Abstract
Immediate type allergic reactions to medication are potentially life threatening and can hamper drug therapy of several medical conditions. Exact incidence and prevalence data for these reactions in children are lacking. If no alternative drug treatment is available, a desensitization procedure may secure the continuation of necessary therapy. Desensitization is only appropriate in case of a strong suspicion of an IgE-mediated allergic reaction. It should be performed by trained clinicians (allergy specialists) in a hospital setting where treatment of a potential anaphylactic reaction can be done without any delay. In this article, literature describing desensitization procedures for several antibiotics, antineoplastic agents, and vaccines in children is reviewed. In general, desensitization schemes for children differ only in final dose from schemes for adults. Contradictory data were found regarding the protective effects of premedication with antihistamines and glucocorticoids.
Similar content being viewed by others
Introduction and definitions
A drug allergy is an adverse drug reaction that results from a specific immunologic response to a medication. Allergic drug reactions account for about 6–10% of all adverse drug reactions, but up to 10% of fatal reactions in the adult population [17]. There are no prevalence data or incidence data for children regarding these allergic drug reactions.
The World Allergy Organization (WAO) has recommended dividing immunologic drug reactions into immediate type I reactions (onset within 1 h of exposure) and delayed reactions (onset after 1 h), based upon the timing of the appearance of symptoms [10]. The signs and symptoms of type I reactions are directly attributable to the vasoactive mediators released by mast cells and basophils. The most common signs and symptoms are urticaria, pruritus, flushing, angioedema (sometimes leading to throat tightness with stridor), wheezing, gastrointestinal symptoms, and hypotension. Anaphylaxis is the most severe presentation of an IgE-mediated drug reaction.
The drugs most commonly implicated in type I reactions in children are beta-lactam drugs, i.e., penicillins and cephalosporins.
Diagnostic procedures in drug allergy are confined to a detailed clinical history and confirmation of an IgE-mediated reaction. The ENDA (European Network for Drug Allergy, an interest group of the EAACI) has set up guidelines on how to perform these tests [4]. In drug allergy, skin tests and in vitro laboratory tests are cumbersome, because the test reagents are not standardized and may even be harmful for a patient with a severe drug reaction. For this reason, the guidelines provide practical skin test methods, test concentrations, and selection of patients. The drug provocation test, the controlled administration of the suspected drug is considered to be the gold standard in order to confirm the diagnosis drug allergy [ENDA, 1].
Desensitization can be considered in patients who are proven (by positive skin testing or in vitro tests) or are strongly suspected to have an IgE-mediated drug allergy and for whom there are no acceptable alternate drugs (see “Practical proposal”). In patients with (multi)resistant bacteria or patients with multiple drug allergies the effect of a desensitization procedure (successful treatment) may outweigh the risks. Desensitization is a procedure which alters the immune response to the drug and results in temporary tolerance, allowing the patient with IgE-mediated allergy to receive a subsequent course of the medication safely. Desensitization should not be attempted in patients with histories of non-IgE-mediated reactions such as Stevens–Johnson syndrome or toxic epidermal necrolysis because even small doses of the drug may induce severe progressive reactions. Desensitization is also not appropriate for patients with type III (IgG-mediated) hypersensitivity drug reactions like hemolytic anemia or nephritis.
Drug desensitization should only be performed by clinicians trained in the technique (usually allergy specialists), in a hospital setting (or outpatient setting under close observation), with intravenous access and necessary medications and equipment to treat anaphylaxis. Pharmacy staff may be consulted prior to the procedure to assist with preparation of the required drug dilutions. Articles concerning protocols are scarce and involve primarily adult patients. In this review, we summarize the known literature concerning pediatric patients who underwent a desensitization procedure.
Review of the literature
For studies describing desensitization procedures in children, PubMed was searched using the combination of keywords “desensitization”, “drug hypersensitivity or drug allergy”, and “child”. The articles found were reviewed for relevance and references were searched where appropriate. Most articles are case reports. Some studies describe case series of adult patients and include one or more children. Very few studies confined to children only were found. This review is limited to desensitization procedures with antibiotics, beta-lactam drugs [8, 22, 23], co-trimoxazole [12, 13, 20], ciprofloxacin [2, 9, 15], cytostatics, carboplatin [5, 14, 18, 19], l-asparaginase [21], and MMR-vaccine [16] in children only.
Procedures
In general, protocols for children differ from those for adults only in the final dose, which should be the daily dose used for adequate therapy.
General principles of desensitization in adult protocols are:
-
Starting doses range from 10% to 0.00001% of the therapeutic dose (mean 0.001%)
-
Administration route orally or intravenously
-
Time interval between two gifts range from 15 to 120 min (mean 30 min)
-
Total duration of desensitization range from 2 h to 21 days (mean 6 h)
-
Increment step range from two times to ten times (mean three times)
Whether premedication with corticosteroids and antihistamines reduces the risk of a desensitization procedure is not known.
Antibiotics
Desensitization procedures are reported to be successful in children with symptoms of an IgE-mediated hypersensitivity reaction like urticaria, angioedema, itch, or anaphylaxis. If reliable skin test procedures are available, such as for beta-lactam antibiotics, these should be performed first. Negative results to intradermal tests with penicilloyl-poly-l-lysine and minor determinant mixture reduce the risk of hypersensitivity symptoms upon re-exposure to less than 5%. In these patients, incremental dosing may be chosen, however, studies comparing this strategy to desensitization with regard to safety and efficacy have not been published.
The starting dose for intravenous procedures is generally 1/1,000,000–1/1,000 of full therapeutic dose, but may be higher (1/100) in oral desensitization [2, 8, 9, 12, 13, 15, 20, 22, 23]. During intravenous desensitization the doses are infused continuously over 15–30 min intervals, followed by intravenous administration of the full therapeutic doses. In the oral procedure, dose intervals described range from 15 min (for ciprofloxacin [15]) to 12 h (for co-trimoxazole [12]). Slow or incomplete absorption from the gastrointestinal tract should be taken into account when choosing this dose interval.
Cytostatics
As cytostatics are usually dosed per square meter, the full therapeutic dose is different for every child. Intravenous desensitization with carboplatin starts at a dose of 0.01–1 mg, infused over 1 min (0.01–1 mg/min). Dose increments are made every 15 min by prolonging the infusion time holding the infusion rate constant. When 15–22.5 mg in 15–22.5 min is well tolerated, the infusion rate is increased to 100 mg/h for 1 h followed by 200 mg/h for the remainder of the dose [5, 18, 19].
l-Asparaginase is administered intramuscularly, but intravenous desensitization had been described starting at a 1 IU dose, doubled every 10 min [21].
Intravenous desensitization for methrotrexate is started at 1/1,000 of the full dose in 1.5 h followed by 1/100 in 1.5 h, 1/10 in 6 h and the remaining dose in 24 h every therapeutic cycle [3, 7]. This procedure may necessitate a dose reduction due to increased toxicity as a result of prolonged exposure to methotrexate [3].
Vaccines
Desensitization to MMR-vaccine is performed by subsequent sc administration of 0.05 ml of a 1/100 dilution, 0.05 ml of a 1/10 dilution, and 0.05 ml of the full strength vaccine up to the 0.5-ml dose [16].
Premedication
Premedication can be done with (methyl)prednisolone, antihistamine, and ranitidine with or without montelukast 13, 7, and 1 h, respectively, before start of the desensitization procedure [18, 19, 21] but the protective effects have not been systematically studied. Administration of a full therapeutic dose in combination with premedication, as an alternative to desensitization, resulted in severe hypersensitivity reactions in three of eight patients reacting to E. coli asparaginase [21]. A recent study in children with carboplatin hypersensitivity reactions suggests that administrating a full dose in combination with premedication may be as effective as desensitization without premedication [14]. However, due to its retrospective nature, it cannot be ruled out that desensitization was preferably initiated in children with more severe hypersensitivity reactions.
Symptoms
In almost 50% of the procedures reviewed in this article, symptoms did occur during the procedure. In general, the symptoms could be treated by antihistamines and dose reduction or postponing dose increase [5, 12, 22, 23].
Effectivity
Success rates in the reports described (mostly IgE-mediated allergy) range from 50% to 100% (see Table 1 for details). However, due to the low number of cases reported and lack of comparative prospective studies, success rate may be either lower or higher in reality. Larger case series in adult patients report a success rate of more than 90% in both allergy to antibiotics and to cytostatics.
Setting
Desensitization in a child with drug allergy should be done by experienced staff with all facilities to treat medical emergencies.
Practical proposal

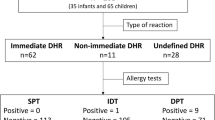
This flowchart is used to decide if desensitization or graded challenge (adapted from Turvey et al. [23]) should be employed.
References
Aberer W, Bircher A, Romano A et al (2003) Drug provocation testing in the diagnosis of drug hypersensitivity reactions: general considerations. Allergy 58:854–863
Bircher AJ, Ritishauser M (1997) Oral desensitization of maculopapular exanthema from ciprofloxacin. Allergy 52:1246–1248
Bouchireb K, Dodille A, Ponvert C et al (2009) Management and successful desensitization in methotrexate-induced anaphylaxis. Pediatr Blood Cancer 52:295–297
Brockow K, Romano A, Blanca M et al (2002) General considerations for skin test procedures in the diagnosis of drug hypersensitivity. Allergy 57:45–51
Broome CB, Schiff RI, Friedman HS (1996) Successful desensitization to carboplatin in patients with systemic hypersensitivity reactions. Med Ped Oncol 26:105–110
Brown LA, Goldberg ND, Shearer WT (1982) Long-term ticarcillin desensitization by the continuous oral administration of penicillin. J Allergy Clin Immunol 69:51–54
Caldeira T, Costa V, Silva I et al (2008) Anaphylactoid reaction to high-dose methotrexate and re-administration after a successful desensitization. Pediatr Hematol Oncol 25:131–134
De Maria C, Lebel D, Desroches A, Gauvin F (2002) Simple intravenous antimicrobial desensitization method for pediatric patients. Am J Health-Syst Pharm 59:1532–1536
Erdem G, Staat MA, Connelly BL, Assa’ad A (1999) Anaphylactic reaction to ciprofloxacin in a toddler: successful desensitization. Ped Inf Dis J 18:563–564
Johansson SGO, Bieber T, Dahl R et al (2004) Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 113:832–836
Kim JH, Kim HB, Kim BS, Hong SJ (2003) Rapid oral desensitization to isoniazid, rifampin, and ethambutol. Allergy 58:540–541
Kletzel M, Beck S, Elser J et al (1991) Trimethoprim-sulfamethoxazole oral desensitization in hemophiliacs infected with human immunodeficiency virus with a history of hypersensitivity reactions. AJDC 145:1428–1429
Kreuz W, Güngör T, Lotz C et al (1990) “Treating through” hypersensitivity to co-trimoxazole in children with HIV infection. Lancet 336:508–509
Lafay-Cousin L, Sung L, Carret AS et al (2007) Carboplatin hypersensitivity reaction in pediatric patients with low-grade glioma: a Canadian Pediatric Brain Tumor consortium experience. Cancer 112:892–899
Lantner RR (1996) Ciprofloxacin desensitization in a patient with cystic fibrosis. J Allergy Clin Immunol 96:1001–1002
Lavi S, Zimmerman B, Koren G, Gold R (1990) Administration of measles, mumps and rubella virus vaccine (live) to egg-allergic children. JAMA 263:269–271
Lazarou J, Pomeranz BH, Corey PN (1998) Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 279:1200–1205
Morgan M, Bowers DC, Gruchalla RS, Khan DA (2004) Safety and efficacy of repeated monthly carboplatin desensitization. J Allerg Clin Immunol 114:974–975
Ogle S, Rose MM, Tate Wildes C (2002) Development and implementation of a carboplatin desensitization protocol for children with neurofibromatosis, type 1 and hypersensitivity reactions in an outpatient oncology clinic. J Pediatr Oncol Nurs 19:122–126
Soffritti S, Ricci G, Prete A et al (2003) Successful desensitization to trimethoprim-sulfamethoxazole after allogeneic haematopoietic stem cell transplantation: preliminary observations. Med Pediatr Oncol 40:271–272
Soyer OU, Aytac S, Tuncer A et al (2009) Alternative algorithm for l-asparaginase allergy in children with acute lymphoblastic leukaemia. J Allergy Clin Immunol 123:895–899
Stark BJ, Earl HS, Gross GN et al (1987) Acute and chronic desensitization of penicillin-allergic patients using oral penicillin. J Allerg Clin Immunol 79:523–532
Turvey SE, Cronin B, Arnold AD, Dioun AF (2004) Antibiotic desensitization for the allergic patient: 5 years of experience and practice. Ann Allergy Asthma Immunol 92:426–432
Conflict of interest
The authors declare that they have no financial relationship with a pharmaceutical company or organization that sponsored the research.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
de Groot, H., Mulder, W.M.C. Clinical practice. Eur J Pediatr 169, 1305–1309 (2010). https://doi.org/10.1007/s00431-010-1236-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-010-1236-1