Abstract
Goals of work
Advanced colorectal cancer (CRC) has recently been treated with monoclonal antibodies, such as cetuximab. Skin toxicity is a peculiar side effect of cetuximab that may induce patients to interrupt therapy if it becomes serious. This study investigates the psychological and social sequelae of skin rash.
Materials and methods
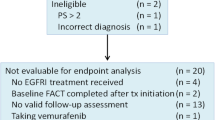
Patients affected by advanced CRC and treated with cetuximab-based therapy entered the trial. The following questionnaires were used: the Functional Assessment of Cancer Therapy—Colorectal (FACT-C) to measure quality of life (QoL) and the Psychological Distress Inventory (PDI). A single item regarding social avoidance was added with a three-point Likert scale. Toxicity was assessed using the National Cancer Institute Criteria (NCI-2).
Main results
Eighty patients were recruited; 41% presented psychological distress. As regards social avoidance, 53% of patients answered that they did not avoid going out at all. The rest of the sample answered that they “very much” (22%) or “somewhat” (25%) avoided going out. Psychological distress and social avoidance were not correlated to skin rash, but only to QoL.
Conclusion
Skin rash was not found to impact patients' psychological status or social life. Two likely explanations for this finding were that (a) patients with advanced cancer consider skin rash as a part of the complex suffering caused by cancer and (b) patients are encouraged by oncologists to continue treatment because skin rash is indicative of response to therapy. This expectation brings hope and helps patients bear the drug-related side effects.
Similar content being viewed by others
References
Agero AL, Dusza SW, Benvenuto-Andrade C et al (2006) Dermatologic side effects associated with the epidermal growth factors receptors inhibitors. J Am Acad Dermatol 55:657–670. doi:10.1016/j.jaad.2005.10.010
Boone SL, Rademaker A, Liu D et al (2007) Impact and management of skin toxicity associated with anti-epidermal growth factor receptor therapy: survey results. Oncology 72:152–159. doi:10.1159/000112795
Bonomi AE, Cella DF, Hahn EA et al (1996) Multilingual translation of the Functional Assessment of Cancer Therapy Quality of Life measurement system. Qual Life Res 5(3):309–320. doi:10.1007/BF00433915
Colucci G, Gebbia V, Paoletti G et al (2005) Phase III randomized trial of FOLFIRI versus FOLFOX in the treatment of advanced colorectal cancer: a multicenter study of the Gruppo Oncologico dell' Italia Meridionale. J Clin Oncol 23(22):4866–4875. doi:10.1200/JCO.2005.07.113
Cunningham D, Humblet Y, Siena S et al (2004) Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan refractory metastatic colorectal cancer. N Engl J Med 351:337–345. doi:10.1056/NEJMoa033025
Dunn J, Lynch B, Aitken J et al (2003) Quality of life and colorectal cancer. A review. Aust N Z J Public Health 27(1):41–53. doi:10.1111/j.1467-842X.2003.tb00378.x
Frieze DA, McCune JS (2006) Current status of cetuximab for the treatment of patient with solid tumors. Ann Pharmacother 40:241–250. doi:10.1345/aph.1G191
Jemal A, Murray T, Ward E et al (2005) Cancer statistics. CA Cancer J Clin 55:10–30. doi:10.3322/canjclin.55.1.10
Karell LH, Christensen AJ, Rosenthal EL et al (2007) Influence of social support on health-related quality of life outcomes in head and neck cancer. Head Neck 29(2):143–146. doi:10.1002/hed.20501
Lemieux J, Maunsell E, Provencher L (2008) Chemotherapy-induced alopecia and effects on quality of life among women with breast cancer: a literature review. Psychooncology 17(4):317–328. doi:10.1002/pon.1245
Lethborg C, Aranda S, Cox S, Kissane D (2007) To what extent does meaning mediate adaptation to cancer? The relationship between physical suffering, meaning in life, and connection to others in adjustment to cancer. Palliat Support Care 5(4):377–388. doi:10.1017/S1478951507000570
McClement SE, Chochinov HM (2008) Hope in advanced cancer patients. Eur J Cancer 44(8):1169–1174. doi:10.1016/j.ejca.2008.02.031
Morasso G, Costantini M, Baracco G et al (1996) Assessing psycological distress in cancer patients: validation of a self administered questionnaire. Oncology 53:295–302
Razavi D, Derlvaux N, Farvacques C et al (1990) Screening for adjustment disorders and major depressive disorders in cancer in-patients. Br J Psychiatry 156:79–83. doi:10.1192/bjp.156.1.79
Rosman S (2004) Cancer and stigma: experience of patients with chemotherapy-induced alopecia. Patient Educ Couns 52:333–339. doi:10.1016/S0738-3991(03)00040-5
Rumsey N, Clarke A, White P (2003) Exploring the psychosocial concerns of outpatients with disfiguring conditions. J Wound Care 12(7):247–252
Schover LR (1991) The impact of breast cancer on sexuality, body image, and intimate relationships. CA Cancer J Clin 41(2):112–120. doi:10.3322/canjclin.41.2.112
Sprangers MA, Taal BG, Aaronson NK et al (1995) Quality of life in colorectal cancer. Stoma vs. nonstoma patients. Dis Colon Rectum 38(4):361–369. doi:10.1007/BF02054222
Sultan S, Fisher DA, Voils CI (2004) Impact of functional support on health related quality of life in patients with colorectal cancer. Cancer 101(12):2737–2743. doi:10.1002/cncr.20699
Tappenden P, Jones R, Paisley S et al (2007) Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer. Health Technol Assess 11(12):1–128 iii–iv
Tournigand C, Andrè T, Achille E et al (2004) FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol 22(2):229–237. doi:10.1200/JCO.2004.05.113
Tversky A, Kahnemann D (1981) The framing of decisions and the psychology of choice. Science 211(4481):453–458. doi:10.1126/science.7455683
Wagner LI (2007) Dermatologic toxicities associated with EGFR inhibitors: the clinical psychologist's perspective. Oncology (Williston Park) 21(11 Suppl 5):34–36
Ward WL, Hahn EA, Mo F et al (1999) Reliability and validity of the Functional Assessment of Cancer Therapy—Colorectal (FACT-C). Qual Life Res 8:181–195. doi:10.1023/A:1008821826499
Wilson KG, Chochinov HM, McPherson CJ et al (2007) Suffering with advanced cancer. J Clin Oncol 25(13):1691–1697. doi:10.1200/JCO.2006.08.6801
Yoo HJ, Kim JC, Eremenco S, Han OS (2004) Quality of life in colorectal cancer patients with colectomy and the validation of the FACT-C version 4. J Pain Symptom Manage 30(1):24–32. doi:10.1016/j.jpainsymman.2004.12.009
Acknowledgments
The authors thank Mr. Baldassarre Stea for his help in the statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors declare that the procedures followed were in accordance with the ethical standards of the Helsinki Declaration (1964, amended in 1975, 1983, 1989, 1996, and 2000) of the World Medical Association.
Appendices
Appendix 1
The FACT-C (Version 4)
PHYSICAL WELL-BEING
I have a lack of energy.
I have nausea.
Because of my physical condition, I have trouble meeting the needs of my family.
I have pain.
I am bothered by side effects of treatment.
I feel ill.
I am forced to spend time in bed.
SOCIAL/FAMILY WELL-BEING
I feel close to my friends.
I get emotional support from my family.
I get support from my friends.
My family has accepted my illness.
I am satisfied with family communication about my illness.
I feel close to my partner (or the person who is my main support).
I am satisfied with my sex life.
EMOTIONAL WELL-BEING
I feel sad.
I am satisfied with how I am coping with my illness.
I am losing hope in the fight against my illness.
I feel nervous.
I worry about dying.
I worry that my condition will get worse.
FUNCTIONAL WELL-BEING
I am able to work (include work at home).
My work (include work at home) is fulfilling.
I am able to enjoy life.
I have accepted my illness.
I am sleeping well.
I am enjoying the things I usually do for fun.
I am content with the quality of my life right now.
ADDITIONAL CONCERNS
I have swelling or cramps in my stomach area.
I am losing weight.
I have control of my bowels.
I can digest my food well.
I have diarrhea.
I have a good appetite.
I like the appearance of my body.
Do you have an ostomy appliance?
If yes, please answer the next two items:
I am embarrassed by my ostomy appliance.
Caring for my ostomy appliance is difficult.
ANSWERS: (0) not at all; (1) a little bit; (2) somewhat; (3) quite a bit; (4) very much.
Appendix 2
The Psychological Distress Inventory (PDI)
In the last week:
-
1.
Do you think your desire to speak with others has diminished?
-
2.
Have you felt calm?
-
3.
Have you experienced moments of anxiety or inner tension?
-
4.
Have you felt tired or lacking in energy?
-
5.
Have you felt more alone?
-
6.
Have you felt better?
-
7.
Have you experienced moments of dejection or depression?
-
8.
Do you think that your illness might have created problems of self-image for you that did not exist before?
-
9.
Have you felt worthless?
-
10.
Have you felt a lack of willpower?
-
11.
Has your interest in the world that surrounds you diminished?
-
12.
Have you felt that your sexual desire has diminished?
-
13.
Has your illness negatively influenced your relationship with others?
ANSWERS: (1) not at all; (2) a little; (3) quite a bit; (4) much; (5) very much.
Rights and permissions
About this article
Cite this article
Romito, F., Giuliani, F., Cormio, C. et al. Psychological effects of cetuximab-induced cutaneous rash in advanced colorectal cancer patients. Support Care Cancer 18, 329–334 (2010). https://doi.org/10.1007/s00520-009-0656-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-009-0656-9