Abstract
Goals of work
Recent literature has indicated the need for rapid evaluation of psychosocial issues secondary to cancer. Because of the problems of routine use of psychometric instruments, short instruments such as visual analogue scales or one-item 0–10 scales have been developed as valid assessment alternatives.
Patients and methods
A study was conducted to examine the role of two 0–10 scales in measuring emotional stress (distress thermometer, DT) and depressed mood (mood thermometer, MT), respectively, in a multicenter study carried out in southern European countries (Italy, Portugal, Spain, and Switzerland). A convenience sample of 312 cancer outpatients completed the DT and MT and the Hospital Anxiety Depression Scale (HADS).
Main results
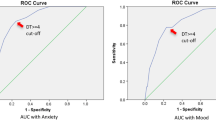
DT was more significantly associated HADS anxiety than HADS depression while MT was related both to HADS anxiety and depression. The correlation of MT with HADS was higher than DT. A cutoff point >4 on the DT maximized sensitivity (65%) and specificity (79%) for general psychosocial morbidity while a cutoff >5 identified more severe “caseness” (sensitivity=70%; specificity=73%). On the MT, sensitivity and specificity for general psychosocial morbidity were 85% and 72% by using the cutoff score >3. A score >4 on the MT was associated with a sensitivity of 78% and a specificity of 77% in detecting more severe caseness.
Conclusions
Two simple instruments, the DT and the MT, were found to have acceptable levels of sensitivity and specificity in detecting psychosocial morbidity. Compared to the HADS, however, the mood MT performed better than the DT.


Similar content being viewed by others
References
van’t Spijker A, Trijsburg RW, Duivenvoorden HJ (1997) Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosom Med 59:280–293
Sollner W, DeVries A, Steixner E, Lukas P, Sprinzl G, Rumpold G, Maislinger S (2001) How successful are oncologists in identifying patient distress, perceived social support, and need for psychosocial counselling? Br J Cancer 84:179–185
Fallowfield L, Ratcliffe D, Jenkins V, Saul J (2001) Psychiatric morbidity and its recognition by doctors in patients with cancer. Br J Cancer 84:1011–1015
Moorey S, Greer S, Watson M, Gorman C, Rowden L, Tunmore R, Robertson B, Bliss J (1991) The factor structure and factor stability of the hospital anxiety and depression scale in patients with cancer. Br J Psychiatry 158:255–259
Carroll B, Kathol R, Noyes R, Wald TG, Clamon GH (1993) Screening for depression and anxiety in cancer patients using the hospital anxiety and depression scale. Gen Hosp Psychiatry 15:69–74
Smith AB, Selby PJ, Velikova G, Stark D, Wright EP, Gould A, Cull A (2002) Factor analysis of the hospital anxiety and depression scale from a large cancer population. Psychol Psychother 75:165–176
Zabora J, Brintzenhofe-Szoc K, Jacobsen P, Curbow B, Piantadosi S, Hooker C, Owens A, Derogatis L (2001) A new psychosocial screening instrument for use with cancer patients. Psychosomatics 42 241–246
Baker F, Denniston M, Zabora J, Polland A, Dudley WN (2002) A POMS short form for cancer patients: psychometric and structural evaluation. Psychooncology 11:273–281
Passik SD, Kirsh KL, Donaghy KB, Theobald DE, Lundberg JC, Holtsclaw E, Dugan WM Jr (2001) An attempt to employ the Zung self-rating depression scale as a “lab test” to trigger follow-up in ambulatory oncology clinics: criterion validity and detection. J Pain Symptom Manage 21:273–281
Liang LP, Dunn SM, Gorman A, Stuart-Harris R (1990) Identifying priorities of psychosocial need in cancer patients. Br J Cancer 62:1000–1003
Maguire P (2002) Improving the recognition of concerns and affective disorders in cancer patients. Ann Oncol 13(Suppl 4):177–181
Maguire P (1999) Improving communication with cancer patients. Eur J Cancer 35:2058–2065
Holland J (2000) An algorithm for rapid assessment and referral of distressed patients. In: Perry CM (ed) American society of clinical oncology educational book. ASCO, Alexandria, pp 129–138
Holland JC, Jacobsen PB, Riba MB (2000) NCCN fever and neutropenia practice guidelines panel. NCCN: distress management. Cancer Control 8(6 Suppl 2):88–93
Holland JC (1997) Preliminary guidelines for the management of distress. Oncology; NCCN Proceedings, November, 11(11A):109–114
Holland JC (1999) Update: NCCN practice guidelines for the management of psychosocial distress. Oncology, NCCN Proceedings, November; 459–507
Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC (1998) Rapid screening for psychological distress in men with prostate carcinoma. Cancer 82:1904–1908
Jacobsen P, Donovan K, Holland JC, Trask P, Fleishman S, Zabora J, Baker F (2004) Multicenter study of the utility of the distress thermometer as a screening instrument in a general cancer population. Psychooncology 13(Suppl 13):42–43
Donovan KA, Jacobsen P, Holland JC, Trask PC, Fleishman S, Zabora J, Baker F (2004) Psychometric properties and correlates of distress thermometer scale. Psychooncology 13(Suppl 13):16
Akizuki N, Akechi T, Nakanishi T, Yoshikawa E, Okamura M, Nakano T, Murakami Y, Uchitomi Y (2003) Development of a brief screening interview for adjustment disorders and major depression in patients with cancer. Cancer 97:2605–2613
Patrick-Miller LJ, Broccoli TL, Levine E, Much JK (2004) Screening for psychosocial distress among ambulatory oncology patients: evaluation of the distress thermometer. Psychooncology 13:S64–S65
Muszbek K, Balogh M, Molnár M, Rohánszky M, Varga K (2004) Screening for distress of Hungarian cancer patients: validation study of Hungarian version of HADS. Psychooncology 13:S63
Grassi L, Rosti G (1996) Psychiatric and psychosocial concomitants of abnormal illness behaviour in patients with cancer. Psychother Psychosom 65:246–252
Gil F, Mendez I, Sirgo A, Llort G, Blanco I, Cortes-Funes H (2003) Perception of breast cancer risk and surveillance behaviours of women with family history of breast cancer: a brief report on a Spanish cohort. Psychooncology 12:821–827
Holland J, Sepulveda C, Zabora J, Katib J, Grassi L, Aikizuki N, Carlsson L (2004) Psychosocial distress—the 6th vital sign: from identification to intervention. Psychooncology 13:S56
Grassi L, Travado L, Gil F, Sabato S, Rossi E, SEPOS Group (2004) Psychosocial morbidity and its correlates in cancer patients of the Mediterranean area: findings from the Southern European Psycho-Oncology Study. J Affect Dis 83:243–248
Travado L, Grassi L, Gil F, Ventura C, Martins C, SEPOS Group (in press) Physician–patient communication among Southern European cancer physicians: the influence of psychosocial orientation and burnout. Psychooncology
Grassi L, Travado L, Gil F, Campos R, Lluch P, Baile W (in press) A communication intervention for training Southern European oncologists to recognize psychosocial morbidity in cancer. I—Development of the model and preliminary results on physicians’ satisfaction. J Cancer Educ
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Karnofsky DA, Burchenal JH (1949) The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM (ed) Evaluation of chemotherapeutic agents. Columbia University Press, New York, pp 191–205
Lynch ME(1995) The assessment and prevalence of affective disorders in advanced cancer patients. J Palliat Care 11:10–18
Zigmond SA, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Ibbotson T, Maguire P, Selby P, Priestman T, Wallace L (1994) Screening for anxiety and depression in cancer patients: the effects of disease and treatment. Eur J Cancer 30:37–40
Razavi D, Delvaux N, Farvacques C, Robaye E, (1990) Screening for adjustment disorders and major depressive disorders in cancer in-patients. Br J Psychiatry 156:79–83
Zweig MH, Campbell G (1993) Receiver-operating characteristics (ROC) plots: a fundamental evaluation in clinical medicine. Clin Chem 39:561–577
Grassi L, Biancosino B, Sabato S, Marmai L, Rossi E, Gil F, Travado L Screening psychiatric morbidity among cancer patients: Italian data from the Southern European Psycho-Oncology Study (SEPOS) (submitted for publication)
Galeazzi GM, Ferrari S, Mackinnon A, Rigatelli M (2004) Interrater reliability, prevalence, and relation to ICD-10 diagnoses of the diagnostic criteria for psychosomatic research in consultation-liaison psychiatry patients. Psychosomatics 45:386–393
Grassi L, Sabato S, Rossi E, Biancosino B, Marmai L (in press) The use of the diagnostic criteria for psychosomatic research (DCPR) in oncology. Psychother Psychosom
Chochinov HM, Wilson KG, Enns M, Lander S (1997)“Are you depressed?” Screening for depression in the terminally ill. Am J Psychiatry 154:674–676
Acknowledgements
The study was funded by the European Community (European Commission DG Health and Consumer Protection—Agreement with the University of Ferrara—SI2.307317 2000CVGG2-026). The research group wish to thank all patients and colleagues for participating in the study and Paul Packer for revising the manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The Southern European Psycho-Oncology Study (SEPOS) Group participating in the project “Improving health staff’s communication and assessment skills of psychosocial morbidity and quality of life in cancer patients: a study of southern European countries,” (principal investigator Luigi Grassi, M.D., University of Ferrara, Italy) was formed by the following persons: Paola Zanotti (CH); Purificación Lluch (E), Maria Francisca Hollenstein (E), Jorge Maté (E), Katia Magnani, Ph.D. (I), Elena Rossi, Ph.D. (I), Silvia Sabato, Ph.D. (I), Giulia Tralli, Ph.D. (I), Cidália Ventura (P); Cristina Martins (P); Sónia Cunha (P); Rute Pires (P).
Rights and permissions
About this article
Cite this article
The SEPOS Group., Gil, F., Grassi, L. et al. Use of distress and depression thermometers to measure psychosocial morbidity among southern European cancer patients. Support Care Cancer 13, 600–606 (2005). https://doi.org/10.1007/s00520-005-0780-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-005-0780-0