Abstract
Purpose
People with melanoma often report pervasive fears about cancer recurrence, unmet information needs, and difficulties accessing psychological care. Interventions addressing the supportive care needs of people with melanoma are rare, and needs are often overlooked. The study evaluated a newly developed, evidence-based, psycho-educational resource for people with melanoma.
Methods
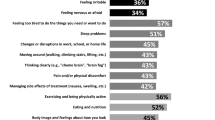
The evaluation study comprised three groups: adults at high risk of new primary disease due to multiple previous melanomas or one melanoma and dysplastic nevus syndrome (DNS), adults at moderate risk due to one previous melanoma and no DNS, and health professionals involved in melanoma care. Participants evaluated a 68-page psycho-educational booklet, Melanoma: Questions and Answers, developed by a multidisciplinary team in accordance with published evidence, clinical guidelines, and intervention development frameworks. The booklet comprised seven modules featuring information on melanoma diagnosis, treatment, prognosis, and ongoing clinical management; risk factors and the role of genetic counseling services for melanoma; psycho-education on emotional, behavioral, and cognitive responses to melanoma, including psycho-education on fear of cancer recurrence; description of healthy coping responses; a suite of tailored tools to support skin self-examination, doctor-patient communication, and identification of the signs and symptoms of anxiety and depression; a list of community-based services and resources; and tools to support melanoma-related record keeping and monitoring. Resource acceptability, relevance, quality, dissemination preferences, emotional responses, unmet information needs, and demographic characteristics were assessed.
Results
Nineteen melanoma survivors (response rate 50 %) and 10 health professionals (response rate 83 %) evaluated the resource. Responses were overwhelmingly positive; the booklet was thoroughly read and highly rated in terms of quality and quantity of information, utility of health education tools, and capacity to address unmet needs. Ninety-five percent of melanoma survivors would recommend the booklet to others. Most preferred a paper-based format, provided by their treating doctor at diagnosis.
Conclusions
Melanoma: Questions and Answers was feasible and acceptable and demonstrated a strong capacity to address the information and psycho-educational needs of people with melanoma at low fiscal cost.

Similar content being viewed by others
References
Australian Institute of Health and Welfare (AIHW) (2015) Australian Cancer Incidence and Mortality (ACIM) books: Melanoma of the skin. Canberra: AIHW. http://www.aihw.gov.au/acim-books
Cancer Australia. Melanoma of the Skin in Australia (2015) http://melanoma.canceraustralia.gov.au/statistics. Accessed January, 2016.
M. Tucker, A. Goldstein (2003) Melanoma etiology: where are we? Oncogene 22:3042–3052
Hayward N (2003) Genetics of melanoma predisposition. Oncogene 22:3053–3062
Whiteman D, Watt P, Purdie D, Hughes M, Hayward N, Green A (2003) Melanocytic nevi, solar keratoses, and divergent pathways to cutaneous melanoma. J Natl Cancer Inst 95(11):806–812
Kefford R, Mann G (2003) Is there a role for genetic testing in patients with melanoma? Curr Opin Oncol 15:157–161
Youlden DR, Youl PH, Soyer HP, Aitken JF, Baade PD (2014) Distribution of subsequent primary invasive melanomas following a first primary invasive or in situ melanoma Queensland, Australia, 1982-2010. JAMA Dermatol 150:526–534
Bradford PT, Freedman DM, Goldstein AM, MA T (2010) Increased risk of second primary cancers after a diagnosis of melanoma. Arch Dermatol 146(3):265–272
Doubrovsky A, Menzies S (2003) Enhanced survival in patients with multiple primary melanoma. Arch Dermatol 139:1013–1018
Sollner W, Zingg-Schir M, Rumpold G, Mairinger G, Fritsch P (1998) Need for supportive counselling—the professionals’ versus the patients’ perspective: a survey in a representative sample of 236 melanoma patients. Psychother Psychosom 67(2):94–104
McLoone J, Watts K, Menzies S, Meiser B, Butow P, Kasparian N (2012) When the risks are high: psychological adjustment among melanoma survivors at high risk of developing new primary disease. Qual Health Res 22(8):1102–1113
Costa DSJ, Dieng M, Cust AE, Butow PN, NA K (2015) Psychometric properties of the fear of cancer recurrence inventory: an item response theory approach. Psycho-Oncol (in press)
Kasparian NA (2013) Psychological care for people with melanoma: what, when, why and how? Semin Oncol Nurs 29(3):214–222
Schofield P, Carey M, Bonevski B, Sanson-Fisher R (2006) Barriers to the provision of evidence-based psychosocial care in oncology. Psycho-Oncol 15(10):863–872
Loquai C, Scheurich V, Syring N, et al. (2013) Screening for distress in routine oncological care: a survey in 520 melanoma patients. PLoS One 8(7):e66800
Australian Cancer Network (2008) Clinical Practice Guidelines for the Management of Melanoma in Australia and New Zealand. Canberra: National Health and Medical Research Council (NHMRC)
Bares CB, Trask PC, Schwartz SM (2002) An exercise in cost-effectiveness analysis: treating emotional distress in melanoma patients. J Clin Psychol Med Settings 9(3):193–200
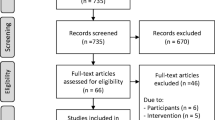
McLoone J, Menzies S, Meiser B, Mann G, Kasparian N (2013) Psycho-educational interventions for people affected by melanoma: a systematic review. Psycho-Oncol 22:1444–1456
Foot G, Sanson-Fisher R (1995) Measuring unmet needs of people living with cancer. Cancer Forum 19(2):131–135
Bonevski B, Sanson-Fisher R, Hersey P, Paul C, Foot G (1999) Assessing the perceived needs of patients attending an outpatient melanoma clinic. J Psychosoc Oncol 17(3–4):101–118
Fallowfield L, Hall A, Maguire P, Baum M, A’Hern R (1994) Psychological effects of being offered choice of surgery for breast cancer. Br Med J 309:448
Brandberg Y, Bergenmar M, Bolund C, Michelson H, et al. (1994) Information to patients with malignant melanoma: a randomized group study. Patient Educ Couns 23(2):97–105
Kasparian NA, McLoone JK, Meiser B, Butow PN, Simpson JM, GJ M (2010) Skin cancer screening behaviours among individuals with a strong family history of malignant melanoma. Br J Cancer 103:1502–1509
McLoone J, Watts K, Menzies S, Barlow-Stewart K, Mann G, Kasparian N (2013) Melanoma survivors at high risk of developing new primary disease: a qualitative examination of the factors that contribute to patient satisfaction with clinical care. Psycho-Oncol 22(9):1994–2000
Medical Research Council. Developing and evaluating complex interventions: new guidance. London: Medical Research Council;2006.
Lazarus R, Folkman S (1984) Stress, appraisal, and coping. Springer, New York
Folkman S (2010) Stress, coping and hope. Psycho-Oncol 19:901–908
National Breast Cancer Centre and National Cancer Control Initiative (2003) Clinical practice guidelines for the psychosocial care of adults with cancer. National Breast Cancer Centre, Camperdown, NSW
National Health and Medical Research Council (2000) How to present the evidence for consumers: preparation of consumer publications. Canberra: Commonwealth of Australia
Dimoska A, Tattersall MH, Butow PN, Shepherd H, Kinnersley P (2008) Can a “prompt list” empower cancer patients to ask relevant questions? Cancer 113(2):225–237
Kasparian N, Butow P, Meiser B, Mann G (2008) High- and average-risk individuals’ beliefs about, and perceptions of, malignant melanoma: an Australian perspective. Psycho-Oncol 17(3):270–279
Australian Bureau of Statistics (2012) Year Book Australia, 2012. Canberra: Australian Bureau of Statistics
O’Connor A (1996) A Cranney User manual: Acceptability. https://decisionaid.ohri.ca/eval_accept.html.
Hodgkinson K, Butow P, Hunt G, et al. (2007) The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: the CaSUN (cancer survivors’ unmet needs measure). Psycho-Oncol 16:796–804
Simard S, Savard J (2009) Fear of cancer recurrence inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer 17(3):241–251
Simard S, Savard J Screening and comorbidity of clinical levels of fear of cancer recurrence. J. Cancer Survivorship (in press)
Zigmond A, Snaith R (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Khoo K, Bolt P, Babl FE, Jury S, Goldman RD (2008) Health information seeking by parents in the internet age. J Paediatr Child Health 44(7–8):419–423
Carlson LE (2016) Mindfulness-based interventions for coping with cancer. Ann N Y Acad Sci (in press)
Janda M, Youl P, Neale R, et al. (2014) Clinical skin examination outcomes after a video-based behavioral intervention: analysis from a randomized clinical trial. JAMA Dermatol 150(4):372–379
Djaja N, Youl P, Aitken J, Janda M (2014) Evaluation of a skin self-examination attitude scale using an item response theory model approach. Health Qual Life Outcomes 12:189
Dieng M, Kasparian NA, Butow PN, et al. (2015) Protocol of a randomised controlled trial of a psycho-educational intervention for melanoma survivors at high risk of developing new primary disease. BMC Psychol 3(1):23
Acknowledgments
Heartfelt thanks to the patients and health professionals who generously gave their time to review earlier versions of the booklet, especially Dr. Elliot Coates, Associate Professor Ross Menzies, Dr. Jordana McLoone, Ms. Heather Reilly, Dr. Pascale Guitera, Ms. Catherine Deans, Dr. Bridget Callaghan, and Dr. Rachael Morton. We also thank Ms. Angela Vangelov for her creative approach to the graphic design of the booklet, CeMPED at The University of Sydney for providing the Question Prompt Sheet that was adapted for the resource, and the Sydney Melanoma Diagnostic Centre at the Royal Prince Alfred Hospital and GenoMEL: the international melanoma genetics consortium, for the provision of images used in the booklet. Nadine Kasparian is supported by a Career Development Fellowship from the National Health and Medical Research Council (NHMRC) of Australia (1049238). Phyllis Butow is supported by an NHMRC Senior Principal Research Fellowship (1022582). Bettina Meiser is supported by an NHMRC Senior Research Fellowship (1078523). This work was also supported by a Project Grant from beyondblue: the national depression initiative (Kasparian) and a Cancer Institute NSW Program Grant for Excellence in Translational Research (Mann, Menzies). Anne Cust is supported by Career Development Fellowships from the NHMRC (1063593) and Cancer Institute NSW (15/CDF/1-14). Mbathio Dieng receives a PhD scholarship through a Cancer Institute NSW Fellowship (Cust) and a Sydney Catalyst Top-Up Research Scholar Award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure of conflicts of interest
None to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Kasparian, N.A., Mireskandari, S., Butow, P.N. et al. “Melanoma: Questions and Answers.” Development and evaluation of a psycho-educational resource for people with a history of melanoma. Support Care Cancer 24, 4849–4859 (2016). https://doi.org/10.1007/s00520-016-3339-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3339-3