Abstract
Purpose
Early detection and improvements in treatment have increased survival after colorectal cancer (CRC), but studies investigating the multidimensional nature of treatment-related symptoms are rare. The aim of this study was therefore to describe the prevalence, frequency, and severity of symptoms and the distress they cause during the early treatment of patients with CRC undergoing chemotherapy.
Methods
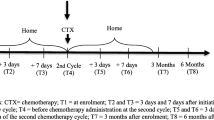
Consecutive outpatients were asked to rate their symptoms during cycle 2 or 3 of chemotherapy, using the Memorial Symptom Assessment Scale.
Results
A total of 104 patients, 58 men and 46 women, evaluated their symptoms of the preceding week at one point during the treatment. The mean number of symptoms was 10.3 (SD, 7.7; range, 0–32). Highly prevalent symptoms were numbness/tingling in the hands/feet (64 %), lack of energy (62 %), feeling drowsy (49 %), and nausea (45 %). Symptoms with the highest scores for frequency, severity, and distress were lack of energy followed by difficulty in sleeping and numbness in the hands/feet. Lack of energy was noted as occurring almost constantly by 26 % and was rated as being severe or very severe by 12 % and as quite distressing or very distressing by 15 %.
Conclusions
This study shows that patients with CRC receiving chemotherapy experience several distressing symptoms early in the treatment phase. In order to provide symptom control, oncology staff should consider evaluating the patient’s symptoms early during treatment and plan adequate measures to minimize the impact of treatment-induced toxicity.



Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61(2):69–90
Labianca R, Beretta GD, Kildani B, Milesi L, Merlin F, Mosconi S, Pessi MA, Prochilo T, Quadri A, Gatta G, de Braud F, Wils J (2010) Colon cancer. Crit Rev Oncol Hematol 74(2):106–133. doi:10.1016/j.critrevonc.2010.01.010
Simpson J, Scholefield JH (2008) Treatment of colorectal cancer: surgery, chemotherapy and radiotherapy. Surg (Oxford) 26(8):329–333
Grenon NN, Chan J (2009) Managing toxicities associated with colorectal cancer chemotherapy and targeted therapy: a new guide for nurses. Clin J Oncol Nurs 13(3):285–296
Holt K (2011) Common side effects and interactions of colorectal cancer therapeutic agents. J Pract Nurs 61(1):7–20
Myers JS (2009) A comparison of the theory of unpleasant symptoms and the conceptual model of chemotherapy-related changes in cognitive function. Oncol Nurs Forum 36(1):E1–E10. doi:10.1188/09.ONF.E1-E10
Naughton M, Homsi J (2002) Symptom assessment in cancer patients. Curr Oncol Rep 4(3):256–263
Stark LL, Tofthagen C, Visovsky C, McMillan SC (2012) The symptom experience of patients with cancer. J Hospice Palliat Nurs 14(1):61–70. doi:10.1097/NJH.0b013e318236de5c
Deshields TL, Potter P, Olsen S, Liu J, Dye L (2011) Documenting the symptom experience of cancer patients. J Support Oncol 9(6):216–223. doi:10.1016/j.suponc.2011.06.003
Cheng KKF, Thompson DR, Ling MW, Chan CWH (2005) Measuring symptom prevalence, severity and distress of cancer survivors. Clin Eff Nurs 9(3–4):154–160
Chou F, Dodd M, Abrams D, Padilla G (2007) Symptoms, self-care, and quality of life of Chinese American patients with cancer. Oncol Nurs Forum 34(6):1162–1167. doi:10.1188/07.onf.1162-1167
Abu-Saad Huijer H, Abboud S (2012) Health-related quality of life among breast cancer patients in Lebanon. Eur J Oncol Nurs. doi:10.1016/j.ejon.2011.11.003
Kamil M, Haron M, Yosuff N, Khalid I, Azman N (2010) High frequency of hand foot syndrome with capecitabine. J Coll Physicians Surg Pak 20(6):421–422
Tofthagen C, McMillan S (2009) Peripheral neuropathy in colon cancer patients receiving oxaliplatin. Oncol Nurs Forum 36(3):70
Lynch BM, Steginga SK, Hawkes AL, Pakenham KI, Dunn J (2008) Describing and predicting psychological distress after colorectal cancer. Cancer 112(6):1363–1370. doi:10.1002/cncr.23300
Kearney N, Miller M, Maguire R, Dolan S, MacDonald R, McLeod J, Maher L, Sinclair L, Norrie J, Wengstrom Y (2008) WISECARE+: results of a European study of a nursing intervention for the management of chemotherapy-related symptoms. Eur J Oncol Nurs 12(5):443–448
World Medical Association (2008) Medical Association Declaration of Helsinki – ethical principles for medical research involving human patients. http://www.wma.net/en/30publications/10policies/b3/. Accessed 1303 2013
Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Kiyasu E, Sobel K, Coyle N, Kemeny N, Norton L et al (1994) The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer 30A(9):1326–1336
Chang VT, Thaler HT, Polyak TA, Kornblith AB, Lepore JM, Portenoy RK (1998) Quality of life and survival: the role of multidimensional symptom assessment. Cancer 83(1):173–179. doi:10.1002/(SICI)1097-0142(19980701)83:1<173::AID-CNCR23>3.0.CO;2-T
Brislin RW (1970) Back-translation for cross-cultural research. J Cross-Cultur Psychol 1:185–216
Acquadro C, Conway K, Giroudet C, Mear I (2012) Linguistic validation manual for health outcome assessments. MAPI Institute, Lyon
Lobchuk MM, Degner LF, Chateau D, Hewitt D (2006) Promoting enhanced patient and family caregiver congruence on lung cancer symptom experiences. Oncol Nurs Forum 33(2):273–282. doi:10.1188/06.onf.273-282
Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Coyle N, Smart-Curley T, Kemeny N, Norton L, Hoskins W et al (1994) Symptom prevalence, characteristics and distress in a cancer population. Qual Life Res 3(3):183–189
Spichiger E, Muller-Frohlich C, Denhaerynck K, Stoll H, Hantikainen V, Dodd M (2011) Prevalence of symptoms, with a focus on fatigue, and changes of symptoms over three months in outpatients receiving cancer chemotherapy. Swiss Med Wkly 141:w13303. doi:10.4414/smw.2011.13303
Rosati G, Rossi A, Tucci A, Pizza C, Manzione L (2001) Phase I study of a weekly schedule of oxaliplatin, high-dose leucovorin, and infusional fluorouracil in pretreated patients with advanced colorectal cancer. Ann Oncol 12(5):669–674
Berg D (2003) Oxaliplatin: a novel platinum analog with activity in colorectal cancer. Oncol Nurs Forum 30(6):957–966
Lam WWT, Law CC, Fu YT, Wong KH, Chang VT, Fielding R (2008) New insights in symptom assessment: the Chinese versions of the Memorial Symptom Assessment Scale Short Form (MSAS-SF) and the Condensed MSAS (CMSAS). J Pain Symptom Manag 36(6):584–595
National Comprensive Cancer Network (2012) NCCN Clinical Practice Guidelines in Oncology. Cancer-Related Fatigue. http://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf. Accessed 10 October 2012
Scott JA, Lasch KE, Barsevick AM, Piault-Louis E (2011) Patients’ experiences with cancer-related fatigue: a review and synthesis of qualitative research. Oncol Nurs Forum 38(3):E191–203. doi:10.1188/11.onf.e191-e203
Butt Z, Rosenbloom SK, Abernethy AP, Beaumont JL, Paul D, Hampton D, Jacobsen PB, Syrjala KL, Von Roenn JH, Cella D (2008) Fatigue is the most important symptom for advanced cancer patients who have had chemotherapy. J Natl Compr Canc Netw 6(5):448–455
Chang VT, Hwang SS, Feuerman M, Kasimis BS, Thaler HT (2000) The memorial symptom assessment scale short form (MSAS-SF). Cancer 89(5):1162–1171
Berger AM, Grem JL, Visovsky C, Marunda HA, Yurkovich JM (2010) Fatigue and other variables during adjuvant chemotherapy for colon and rectal cancer. Oncol Nurs Forum 37(6):E359–369. doi:10.1188/10.onf.e359-e369
Chaiviboontham S, Viwatwongkasem C, Hanucharurnkul S, McCorkle R (2011) Symptom clusters in Thais with advanced cancer. Pac Rim Int J Nurs Res 15(4):265–277
Spichiger E, Müller-Fröhlich C, Denhaerynck K, Stoll H, Hantikainen V, Dodd M (2011) Symptom prevalence and changes of symptoms over ten days in hospitalized patients with advanced cancer: a descriptive study. Eur J Oncol Nurs 15(2):95–102. doi:10.1016/j.ejon.2010.06.005
Kris AE, Dodd MJ (2004) Symptom experience of adult hospitalized medical-surgical patients. J Pain Symptom Manag 28(5):451–459
Di Fabio F, Koller M, Nascimbeni R, Talarico C, Salerni B (2008) Long-term outcome after colorectal cancer resection. Patients’ self-reported quality of life, sexual dysfunction and surgeons’ awareness of patients’ needs. Tumori 94(1):30–35
Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P (2000) The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer 88(1):226–237
Rasmusson EM, Plantin L, Elmerstig E (2013) ‘Did they think I would understand all that on my own?’ A questionnaire study about sexuality with Swedish cancer patients. Eur J Cancer Care 22(3):361–369. doi:10.1111/ecc.12039
Akin S, Can G, Aydiner A, Ozdilli K, Durna Z (2010) Quality of life, symptom experience and distress of lung cancer patients undergoing chemotherapy. Eur J Oncol Nurs 14(5):400–409. doi:10.1016/j.ejon.2010.01.003
Sumdaengrit B, Hanucharurnkul S, Dodd MJ, Wilailak S, Vorapongsathorn T, Pongthavornkamol K (2010) Symptom experience and self-care among Thai women with cervical cancer. Pacific Rim Int J Nurs Res 14(3):203–218
Blinderman CD, Homel P, Billings JA, Tennstedt S, Portenoy RK (2009) Symptom distress and quality of life in patients with advanced chronic obstructive pulmonary disease. J Pain Symptom Manag 38(1):115–123
Zambroski CH, Moser DK, Bhat G, Ziegler C (2005) Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. Eur J Cardiovasc Nurs 4(3):198–206. doi:10.1016/j.ejcnurse.2005.03.010
Strömgren AS, Groenvold M, Pedersen L, Olsen AK, Sjogren P (2002) Symptomatology of cancer patients in palliative care: content validation of self-assessment questionnaires against medical records. Eur J Cancer 38(6):788–794. doi:10.1016/s0959-8049(01)00470-1
Acknowledgments
We thank the research nurses Monica Rösliden and Cecilia Blad for monitoring the data collection in the survey. We also want to thank members of the research team who planned the large project that this study is part of Hans Starkhammar, Susanne Borén, Viktoria Markusson, and Ursula Falkmer. This study was supported by the Medical Research Council of Southeast Sweden and the Division of Nursing Science at the Department of Medical and Health Sciences, Faculty of Health Sciences, Linköping University.
Clinical implications
The results suggest that regular symptom assessment is important even at the beginning of chemotherapy treatment in order to be able to provide effective treatment for symptoms as soon as they occur. In addition, it may be important to include dimensions such as severity and distress as a complement to assessing the frequency of a symptom.
Conflict of interest
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pettersson, G., Berterö, C., Unosson, M. et al. Symptom prevalence, frequency, severity, and distress during chemotherapy for patients with colorectal cancer. Support Care Cancer 22, 1171–1179 (2014). https://doi.org/10.1007/s00520-013-2069-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-2069-z