174
Stenberg U, Ruland CM, Miaskowski C (2010) Review of the literature on the effects of caring for a patient with cancer. Psycho-oncology 19:1013–1025
Yanez B, Maggard Gibbons M, Moreno PI, Jorge A, Stanton AL (2016) Predictors of psychological outcomes in a longitudinal study of Latina breast cancer survivors. Psychol Health 31(11):1359–1374. https://doi.org/10.1080/08870446.2016.1208821
Lam WW, Shing YT, Bonanno GA, Mancini AD, Fielding R (2012) Distress trajectories at the first year diagnosis of breast cancer in relation to 6 years survivorship. Psycho-oncology 21(1):90–99. https://doi.org/10.1002/pon.1876
Hasson-Ohayon I, Goldzweig G, Braun M, Galinsky D (2010) Women with advanced breast cancer and their spouses: diversity of support and psychological distress. Psycho-oncology 19(11):1195–1204. https://doi.org/10.1002/pon.1678
Harding R, List S, Epiphaniou E, Jones H (2012) How can informal caregivers in cancer and palliative care be supported? An updated systematic literature review of interventions and their effectiveness. Palliat Med 26(1):7–22. https://doi.org/10.1177/0269216311409613
Yarbroff KR, Kim Y (2009) Time costs associated with informal caregiving for cancer survivors. Cancer 115(18 Suppl):4362–4373
Teixeira RJ, Applebaum AJ, Bhatia S, Brandao T (2018) The impact of coping strategies of cancer caregivers on psychophysiological outcomes: an integrative review. Psychol Res Behav Manag 11:207–215. https://doi.org/10.2147/PRBM.S164946
Kotronoulas G, Wengstrom Y, Kearney N (2013) Sleep patterns and sleep-impairing factors of persons providing informal care for people with cancer: a critical review of the literature. Cancer Nurs 36(1):E1–E15. https://doi.org/10.1097/NCC.0b013e3182456c38
Bambauer KZ, Zhang B, Maciejewski PK, Sahay N, Pirl WF, Block SD, Prigerson HG (2006) Mutuality and specificity of mental disorders in advanced cancer patients and caregivers. Soc Psychiatry Psychiatr Epidemiol 41(10):819–824
Butow PN, Price MA, Bell ML, Webb PM, deFazio A, Australian Ovarian Cancer Study G, Australian Ovarian Cancer Study Quality Of Life Study I, Friedlander M (2014) Caring for women with ovarian cancer in the last year of life: a longitudinal study of caregiver quality of life, distress and unmet needs. Gynecol Oncol 132(3):690–697. https://doi.org/10.1016/j.ygyno.2014.01.002
Kim Y, Carver CS, Shaffer KM, Gansler T, Cannady RS (2015) Cancer caregiving predicts physical impairments: roles of earlier caregiving stress and being a spousal caregiver. Cancer 121(2):302–310. https://doi.org/10.1002/cncr.29040
Manne S, Babb J, Pinover W, Horwitz E, Ebbert J (2004) Psychoeducational group intervention for wives of men with prostate cancer. Psycho-oncology 13(1):37–46
Manne S, Ostroff J, Sherman M, Glassman M, Ross SGL, Fox K (2003) Buffering effects of family and friend support on associations between partner unsupportive behaviors and coping among women with breast cancer. J Soc Pers Relat 20(6):771–792
Northouse LL, Mood DW, Montie JE, Sandler HM, Forman JD, Hussain M, Pienta KJ, Smith DC, Sanda MG, Kershaw T (2007) Living with prostate cancer: patients' and spouses' psychosocial status and quality of life. J Clin Oncol 25(27):4171–4177
Rabin EG, Heldt E, Hirakata VN, Bittelbrunn AC, Chachamovich E, Fleck MP (2009) Depression and perceptions of quality of life of breast cancer survivors and their male partners. Oncol Nurs Forum 36(3):E153–E158
Segrin C, Badger TA, Meek P, Lopez AM, Bonham E, Sieger A (2005) Dyadic interdependence on affect and quality-of-life trajectories among women with breast cancer and their partners. J Soc Pers Relat 22(5):673–689
Segrin C, Badger T, Dorros SM, Meek P, Lopez AM (2007) Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psycho-oncology 16(7):634–643
Segrin C, Badger TA, Harrington J (2012) Interdependent psychological quality of life in dyads adjusting to prostate cancer. Health Psychol 31(1):70–79. https://doi.org/10.1037/a0025394
Manne SL, Ostroff JS, Norton TR, Fox K, Goldstein L, Grana G (2006) Cancer-related relationship communication in couples coping with early stage breast cancer. Psycho-oncology 15(3):234–247
Jacobs JM, Shaffer KM, Nipp RD, Fishbein JN, MacDonald J, El-Jawahri A, Pirl WF, Jackson VA, Park ER, Temel JS, Greer JA (2017) Distress is interdependent in patients and caregivers with newly diagnosed incurable cancers. Ann Behav Med 51(4):519–531. https://doi.org/10.1007/s12160-017-9875-3
Katapodi MC, Ellis KR, Schmidt F, Nikolaidis C, Northouse LL (2018) Predictors and interdependence of family support in a random sample of long-term young breast cancer survivors and their biological relatives. Cancer Med 7(10):4980–4992. https://doi.org/10.1002/cam4.1766
Segrin C, Badger TA (2014) Psychological and physical distress are interdependent in breast cancer survivors and their partners. Psychol Health Med 19(6):716–723. https://doi.org/10.1080/13548506.2013.871304
Stokes JE (2017) Mutual influence and older married adults’ anxiety symptoms: results from the Irish Longitudinal Study on Ageing. The Gerontologist 57(3):529–539. https://doi.org/10.1093/geront/gnv147
Hatfield E, Cacioppo JT, Rapson RL (1993) Emotional contagion. Curr Dir Psychol Sci 2(3):96–99. https://doi.org/10.1111/1467-8721.ep10770953
Hatfield E, Cacioppo JT, Rapson RL (1994) Emotional contagion. Cambridge University Press, Paris
Deng H, Hu P (2017) Matching your face or appraising the situation: two paths to emotional contagion. Front Psychol 8:2278. https://doi.org/10.3389/fpsyg.2017.02278
Bonnaud-Antignac A, Hardouin JB, Leger J, Dravet F, Sebille V (2012) Quality of life and coping of women treated for breast cancer and their caregiver. What are the interactions? J Clin Psychol Med Settings 19(3):320–328. https://doi.org/10.1007/s10880-012-9300-9
Milbury K, Badr H, Fossella F, Pisters KM, Carmack CL (2013) Longitudinal associations between caregiver burden and patient and spouse distress in couples coping with lung cancer. Support Care Cancer 21(9):2371–2379. https://doi.org/10.1007/s00520-013-1795-6
Douglas SL, Daly BJ (2013) The impact of patient quality of life and spirituality upon caregiver depression for those with advanced cancer. Palliat Support Care 11(5):389–396. https://doi.org/10.1017/S1478951512000570
Lopez-Class M, Perret-Gentil M, Kreling B, Caicedo L, Mandelblatt J, Graves KD (2011) Quality of life among immigrant Latina breast cancer survivors: realities of culture and enhancing cancer care. J Cancer Educ 26(4):724–733. https://doi.org/10.1007/s13187-011-0249-4
Katiria Perez G, Cruess D (2014) The impact of familism on physical and mental health among Hispanics in the United States. Health Psychol Rev 8(1):95–127. https://doi.org/10.1080/17437199.2011.569936
Badger TA, Segrin C, Sikorskii A, Pasvogel A, Weihs K, Lopez AM, Chalasani P (2019) Randomized controlled trial of supportive care interventions to manage psychological distress and symptoms in Latinas with breast cancer and their informal caregivers. Psychol Health:1–20. https://doi.org/10.1080/08870446.2019.1626395
Correia H (2011) Spanish translations of PROMIS Instruments. Northwestern University, Dept. of Medical Social Sciences
Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, Group PC (2011) Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): depression, anxiety, and anger. Assessment 18(3):263–283. https://doi.org/10.1177/1073191111411667
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24(4):385–396
Hewitt PL, Flett GL et al (1992) The Perceived Stress Scale: factor structure and relation to depression symptoms in a psychiatric sample. J Psychopathol Behav Assess 14(3):247–257
Remor E (2006) Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Span J Psychol 9(1):86–93
Badger TA, Segrin C, Meek P (2011) Development and validation of an instrument for rapidly assessing symptoms: the general symptom distress scale. J Pain Symptom Manag 41(3):535–548. https://doi.org/10.1016/j.jpainsymman.2010.06.011
Kenny DA, Kashy DA, Cook WL (eds) (2006) Dyadic data analysis. Guilford Press, New York
Kenny DAC, W. (1999) Partner effects in relationship research: conceptual issues, analytic difficulties, and illustrations. Pers Relat 6:433–488
Ellis KR, Janevic MR, Kershaw T, Caldwell CH, Janz NK, Northouse L (2016) Meaning-based coping, chronic conditions and quality of life in advanced cancer & caregiving. Psycho-oncology. https://doi.org/10.1002/pon.4146
Kim Y, Kashy DA, Wellisch DK, Spillers RL, Kaw CK, Smith TG (2008) Quality of life of couples dealing with cancer: dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Ann Behav Med 35(2):230–238. https://doi.org/10.1007/s12160-008-9026-y
Shaffer KM, Kim Y, Carver CS (2016) Physical and mental health trajectories of cancer patients and caregivers across the year post-diagnosis: a dyadic investigation. Psychol Health 31(6):655–674. https://doi.org/10.1080/08870446.2015.1131826
Segrin C, Badger T (2010) Psychological distress in different social network members of breast and prostate cancer patients. Res Nurs Health 33(5):450–464
Cleeland CS, Sloan JA, Cella D, Chen C, Dueck AC, Janjan NA, Liepa AM, Mallick R, O’Mara A, Pearson JD, Torigoe Y, Wang XS, Williams LA, Woodruff JF, Force CMT (2013) Recommendations for including multiple symptoms as endpoints in cancer clinical trials: a report from the ASCPRO (Assessing the Symptoms of Cancer Using Patient-Reported Outcomes) Multisymptom Task Force. Cancer 119(2):411–420. https://doi.org/10.1002/cncr.27744
Acknowledgments
We thank the research staff: Maria Figueroa, Karina Othon-Tapia, Xochitl Gaxiola, Mary Pentland, and Molly Hadeed, the community providers who referred survivors to the study, and the study participants.
Funding
This research was supported by a grant no. RSG-12-120-01-CPPB from the American Cancer Society to Terry Badger.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee ( University of Arizona Institutional Review Board ) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
Terry Badger, Chris Segrin, and Alla Sikorskii received grant funding from the American Cancer Society pursuant to the research reported in this manuscript. They have control of all primary data and agree to allow the journal to review the data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Segrin, C., Badger, T.A., Sikorskii, A. et al. Longitudinal dyadic interdependence in psychological distress among Latinas with breast cancer and their caregivers. Support Care Cancer 28, 2735–2743 (2020). https://doi.org/10.1007/s00520-019-05121-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05121-4