Abstract
Purpose
Although many cancer patients benefit from physical activity (PA), healthcare professionals (HCP) still do not promote it routinely. Including different groups of HCP, this study aimed to examine how structural barriers are perceived as impeding by HCP for promoting PA to cancer patients, how the perceptions of structural barriers are associated with promoting PA, and how HCP react to information resources.
Methods
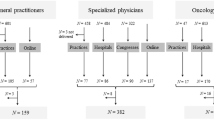
A total of 287 physicians in outpatient care, 242 physicians in inpatient care, and 388 oncology nurses completed our questionnaire (paper-pencil or online). Participants assessed nine different structural barriers (on a 4-point Likert Scale) and reported their PA promotion frequency. Further, they could request three different kinds of information resources about PA in oncological settings.
Results
Across professional groups, more than 70% of HCP indicated that they promoted PA to their cancer patients often or routinely. Oncology nurses indicated that they were more impeded in promoting PA by six structural barriers than physicians (all p < .01). “Not enough time per patient” and “lack of an expert contact person” were associated with a reduced PA promotion in two professional groups (all p < .05). Information resources were requested by 69.5% of the participants: mostly physicians working in outpatient care and especially by those perceiving structural barriers.
Conclusions
Although a big proportion of HCP reported that they frequently promoted PA, our findings suggest that HCP still perceive structural barriers. The perception and influence of structural barriers differed between professional groups, pointing to the importance of profession specific guidance.


Similar content being viewed by others
References
Buffart LM, Kalter J, Sweegers MG, Courneya KS, Newton RU, Aaronson NK, Jacobsen PB, May AM, Galvão DA, Chinapaw MJ, Steindorf K, Irwin ML, Stuiver MM, Hayes S, Griffith KA, Lucia A, Mesters I, van Weert E, Knoop H, Goedendorp MM, Mutrie N, Daley AJ, McConnachie A, Bohus M, Thorsen L, Schulz K-H, Short CE, James EL, Plotnikoff RC, Arbane G, Schmidt ME, Potthoff K, van Beurden M, Oldenburg HS, Sonke GS, van Harten WH, Garrod R, Schmitz KH, Winters-Stone KM, Velthuis MJ, Taaffe DR, van Mechelen W, Kersten M-J, Nollet F, Wenzel J, Wiskemann J, Verdonck-de Leeuw IM, Brug J (2017) Effects and moderators of exercise on quality of life and physical function in patients with cancer: an individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev 52:91–104. https://doi.org/10.1016/j.ctrv.2016.11.010
Mustian KM, Alfano CM, Heckler C, Kleckner AS, Kleckner IR, Leach CR, Mohr D, Palesh OG, Peppone LJ, Piper BF, Scarpato J, Smith T, Sprod LK, Miller SM (2017) Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: a meta-analysis. JAMA Oncol 3(7):961–968. https://doi.org/10.1001/jamaoncol.2016.6914
Segal R, Zwaal C, Green E, Tomasone JR, Loblaw A, Petrella T (2017) Exercise for people with cancer: a systematic review. Curr Oncol 24(4):e290–e315. https://doi.org/10.3747/co.24.3619
Cormie P, Zopf EM, Zhang X, Schmitz KH (2017) The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiol Rev 39(1):71–92. https://doi.org/10.1093/epirev/mxx007
Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvao DA, Pinto BM, Irwin ML, Wolin KY, Segal RJ, Lucia A, Schneider CM, von Gruenigen VE, Schwartz AL (2010) American college of sports medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc 42(7):1409–1426. https://doi.org/10.1249/MSS.0b013e3181e0c112
Crawford JJ, Holt NL, Vallance JK, Courneya KS (2016) A new paradigm for examining the correlates of aerobic, strength, and combined exercise: an application to gynecologic cancer survivors. Support Care Cancer 24(8):1–9. https://doi.org/10.1007/s00520-016-3173-7
Ottenbacher A, Yu M, Moser RP, Phillips SM, Alfano C, Perna FM (2015) Population estimates of meeting strength training and aerobic guidelines, by gender and cancer survivorship status: Findings from the Health Information National Trends Survey (HINTS). J Phys Act Health 12(5):675–679. https://doi.org/10.1123/jpah.2014-0003
Berra K, Rippe J, Manson JE (2015) Making physical activity counseling a priority in clinical practice: the time for action is now. JAMA 314(24):2617–2618. https://doi.org/10.1001/jama.2015.16244
Murphy JL, Girot EA (2013) The importance of nutrition, diet and lifestyle advice for cancer survivors—the role of nursing staff and interprofessional workers. J Clin Nurs 22(11–12):1539–1549. https://doi.org/10.1111/jocn.12053
Rogers LQ, Markwell SJ, Verhulst S, McAuley E, Courneya KS (2009) Rural breast cancer survivors: exercise preferences and their determinants. Psychooncology 18(4):412–421. https://doi.org/10.1002/pon.1497
McGowan EL, Speed-Andrews AE, Blanchard CM, Rhodes RE, Friedenreich CM, Cubs-Reed SN, Courneya KS (2013) Physical activity preferences among a population-based sample of colorectal cancer survivors. Oncol Nurs Forum 40(1):44–52. https://doi.org/10.1188/13.onf.44-52
Tarasenko YN, Miller EA, Chen C, Schoenberg NE (2017) Physical activity levels and counseling by health care providers in cancer survivors. Prev Med 99:211–217. https://doi.org/10.1016/j.ypmed.2017.01.010
Fisher A, Williams K, Beeken R, Wardle J (2015) Recall of physical activity advice was associated with higher levels of physical activity in colorectal cancer patients. BMJ Open 5(4):e006853. https://doi.org/10.1136/bmjopen-2014-006853
Nyrop KA, Deal AM, Williams GR, Guerard EJ, Pergolotti M, Muss HB (2016) Physical activity communication between oncology providers and patients with early-stage breast, colon, or prostate cancer. Cancer 122(3):470–476. https://doi.org/10.1002/cncr.29786
Kenzik K, Pisu M, Fouad MN, Martin MY (2016) Are long-term cancer survivors and physicians discussing health promotion and healthy behaviors? J Cancer Surviv 10(2):271–279. https://doi.org/10.1007/s11764-015-0473-8
Karvinen KH, DuBose KD, Carney B, Allison RR (2010) Promotion of physical activity among oncologists in the United States. J Support Oncol 8(1):35–41. https://doi.org/10.1097/NCC.0b013e31822d9081
Park J-H, Oh M, Yoon YJ, Lee CW, Jones LW, Kim SI, Kim NK, Jeon JY (2015) Characteristics of attitude and recommendation of oncologists toward exercise in South Korea: a cross sectional survey study. BMC Cancer 15(1):249. https://doi.org/10.1186/s12885-015-1250-9
Spellman C, Craike M, Livingston P (2013) Knowledge, attitudes and practices of clinicians in promoting physical activity to prostate cancer survivors. Health Educ J 73(5):566–575. https://doi.org/10.1177/0017896913508395
Karvinen K, McGourty S, Parent T, Walker PR (2012) Physical activity promotion among oncology nurses. Cancer Nurs 35(3):41–48. https://doi.org/10.1097/NCC.0b013e31822d9081
O’Hanlon É, Kennedy N (2014) Exercise in cancer care in Ireland: a survey of oncology nurses and physiotherapists. Eur J Cancer Care (Engl) 23(5):630–639. https://doi.org/10.1111/ecc.12206
Williams K, Beeken RJ, Fisher A, Wardle J (2015) Health professionals’ provision of lifestyle advice in the oncology context in the United Kingdom. Eur J Cancer Care (Engl) 24(4):522–530. https://doi.org/10.1111/ecc.12305
Jones LW, Courneya KS, Peddle C, Mackey JR (2005) Oncologists’ opinions towards recommending exercise to patients with cancer: a Canadian national survey. Support Care Cancer 13(11):929–937. https://doi.org/10.1007/s00520-005-0805-8
Smith-Turchyn J, Richardson J, Tozer R, McNeely M, Thabane L (2016) Physical activity and breast cancer: a qualitative study on the barriers to and facilitators of exercise promotion from the perspective of health care professionals. Physiother Can 68(4):383–390. https://doi.org/10.3138/ptc.2015-84
Haussmann A, Gabrian M, Ungar N, Jooß S, Wiskemann J, Sieverding M, Steindorf K (2018) What hinders healthcare professionals in promoting physical activity towards cancer patients? The influencing role of healthcare professionals’ concerns, perceived patient characteristics, and perceived structural factors. Eur J Cancer Care (Engl). https://doi.org/10.1111/ecc.12853
Ewing JC (2015) Roles played by advanced practitioners in oncology: present status and future outlook. Clin J Oncol Nurs 19(2):226–227. https://doi.org/10.1188/15.cjon.226-227
Fisher MD, Punekar R, Yim YM, Small A, Singer JR, Schukman J, McAneny BL, Luthra R, Malin J (2017) Differences in health care use and costs among patients with cancer receiving intravenous chemotherapy in physician offices versus in hospital outpatient settings. J Oncol Pract 13(1):e37–e46. https://doi.org/10.1200/jop.2016.012930
Shi L, Lebrun LA, Hung L-M, Zhu J, Tsai J (2012) US primary care delivery after the health center growth initiative: Comparison of health centers, hospital outpatient departments, and physicians’ offices. J Ambul Care Manage 35(1):60–74. https://doi.org/10.1097/JAC.0b013e31823abf07
Ajzen I (2002) Constructing a TpB-questionnaire: conceptual and methodological considerations. http://chuang.epage.au.edu.tw/ezfiles/168/1168/attach/20/pta_41176_7688352_57138.pdf. Accessed 9 April 2018
Francis JJ, Eccles MP, Johnston M, Walker A, Grimshaw J, Foy R, Kaner EF, Smith L, Bonetti D (2004) Constructing questionnaires based on the theory of planned behaviour. A manual for health services researchers. http://openaccess.city.ac.uk/1735. Accessed 5 April 2018
Ajzen I (1991) The theory of planned behavior. Organ Behav Hum Decis Process 50(2):179–211. https://doi.org/10.1016/0749-5978(91)90020-T
Spittaels H, Foster C, Oppert J-M, Rutter H, Oja P, Sjöström M, De Bourdeaudhuij I (2009) Assessment of environmental correlates of physical activity: development of a European questionnaire. Int J Behav Nutr Phys Act 6(1):39. https://doi.org/10.1186/1479-5868-6-39
Sieverding M, Decker S, Zimmermann F (2010) Information about low participation in cancer screening demotivates other people. Psychol Sci 21(7):941–943. https://doi.org/10.1177/0956797610373936
Wiskemann J, Lauer H, Wohland-Braun B (2016) Sport, Bewegung und Krebs. Krebsverband Baden-Wuerttemberg e.V., Nationales Centrum für Tumorerkrankungen Heidelberg. https://www.nct-heidelberg.de/fileadmin/media/fuer_patienten/beratung/bewegung/OnkoAktiv/0706_Sport_und_Krebs_web.pdf [also available in English: https://www.nct-heidelberg.de/en/for-patients/counseling-services/physical-activity/network-onkoaktiv.html]. Accessed 6 April 2018
Steindorf K, Schmidt ME, Scharhag-Rosenberger F, Wiskemann J (2014) Supportive Sport- und Bewegungstherapie für onkologische Patienten [English: Supportive exercise therapy for cancer patients]. Onkologie heute 9:41–46
Cohen J (1973) Eta-squared and partial eta-squared in fixed factor ANOVA designs. Educ Psychol Meas 33(1):107–112
Statista (2017) Ärzte in Deutschland. https://de.statista.com/statistik/daten/studie/190309/umfrage/durchschnittsalter-von-vertrags--und-krankenhausaerzten-seit-2000/. Accessed 13 November 2017
Destatis (2015) STATmagazin Datenreport. http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=79492869&nummer=89&p_sprache=D&p_indsp=4051&p_aid=87933691#SOURCES. Accessed 13 November 2017
van Veen MR, Hoedjes M, Versteegen JJ, van de Meulengraaf-Wilhelm N, Kampman E, Beijer S (2017) Improving oncology nurses’ knowledge about nutrition and physical activity for cancer survivors. Oncol Nurs Forum 44(4):488–496. https://doi.org/10.1188/17.onf.488-496
Klemp JR, Frazier LM, Glennon C, Trunecek J, Irwin M (2011) Improving cancer survivorship care: oncology nurses’ educational needs and preferred methods of learning. J Cancer Educ 26(2):234–242. https://doi.org/10.1007/s13187-011-0193-3
Karvinen KH, Balneaves L, Courneya KS, Perry B, Truant T, Vallance J (2017) Evaluation of online learning modules for improving physical activity counseling skills, practices, and knowledge of oncology nurses. Oncol Nurs Forum 44(6):729–738. https://doi.org/10.1188/17.onf.729-738
Nadler M, Bainbridge D, Tomasone J, Cheifetz O, Juergens RA, Sussman J (2017) Oncology care provider perspectives on exercise promotion in people with cancer: an examination of knowledge, practices, barriers, and facilitators. Support Care Cancer 25(7):2297–2304. https://doi.org/10.1007/s00520-017-3640-9
Little P, Roberts L, Blowers H, Garwood J, Cantrell T, Langridge J, Chapman J (2001) Should we give detailed advice and information booklets to patients with back pain? A randomized controlled factorial trial of a self-management booklet and doctor advice to take exercise for back pain. Spine 26(19):2065–2072. https://doi.org/10.1097/00007632-200110010-00003
Simmons KR, Sinning MA, Pearson JA, Hendrix C (2013) Implementing a home-based exercise prescription for older patients with peripheral arterial disease and intermittent claudication: a quality improvement project. J Vasc Nurs 31(1):2–8. https://doi.org/10.1016/j.jvn.2012.06.005
Park J-H, Lee J, Oh M, Park H, Chae J, Kim D-I, Lee MK, Yoon YJ, Lee CW, Park S, Jones LW, Kim NK, Kim SI, Jeon JY (2015) The effect of oncologists’ exercise recommendations on the level of exercise and quality of life in survivors of breast and colorectal cancer: a randomized controlled trial. Cancer 121(16):2740–2748. https://doi.org/10.1002/cncr.29400
Vallance JK, Courneya KS, Plotnikoff RC, Yasui Y, Mackey JR (2007) Randomized controlled trial of the effects of print materials and step pedometers on physical activity and quality of life in breast cancer survivors. J Clin Oncol 25(17):2352–2359. https://doi.org/10.1200/jco.2006.07.9988
Acknowledgements
We thank Anastasia Penner, Fiona Rupprecht, Sophie Scherer, and Kim Alice Schouten for their help in the recruitment, coding procedure, and data management.
Funding
This study was part of the Momentum Project that has been supported by a grant from the German Cancer Aid (Grant Nos. 110512, 110551, and 111223).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study received ethical approval by the ethics commission of the Faculty of Behavioral and Cultural Studies of the University of Heidelberg. The authors declare that they have full control of all primary data and that they agree to allow the journal to review their data.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Haussmann, A., Ungar, N., Gabrian, M. et al. Are healthcare professionals being left in the lurch? The role of structural barriers and information resources to promote physical activity to cancer patients. Support Care Cancer 26, 4087–4096 (2018). https://doi.org/10.1007/s00520-018-4279-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4279-x