Abstract
Purpose
Oxaliplatin, an important chemotherapeutic agent in colorectal cancer, causes chemotherapy-induced peripheral neuropathy (CIPN), for which prophylactic or therapeutic interventions are lacking. We aimed to investigate changes in upper extremities, activities of daily living (ADL), and health-related quality of life (HRQoL) parameters after the first chemotherapy cycle.
Methods
Thirty-eight colorectal cancer patients scheduled to receive the leucovorin, 5′-fluorouracil, oxaliplatin (FOLFOX) therapy or the capecitabine, oxaliplatin (CAPOX) therapy, participated. Patients underwent objective assessment of sensory function, muscular strength, and manual dexterity and answered the European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire C30 (EORTC QLQ-C30) and the Disabilities of the Arm, Shoulder, and Hand-Disability/Symptom (DASH-DS) questionnaires for subjective assessment. The CIPN was assessed at baseline and prior to the second drug cycle.
Results
Light touch sensation in both hands worsened significantly after the first drug cycle, though no significant changes were observed in muscular strength and manual dexterity. The QLQ-C30 analysis showed that Physical Functioning, Role Functioning, Nausea and Vomiting, and Dyspnea were significantly worse, whereas Emotional Functioning was improved. The DASH-DS analysis revealed significant worsening of dysfunction and subjective symptoms.
Conclusions
Our results suggest that light touch sensation may worsen even in the absence of multiple chemotherapy cycles. Even if arm and hand function (muscular strength and manual dexterity) is apparently intact, patients may experience dysfunction and decreased HRQoL. For preserving or improving patients’ ADL and HRQoL, it is imperative to provide support at chemotherapy initiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The recent development of multidisciplinary therapy has led to improved survival and reduced relapse in cancer patients. However, chemotherapy side effects may decrease patient health-related quality of life (HRQoL), with serious clinical implications, such as the need for dose reduction, treatment delays, or treatment discontinuation [1].
Oxaliplatin (L-OHP), an important chemotherapeutic agent in colorectal cancer, causes acute and chronic chemotherapy-induced peripheral neuropathy (CIPN). Chronic CIPN leads to dose-limiting toxicity [2, 3], and a cumulative dose ≥ 540–850 mg/m2 increases risk of subjective symptoms such as numbness, and that of functional disorders which may affect patient activities of daily living (ADL) [2,3,4,5,6]. Patients often experience CIPN symptoms in their fingers [7], which can interfere with ADL and HRQoL [8,9,10,11]. However, there is no standardized effective therapy for prevention and treatment of CIPN [12,13,14,15,16,17,18]. Commonly used measures of CIPN include the National Cancer Institute Common Terminology Criteria (NCI-CTCAE) v4.0, and physician-based instruments [19]. However, CIPN symptoms are largely subjective, and the lack of a universally recognized standard for quantifying CIPN symptoms [17, 20,21,22] makes it difficult to capture changes in sensory function, ADL, and HRQoL, in detail [23,24,25]. Chronic platinum-induced neuropathy is believed to manifest as secondary axonal degeneration or axonal damage accompanying dorsal root ganglion neuronopathy [26,27,28]. Although L-OHP-induced neuropathy is sensory rather than motor in nature, the intensity of dysfunction can impair physical functions, resulting in symptoms such as sensory ataxia [1].
The negative influence of CIPN on upper extremity function, ADL, and HRQoL can be detected only in advanced stages of dysfunction. Once CIPN symptoms occur, they usually persist for a year or more after treatment termination [29,30,31]. In severe cases, sensory nerve fiber damage may become irreversible [16]. Therefore, it is important that interventions or self-care strategies are offered to patients prior to the appearance of obvious CIPN symptoms.
We aimed to investigate changes in chronic sensory neuropathy, manual dexterity, ADL, and HRQoL after the first cycle of L-OHP-based chemotherapy in colorectal cancer patients who were scheduled to receive initial chemotherapy. We focused on the period after the first chemotherapy cycle when CIPN symptoms were expected to be milder, rather than during the period when the cumulative L-OHP dose was 540–850 mg/m2 or higher, when functional disorders caused by chronic CIPN are likely to appear.
Methods
Study design and participants
We conducted a prospective single-center observational study, approved by the Kyoto University Graduate School and Faculty of Medicine, Ethics Committee (E1571). Colorectal cancer patients scheduled to receive initial chemotherapy with the leucovorin, 5′-fluorouracil, oxaliplatin (FOLFOX) or the capecitabine, oxaliplatin (CAPOX) therapy at the Kyoto University Hospital were surveyed.
Study eligibility criteria included (a) diagnosis of colorectal cancer, (b) scheduled FOLFOX or CAPOX therapy, (c) ability to fill a questionnaire, and (d) written informed consent provided. Study exclusion criteria were (a) pre-existing neuropathic disease (peripheral neuropathy and/or a disease of the central nervous system), (b) prior chemotherapy, and (c) unsuitability as deemed by the researchers and/or the attending physician.
Procedures
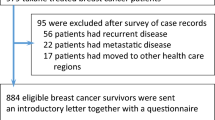
The CIPN measurements were collected before initiation of the first chemotherapy cycle (baseline) and again before start of the second drug cycle, to investigate changes in chronic sensory neuropathy, manual dexterity, ADL, and HRQoL after the first chemotherapy cycle. Following that, CIPN measurements were collected 2 or 3 weeks after baseline just before the second drug cycle depending on the regimen, because FOLFOX therapy was administered every 2 weeks and CAPOX therapy was administered every 3 weeks (Fig. 1).
Measures
Objective assessments
Sensory evaluation was performed by light touch sensation, moving two-point discrimination (m2PD), and proprioceptive sensation assessments. Motor function was evaluated by manual dexterity, grip strength, and pinch strength tests.
Evaluation of sensory function
Evaluation of light touch sensation
We employed the widely used Semmes-Weinstein monofilament test (SWMT) (2.83, 3.22, 3.61, 4.31, 4.56, and 6.65 mg monofilaments) (Aesthesio®, Precise Tactile Sensory Evaluator), to evaluate light touch sensation [32]. The evaluation was conducted according to the operation manual [33] by an experienced occupational therapist. The testing procedure was explained to the patients, and they were instructed to respond verbally by saying “touch” or “yes” when a stimulus was felt. Subsequently, in a quiet area conducive to minimize distractions, two evaluations were performed under similar conditions. Light touch sensation was assessed in the right and left index finger pad (a half beyond the distal interphalangeal joint). Perception levels were interpreted based on the monofilament labels as follows: 2.83 (normal), 3.22 or 3.61 (diminished light touch), 4.31 (diminished protective sensation), 4.56 or 6.65 (loss of protective sensation), and 6.65 undetected (nonmeasurable).
Moving two-point discrimination test [34, 35]
Pressure perception of right and left index fingers was evaluated using a two-point discriminator. One or two points of the discriminator were vertically pressed onto the long axis of the finger pad until it bent slightly, were held for about 2 s, and then slowly moved distally to the fingertip. The subject was asked whether he/she was being touched at one point or at two points. Testing began with 5-mm spacing between discriminator tips, which was narrowed in a stepwise manner. The subject was required to respond to two out of three stimuli before the distance was recorded as the minimum separable distance between two points.
Evaluation of proprioceptive test
The flexion and extension movements of the metacarpophalangeal (MP) joints of the right and left index fingers were repeated ten times passively. A tenth and a half of normal range of motion (ROM) movement was repeated five times each. The subject was asked whether his/her MP joints were being moved to the flexion or extension direction. The number of times the patient answered correctly was recorded as the proprioceptive acuity score.
Evaluation of motor function
Manual dexterity test
We used the Purdue Pegboard Test [36] to evaluate manual dexterity. The number of pins a patient could place in the holes of the relevant column using their dominant hand and their nondominant hand in 30 s was recorded as a function of manual dexterity.
Grip strength test
The grip strength of both hands was measured using a Smedley-type digital hand dynamometer (TSUTSUMI) in the sitting and the elbow-extended positions.
Pinch strength test
Pinch force between the index finger and thumb of both hands (i.e., pulp pinch strength) was measured. During the pulp pinch strength measurement with a hydraulic pinch gauge (North Coast), the subjects were seated upright with the elbow flexed at a 90° angle.
Subjective assessments
Subjective assessments of the ADL and HRQoL were performed using the Japanese Society for Surgery of the Hand (JSSH) version of the Disabilities of the Arm, Shoulder, and Hand (DASH), and the European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire C30 (EORTC QLQ-C30) version 3.
The DASH disability/symptom (DASH-DS) [37]
The DASH is a patient self-administered questionnaire to assess upper extremity dysfunction and relevant subjective symptoms during the preceding week. The DASH-DS is part of DASH, with 30 items assessing: pain and subjective symptoms (5 items), the degree of difficulty when performing various physical activities (21 items), and the effect of upper extremity dysfunction on social activities (1 item), on work and daily life (1 item), on sleep (1 item), and the psychological effect on self-image (1 item). Each item is scored on a scale of 1 to 5, for a total score ranging from 0 to 100, calculated as per the DASH-DS scoring manual. Higher scores indicate higher severity. In this study, the total score was calculated from 29 items after excluding an item pertaining to sexual function. This information was not obtained since it is not pertinent to upper extremity function, and in addition, would be difficult for the elderly patient group to provide.
EORTC QLQ-C30 (version 3)
The EORTC QLQ-C30 (version 3) (QLQ-C30) is a 30-item patient self-administered questionnaire assessing HRQoL [38], with a global health status/QOL (global QOL) scale, 5 functional scales (physical functioning, role functioning, emotional functioning, cognitive functioning, and social functioning), and 9 symptom scales (fatigue, nausea and vomiting, pain, dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial difficulties). The QOL scores were calculated as per the EORTC Scoring Manual. Higher scores on the global QOL scale and the functional scale indicate favorable conditions. Conversely, higher scores on the symptom scale indicate poor conditions.
Statistical analyses
Scores from the Purdue Pegboard Test, grip strength test, and the pinch strength test were compared using paired t tests. Scores obtained from the Semmes-Weinstein monofilament test, m2PD test, DASH-DS, and the QLQ-C30 were compared using the Wilcoxon signed rank test. All statistical analyses were performed using the IBM SPSS, ver. 20 software (International Business Machines Corporation, Armonk, NY). A p value < 0.05 (two-tailed test) was considered statistically significant.
Results
Forty-eight colorectal cancer patients scheduled to receive initial FOLFOX/CAPOX therapy at the Kyoto University Hospital who provided informed consent and were enrolled between November 2012 and June 2014. Ten patients were excluded due to the following reasons: chemotherapy discontinued during the assessment period (3), poor health conditions (3), prior history of peripheral neuropathy or upper extremity disorders (2); difficulty in baseline assessment (1), and difficulty in assessment due to time constraints (1). Thirty-eight patients who satisfied study eligibility criteria were included in this study (Table 1).
Patient characteristics
Thirty-eight patients (22 men, 16 women) were included in the study (median age 65 years; range 33–76 years). All patients were right-handed and received either the FOLFOX (n = 19) or the CAPOX therapy (n = 19).
Objective assessments
All patients provided data for all items at baseline. However, one patient did not provide data for the manual dexterity, grip strength, or the pinch strength tests prior to the second drug cycle due to malaise, pain, or other unfavorable health conditions. Thus, the sample size differed by time point.
Evaluation of sensory function
Semmes-Weinstein monofilament test
There was a significant difference in the median SWMT readings for the right index finger at baseline (2.83 mg), and those prior to the second drug cycle (3.61 mg) (p = 0.000, Table 2(a)). Likewise, the median reading for the left index finger at baseline was 2.83 mg, while that prior to the second drug cycle was 2.83 mg, which were also significantly different (p = 0.009).
Moving two-point discrimination test
There was no statistically significant change between m2PD test values at baseline and those prior to the second drug cycle (Table 2(b)).
Proprioceptive test
There was no statistically significant change between proprioceptive test results at baseline and those prior to the second drug cycle (Table 2(c)).
Evaluation of motor function
Manual dexterity test
There was no significant change in manual dexterity test values at baseline and those prior to the second drug cycle (Table 3(a)).
Grip strength test
There was no significant difference between mean values for the right hand at baseline (28.3 ± 9.2 kg) and those prior to the second drug cycle (28.0 ± 8.7 kg). Likewise, the mean value for the left hand at baseline was 26.6 ± 9.1 kg, while that prior to the second drug cycle was 26.2 ± 8.6 kg, and this change was not statistically significant (Table 3(b)). In addition, 36/37 patients (97.3%) had lower mean grip strength at any time compared to that of age- and gender-matched individuals as per the FY2014 Survey on Physical Fitness and Motor Abilities conducted by the Ministry of Education, Culture, Sports, Science and Technology [39].
Pinch strength test
No significant changes in pinch strength test results were observed between the two time points (Table 3(c)).
Subjective assessments
DASH-DS
The median DASH-DS score at baseline was 2.6, while that prior to the second drug cycle was 5.2, showing significant worsening of dysfunction and subjective symptoms (p = 0.007) (Table 4). There was a significant difference between median scores for pain and subjective symptoms at baseline (median score 5), and that prior to the second drug cycle (median score 6) (p = 0.036).
QLQ-C30
The scores for each QLQ-C30 scale were compared between baseline and prior to the second drug cycle (Table 5). There were no significant changes in the scores on the global health status/QOL scale. However, physical functioning (p = 0.049) and role functioning (p = 0.014) significantly worsened. However, emotional functioning improved significantly (p = 0.003). Cognitive functioning and social functioning did not change significantly. Nausea and vomiting (p = 0.045) and dyspnea (p = 0.020) significantly worsened. There were no significant changes in fatigue, pain, insomnia, appetite loss, constipation, diarrhea, and financial difficulties.
Discussion
This study examined the changes in sensory dysfunction, manual dexterity, ADL, and HRQoL after the first chemotherapy drug cycle in colorectal cancer patients from both objective and subjective points of view, by combining six assessment tools on upper extremity function and two subjective assessment tools on ADL and HRQoL.
In this study, light touch sensation worsened after the first drug cycle, but neither m2PD nor proprioception showed clear worsening. The light touch sensation receptor is a slow-adapting mechanoreceptor that affects grip force adjustment ability such as while continuously holding an object without squashing or dropping it. On the other hand, the m2PD receptor is a quick-adapting mechanoreceptor that affects the identification of materials and dexterity. Thus, our results imply that slow-adapting mechanoreceptors are more likely to be damaged than are quick-adapting mechanoreceptors, during low total dose of chemotherapy. Thus, manual dexterity, dependent on quick-adapting mechanoreceptors did not worsen, while light touch sensation, a function of slow-adapting mechanoreceptors worsened, in our study. However, studies suggest that sensory ataxia may occur as symptoms become severe [1]. Thus, as the total L-OHP dose increases, both the slow and the quick-adapting mechanoreceptors may be damaged. Therefore, continuous assessments of sensory function and manual dexterity are indicated. The significant change in the SWMT median for the right hand (2.83 vs. 3.61 mg) suggests clinically relevant dysfunction because the perception level changes from “normal” to “diminished light touch.” However, the median left hand scores at baseline and at follow-up were similar, implying absence of clinically relevant dysfunction. The 75th percentile of SWMT scores before the second course of chemotherapy was 3.61 mg. These results indicate that an increase in patients with diminished light touch in the left hand as well. We cannot ascertain if this left hand dysfunction is clinically relevant based on these results alone, so there is a need to investigate the correlation between these results and everyday life as a topic for future research.
L-OHP-induced peripheral neuropathy symptoms are not considered to be due to motor neuropathy [40]. This is consistent with the findings of this study which indicated that motor function did not worsen after one cycle of chemotherapy. On the other hand, the mean grip strength test score in 97.3% of patients was lower than that in age- and gender-matched subjects according to the FY2014 Survey on Physical Fitness and Motor Abilities [39], suggesting a lower muscle strength in colorectal cancer patients receiving chemotherapy. There were 12 patients receiving neoadjuvant therapy (31.6%), 15 patients receiving adjuvant therapy (39.5%), and 11 patients receiving palliative therapy (28.9%) in this study. In 52.6% of patients with advanced stage IV disease with distant metastasis, there was a risk of reduced physical function due to disease progression in addition to that due to chemotherapy side effects. Because this study examined changes in chronic sensory dysfunction, manual dexterity, ADL, and HRQoL after the first chemotherapy cycle, objective assessment tools specialized for upper extremity function were selected. While we were unable to objectively evaluate the possible effect of deterioration of general patient condition on test results, it is unlikely that disease progression or rapid deterioration of the general condition of patients had an effect on test scores because: only patients receiving chemotherapy for the first time were studied; included patients were deemed testable by a doctor; the second evaluation time point was 2–3 weeks after the first (thus still being in the initial stage of chemotherapy); and data from patients who were unable to be evaluated a second time were not included in this study. However, DASH-DS and QLQ-C30 used to assess ADL and HRQoL are not specialized for the assessment of CIPN symptoms, and reduced physical function can affect the scores, so these results need to be interpreted with caution.
The objective assessment results did not reveal worsening of upper extremity function, except in the case of light touch sensation. This implied that no causative dysfunction was detected after the first drug cycle, which might affect ADL. On the other hand, DASH-DS, a subjective assessment tool, showed dysfunction and worsening of subjective symptoms after the first drug cycle. Thus, the standard clinical assessment tools for upper extremity function showed that chemotherapy can adversely affect daily life activities and cause worsening of subjective symptoms in cancer patients receiving chemotherapy even at a stage where compromised muscle strength or upper extremity dysfunction are not likely. This indicates that it is necessary to support cancer patients on chemotherapy from the most initial stages, even in the absence of any apparent dysfunction. It is important to note that, to provide individualized support while accommodating unique symptoms and backgrounds during treatment, care should be taken even during the initial stages of treatment. Additionally, patients may have decreased sensory perception post-chemotherapy initiation, so it is also necessary to focus on patient education and providing guidance for daily living, early on.
According to the EORTC QLQ-C30 scoring manual [41], patients who reported “a little” change for better or worse on a particular scale (function or symptom) had QLQ-C30 changes of about 5 to 10. The changes in means for role functioning, emotional functioning, and dyspnea suggest minimal changes clinically. The QLQ-C30 assessment revealed that emotional functioning significantly improved while physical functioning and role functioning significantly worsened after the first drug cycle. According to a HRQoL study conducted 1 year post-surgery in colorectal cancer patients who did not undergo chemotherapy, emotional functioning significantly improved 2 months post-surgery, compared with that pre-surgery [42]. These results are consistent with the findings of the present study which showed improved emotional functioning after the first drug cycle. However, since patients on post-operative adjuvant therapy as well as those on pre-operative neoadjuvant therapy or mitigation therapy were included in the current study, these results cannot be compared with previously published results. Previous studies [42] have not reported worsening of physical functioning or role functioning after the first cycle of chemotherapy. Thus, worsening of physical and role functioning may be due to changes in HRQoL at the early stages of chemotherapy. Role functioning tools assess the degree of difficulty in work, daily life, hobbies, and leisure but cannot address specific areas of difficulty. So, in the rehabilitation of cancer patients, identifying specific areas of difficulty and offering individualized support may be important.
Although 48 colorectal cancer patients were initially enrolled in this study, ten withdrew due to poor physical condition, and 38 patients were included in the final analysis. Accordingly, the results of this study are based on patients with relatively good systemic conditions, and hence, caution is required while interpreting the results. In addition, in this study, the results show worsening of light touch sensation and subjective symptoms, and changes in scores on the symptom scale and the functional scale. The objective of this study was to determine changes in upper limb function, ADL, and HRQoL after initiating chemotherapy, when the total oxaliplatin dose is still low. It is difficult to determine the long-term prognosis based on this time results alone. While there are functional changes during the initial stage of chemotherapy, it is not clear how this is related to long-term functional disability. This topic will be included in our future research. A possible limitation of the study is that, since multiple statistical comparisons were made with a small sample size, a family-wise error (type I error) may have occurred. It is important to conduct additional large-scale and long-term studies in the future to verify the reliability of this finding.
Conclusions
Our results suggested that light touch sensation may worsen after the first drug cycle even during low total dose chemotherapy. In addition, m2PD and proprioception were maintained, and dysfunction that can affect ADL such as reduced manual dexterity did not occur. However, our results also showed that L-OHP may cause worsening of ADL and HRQoL in patient-subjective assessments. Our results imply that it is necessary to support cancer patients on chemotherapy from the most initial stages, even in absence of any apparent dysfunction.
References
Ewertz M, Qvortrup C, Eckhoff L (2015) Chemotherapy-induced peripheral neuropathy in patients treated with taxanes and platinum derivatives. Acta Oncol 54(5):587–591. https://doi.org/10.3109/0284186X.2014.995775
Cersosimo RJ (2005) Oxaliplatin-associated neuropathy: a review. Ann Phamacother 39(1):128–135. https://doi.org/10.1345/aph.1E319
Pasetto LM, D'Andrea MR, Rossi E, Monfardini S (2006) Oxaliplatin-related neurotoxicity. How and why? Crit Rev Oncol Hematol 59(2):159–168. https://doi.org/10.1016/j.critrevonc.2006.01.001
Cassidy J, Misset JL (2002) Oxaliplatin-related side effects: characteristics and management. Semin Oncol 29(5 Suppl 15):11–20. https://doi.org/10.1053/sonc.2002.35524
Gamelin E, Gamelin L, Bossi L, Quasthoff S (2002) Clinical aspects and molecular basis of oxaliplatin neurotoxicity: current management and development of preventive measures. Semin Oncol 29(5 Suppl 15):21–33. https://doi.org/10.1053/sonc.2002.35525
Grothey A (2003) Oxaliplatin-safety profile: neurotoxicity. Semin Oncol 30:5–13. https://doi.org/10.1016/S0093-7754(03)00399-3
Satomi M, Kono T, Mamiya N, Chisato N, Ebisawa Y, Sugawara M, Saito T, Matsubara K, Kasai S (2009) Survey of oxaliplatin-associated peripheral sensory neuropathy using an interview-based questionnaire in patients with advanced colorectal cancer. Jpn J Cancer Chemother 36:1321–1325
Bakitas MA (2007) Background noise: the experience of chemotherapy-induced peripheral neuropathy. Nurs Res 56(5):323–331. https://doi.org/10.1097/01.NNR.0000289503.22414.79
Mols F, Beijers T, Vreugdenhil G, van de Poll-Franse L (2014) Chemotherapy-induced peripheral neuropathy and its association with quality of life: a systematic review. Support Care Cancer 22(8):2261–2269. https://doi.org/10.1007/s00520-014-2255-7
Markman M (1996) Chemotherapy-associated neurotoxicity: an important side effect-impacting on quality, rather than quantity, of life. J Cancer Res Clin Oncol 122:511–512. https://doi.org/10.1007/BF01213547
Tofthagen C (2010) Surviving chemotherapy for colon cancer and living with the consequences. J Palliat Med 13(11):1389–1391. https://doi.org/10.1089/jpm.2010.0124
Argyriou AA, Polychronopoulos P, Iconomou G, Chroni E, Kalofonos HP (2008) A review on oxaliplatin-induced peripheral nerve damage. Cancer Treat Rev 34(4):368–377. https://doi.org/10.1016/j.ctrv.2008.01.003
Beijers AJ, Jongen JL, Vreugdenhil G (2012) Chemotherapy-induced neurotoxicity: the value of neuroprotective strategies. Neth J Med 70(1):18–25
Grothey A (2005) Clinical management of oxaliplatin-associated neurotoxicity. Clin Colorectal Cancer 5:S38–S46. https://doi.org/10.3816/CCC.2005.s.006
Pachman DR, Barton DL, Watson JC, Loprinz CL (2011) Chemotherapy-induced peripheral neuropathy: prevention and treatment. Clin Pharmacol Ther 90(3):377–387. https://doi.org/10.1038/clpt.2011.115
Wolf S, Barton D, Kottschade L, Grothey A, Loprinzi C (2008) Chemotherapy-induced peripheral neuropathy: prevention and treatment strategies. Eur J Cancer 44(11):1507–1515. https://doi.org/10.1016/j.ejca.2008.04.018
Visovsky C, Collins M, Abbott L, Aschenbrenner J, Hart C (2007) Putting evidence into practice: evidence-based interventions for chemotherapy-induced peripheral neuropathy. Clin J Oncol Nurs 11(6):901–913. https://doi.org/10.1188/07.CJON.901-913
Wilkes G (2007) Peripheral neuropathy related to chemotherapy. Semin Oncol Nurs 23(3):162–173. https://doi.org/10.1016/j.soncn.2007.05.001
National Cancer Institute. Common Terminology Criteria for Adverse Event (NCI-CTCAE): http://ctep.cancer.gov/. Accessed 2 August 2012
Armstrong T, Almadrones L, Gilbert MR (2005) Chemotherapy-induced peripheral neuropathy. Oncol Nurs Forum 32(2):305–311. https://doi.org/10.1188/05.ONF.305-311
Frigeni B, Piatti M, Lanzani F, Alberti P, Villa P, Zanna C, Ceracchi M, Ildebrando M, Cavaletti G (2011) Chemotherapy-induced peripheral neurotoxicity can be misdiagnosed by the National Cancer Institute Common Toxicity scale. J Peripher Nerv Syst 16(3):228–236. https://doi.org/10.1111/j.1529-8027.2011.00351.x
Griffith KA, Merkies IS, Hill EE, Cornblath DR (2010) Measures of chemotherapy-induced peripheral neuropathy: a systematic review of psychometric properties. J Peripher Nerv Syst 15(4):314–325. https://doi.org/10.1111/j.1529-8027.2010.00292.x
Shimozuma K, Ohashi Y, Takeuchi A, Aranishi T, Morita S, Kuroi K, Ohsumi S, Makino H, Mukai H, Katsumata N, Sunada Y, Watanabe T, Hausheer FH (2009) Feasibility and validity of the Patient Neurotoxicity Questionnaire during taxane chemotherapy in a phase III randomized trial in patients with breast cancer: N-SAS BC 02. Support Care Cancer 17(12):1483–1491. https://doi.org/10.1007/s00520-009-0613-7
Sloan JA, Berk L, Roscoe J, Fisch MJ, Shaw EG, Wyatt G, Morrow GR, Dueck AC, National Cancer Institute (2007) Integrating patient-reported outcomes into cancer symptom management clinical trials supported by the National Cancer Institute-sponsored clinical trials networks. J Clin Oncol 25(32):5070–5077. https://doi.org/10.1200/JCO.2007.12.7670
Stephens RJ, Hopwood P, Girling DJ, Machin D (1997) Randomized trials with quality of life endpoints: are doctors’ ratings of patients’ physical symptoms interchangeable with patients’ self-ratings? Qual Life Res 6:225–236. https://doi.org/10.1023/A:1026458604826
Avan A, Postma TJ, Ceresa C, Avan A, Cavaletti G, Giovannetti E, Peters GJ (2015) Platinum-induced neurotoxicity and preventive strategies: past, present, and future. Oncologist 20(4):411–432. https://doi.org/10.1634/theoncologist.2014-0044
Cavaletti G, Alberti P, Frigeni B, Piatti M, Susani E (2011) Chemotherapy-induced neuropathy. Curr Treat Options Neurol 13(2):180–190. https://doi.org/10.1007/s11940-010-0108-3
McWhinney SR, Goldberg RM, McLeod HL (2009) Platinum neurotoxicity pharmacogenetics. Mol Cancer Ther 8(1):10–16. https://doi.org/10.1158/1535-7163.MCT-08-0840
André T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C, Bonetti A, Clingan P, Bridgewater J, Rivera F, de Gramont A (2009) Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 27(19):3109–3116. https://doi.org/10.1200/JCO.2008.20.6771
Beijers AJ, Mols F, Vreugdenhil G (2014) A systematic review on chronic oxaliplatin-induced peripheral neuropathy and the relation with oxaliplatin administration. Support Care Cancer 22(7):1999–2007. https://doi.org/10.1007/s00520-014-2242-z
Park SB, Krishnan AV, Lin CS, Goldstein D, Friedlander M, Kiernan MC (2008) Mechanism underlying chemotherapy-induced neurotoxicity and the potential for neuroprotective strategies. Curr Med Chem 15(29):3081–3094. https://doi.org/10.2174/092986708786848569
Lee JJ, Low JA, Croarkin E, Parks R, Berman AW, Mannan N, Steinberg SM, Swain SM (2006) Changes in neurologic function tests may predict neurotoxicity caused by ixabepilone. J Clin Oncol 24(13):2084–2091. https://doi.org/10.1200/JCO.2005.04.2820
Operation manual. Touch test sensory evaluators. -Semmes Weinstein Von Frey Aesthesiometers-https://www.stoeltingco.com/media/wysiwyg/58011_Touch_Test_Evaluator.pdf. Accessed 31 August 2012
Dellon AL (1978) The moving two-point discrimination test: clinical evaluation of the quickly adapting fiber/receptor system. J Hand Surg Am 3:474–481. https://doi.org/10.1016/S0363-5023(78)80143-9
Kaneko A, Asai N, Kanda T (2005) The influence of age on pressure perception of static and moving two-point discrimination in normal subjects. J Hand Ther 18(4):421–424. https://doi.org/10.1197/j.jht.2005.09.010
Tiffin J, Asher EJ (1948) The Purdue pegboard; norms and studies of reliability and validity. J Appl Psychol 32(3):234–247. https://doi.org/10.1037/h0061266
Imaeda T, Toh S, Nakao Y, Nishida J, Hirata H, Ijichi M, Kohri C, Nagano A, Impairment Evaluation Committee, Japanese Society for Surgery of the Hand (2005) Validation of the Japanese Society for Surgery of the Hand version of the Disability of the Arm, Shoulder, and Hand questionnaire. J Orthop Sci 10(4):353–359. https://doi.org/10.1007/s00776-005-0917-5
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376. https://doi.org/10.1093/jnci/85.5.365
Ministry of Rducation, Culture, Sports, Science & Technology in Japan: http://www.e-stat.go.jp/SG1/estat/List.do?bid=000001054955&cycode=0. Accessed 5 February 2016
Shinozaki E (2010) Chemotherapy-induced peripheral neuropathy: mechanisms and management. Pain Clinic 31:859–867
Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A, on behalf of the EORTC Quality of Life Group (2001) EORTC QLQ-C30 scoring manual (3rd edition). Brussels, Belgium
Tsunoda A, Nakao K, Hiratsuka K, Tsunoda Y, Kusano M (2007) Prospective analysis of quality of life in the first year after colorectal cancer surgery. Acta Oncol 46:77–82. https://doi.org/10.1080/02841860600847053
Acknowledgements
We deeply appreciate patients at Kyoto University Hospital for their contribution to this study. We would like to thank Editage (www.editage.jp) for English language editing.
Funding
This work was partially supported by the Promotion Plan for the Platform of Human Resource Development for Cancer administered by the Ministry of Education, Culture, Sports, Science and Technology in Japan (grant no. 12 to TT). The funder did not have a role in the study design; collection, analysis, or interpretation of the data; the writing of the report; or the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We have full control of all primary data and agree to allow the journal to review these on request.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tabata, A., Kanai, M., Horimatsu, T. et al. Changes in upper extremity function, ADL, and HRQoL in colorectal cancer patients after the first chemotherapy cycle with oxaliplatin: a prospective single-center observational study. Support Care Cancer 26, 2397–2405 (2018). https://doi.org/10.1007/s00520-018-4070-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4070-z