Abstract
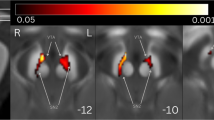
In Parkinson disease (PD), REM sleep behavior disorder (RBD) and depression may occur before the onset of parkinsonism. Transcranial sonography (TCS) shows that hyperechogenicity of the substantia nigra (SN+) and hypoechogenicity of the brainstem raphe (BR+) are frequent in PD, particularly when depression is associated. Combined SN+ and BR+ identify PD subjects in whom depression antedates parkinsonism onset. It can be speculated that SN+ and BR+ may also identify idiopathic RBD (IRBD) subjects with comorbid depression, supporting the clinical diagnosis of this mood disorder. We aimed to study the brainstem raphe and substantia nigra echogenicity and their ability to predict comorbid depression in IRBD. Seventy-two IRBD patients and 71 age and sex-matched controls underwent TCS. Depression was diagnosed by means of DSM-IV criteria. Depression was more frequent in IRBD patients than in controls (44.4 vs. 18.3 %; p = 0.001). BR+ was more frequent in depressed than in nondepressed IRBD patients (32.0 vs. 11.4 %; p = 0.050). Sensitivity of BR+ to predict depression in IRBD was 32.0 %, specificity was 88.6 %, and relative risk was 1.88. Sensitivity of SN+ to predict depression in IRBD was 72.0 %, specificity was 44.1 %, and relative risk was 1.53. Sensitivity of combined BR+ and SN+ to predict depression in IRBD was 23.1 %, specificity 97.1 %, and relative risk was 2.31. Hypoechogenicity of the brainstem raphe, particularly when combined with hyperechogenicity of the substantia nigra, detects comorbid depression in IRBD. This finding suggests that dysfunction of the serotonergic dorsal raphe may be involved in the pathophysiology of depression in IRBD.

Similar content being viewed by others
References
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Tolosa E, Pont-Sunyer C (2011) Progress in defining the premotor phase of Parkinson’s disease. J Neurol Sci 310:4–8
Postuma RB, Aarslnad D, Barone P et al (2012) Identifying prodromal Parkinson’s disease: pre-motor disorders in Parkinson’s disease. Mov Disord 27:617–626
Plomhouse L, Dujarin K, Duhamel A et al (2013) Rapid eye movement sleep behaviour disorder in treatment-naïve Parkinson disease patients. Sleep Med 14:1035–1037
Iranzo A, Santamaria J, Rye DB et al (2005) Characteristics of idiopathic REM sleep behaviour disorder and that associated with MSA and PD. Neurology 65:247–252
Pont-Sunyer C, Hotter A, Gaig C et al (2015) The onset of nonmotor symptoms in Parkinson’s disease (The ONSET PD Study). Mov Disord 30:229–237
Schenck CH, Boeve BF, Mahowald MW (2013) Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behaviour disorder: a 16-year update on a previously reported series. Sleep Med 14:744–748
Iranzo A, Tolosa E, Gelpi E, Molinuevo JL, Valldeoriola F, Serradell M et al (2013) Neurodegenerative disease status and post-mortem pathology in idiopathic rapid-eye-movement sleep behaviour disorder: an observational cohort study. Lancet Neurol 12:443–453
Postuma RB, Gagnon JF, Montplaisir J (2013) Rapid eye movement sleep behaviour disorder as a biomarker for neurodegeneration: the past 10 years. Sleep Med 14:763–767
Nilsson FM, Kessing LV, Bolwig TC (2001) Increased risk of developing Parkinson’s disease for patients with major affective disorder: a register study. Acta Psychiatr Scand 104:380–386
Leentjens AFG, Van den Akker M, Metsemakers JFM, Lousberg R, Verhey FRJ (2003) Higher incidence of depression preceding the onset of Parkinson’s disease: a register study. Mov Disord 18:414–418
Santamaria J, Tolosa E, Valles A (1986) Parkinson’s disease with depression: a possible subgroup of idiopathic parkinsonism. Neurology 36:1130–1133
Barone P, Antonini A, Colosimo C et al (2009) The PRIAMO study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson disease. Mov Disord 24:1641–1649
Berg D, Godau J, Walter U (2008) Transcranial sonography in movement disorders. Lancet Neurol 7:1044–1055
Berg D, Behnke S, Seppi K, Godau J, Lerche S, Mahlknecht P et al (2013) Enlarged hyperechogenic substantia nigra as a risk marker for Parkinson’s disease. Mov Disord 28:216–219
Iranzo A, Stockner H, Serradell M, Seppi K, Valldeoriola F, Frauscher B et al (2014) Five-year follow-up of substantia nigra echogenicity in idiopathic REM sleep behaviour disorder. Mov Disord 29:1774–1780
Walter U, Hoeppner J, Prudente-Morrissey L, Horowski S, Herpertz SC, Benecke R (2007) Parkinson’s disease-like midbrain sonography abnormalities are frequent in depressive disorders. Brain 130:1799–1807
Becker G, Struck M, Bogdahn U, Becker T (1994) Echogenicity of the brainstem raphe in patients with major depression. Psychiatry Res 55:75–84
Becker T, Becker G, Seufert J, Hofmann E, Lange KW, Naumann M et al (1997) Parkinson’s disease and depression: evidence for an alteration of the basal limbic system detected by transcranial sonography. J Neurol Neurosurg Psychiatry 63:590–596
Berg D, Supprian T, Hofmann E, Zeiler B, Jager A, Lange KW et al (1999) Depression in Parkinson’s disease: brainstem midline alteration on transcranial sonography and magnetic resonance imaging. J Neurol 246:1186–1193
Cho JW, Baik JS, Lee MS (2011) Mesencephalic midline change on transcranial sonography in early Parkinson disease patients with depression. J Neurol Sci 310:50–52
Schmidauer C, Sojer M, Seppi K et al (2005) Transcranial ultrasound shows nigral hypoechogenicity in restless legs syndrome. Ann Neurol 58:630–634
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Medicine, Darien
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P et al (2008) Movement disorder society-sponsored revision of the unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23:2129–2170
American Psychiatric Association (1995) Diagnostic and statistical manual of mental disorders 4a. American Psychiatric Association, Washington, DC
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Schrag A, Hosrdfall L, Walters K, Noyce A, Petersen I (2014) Prediagnostic presentations of Parkinson’s disease in primary care: a case-control study. Lancet Neurol 14:57–64
Kessler RC, Birnbaum H, Bromet E et al (2010) Age differences in major depression: results from the National Comorbidity Survey Replication (NCS-R). Psaychol Med 40:225–237
Richards D (2011) Prevalence and clinical course of depression: a review. Clin Psycol Rev 31:117–1125
Grinberg LT, Rueb U, di Lorenzo AT, Heinsen H (2010) Brainstem pathology and non-motor symptoms of PD. J Neurol Sci 289:81–88
Walter U, Skoloduik D, Berg D (2010) Transcranial sonography findings related to non-motor features of Parkinson’s disease. J Neurol Sci 289:123–127
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vilas, D., Iranzo, A., Pont-Sunyer, C. et al. Brainstem raphe and substantia nigra echogenicity in idiopathic REM sleep behavior disorder with comorbid depression. J Neurol 262, 1665–1672 (2015). https://doi.org/10.1007/s00415-015-7745-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7745-0