Abstract
Background
The effectiveness of medication is influenced by treatment adherence. After TIA or minor disabling stroke patients usually are advised to take antithrombotic medication. Stroke patients are an interesting group of patients with respect to adherence, since cardiovascular risk factors and stroke may (indirectly) negatively influence brain function, which can affect adherence. We investigated determinants of non–adherence in patients who used aspirin or oral anticoagulation after cerebral ischaemia of arterial origin.
Methods
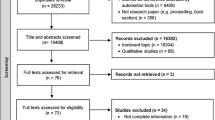
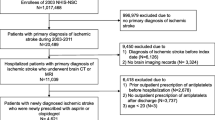
Data of patients prospectively followed in two clinical trials (the Dutch TIA Trial and the Stroke Prevention In Reversible Ischaemia Trial) were analysed with Cox proportional hazards modelling.
Results
In the two trials 3796 patients were treated with aspirin. During a mean follow–up of 2.1 years, 689 patients (18%) prematurely stopped treatment, 305 (8 %) did so without a clear medical reason (non–adherence). Age ≥ 65 years and the use of 300 instead of 30 mg of aspirin were independently associated with non–adherence. Diastolic blood pressure of ≥ 90 mmHg and dizziness were associated with better adherence. Of 651 patients on oral anticoagulation, 143 patients (22 %) stopped after a mean follow–up of 1.0 year, 66 (10 %) did so because of nonadherence. No statistically significant determinants for non–adherence were identified.
Conclusion
As found in the literature on nonadherence in general, age of ≥ 65 years and a higher dose of aspirin (300 mg versus 30 mg) were independently associated with non–adherence with aspirin treatment that was prescribed for secondary prevention after cerebral ischaemia of arterial origin. Older patients may require extra encouragement to continue antithrombotic treatment. Lower doses of aspirin may improve treatment adherence.
Similar content being viewed by others
References
Cleemput I, Kesteloot K (2002) Economic implications of non–compliance in health care. Lancet 359:2129–2130
Donovan JL (1995) Patient decision making. The missing ingredient in compliance research. Int J Technol Assess Health Care 11:443–455
EAFT (European Atrial Fibrillation Trial) Study Group (1993) Secondary prevention in non–rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet 342:1255–1262
Gencheva E, Sloan M, Leurgans S, Raman R, Harris Y, Gorelick P (2004) Attrition and non–compliance in secondary stroke prevention trials. Neuroepidemiology 23:61–66
Hamann GF, Weimar C, Glahn J, Busse O, Diener HC (2003) Adherence to secondary stroke prevention strategies– results from the German Stroke Data Bank. Cerebrovasc Dis 15:282–288
Hillen T, Dundas R, Lawrence E, Stewart JA, Rudd AG, Wolfe CD (2000) Antithrombotic and antihypertensive management 3 months after ischemic stroke: a prospective study in an inner city population. Stroke 31:469–475
Mushlin AI, Appel FA (1977) Diagnosing potential noncompliance. Physicians’ ability in a behavioral dimension of medical care. Arch Intern Med 137:318–321
Rojas–Fernandez CH, Kephart GC, Sketris IS, Kass K (1999) Underuse of acetylsalicylic acid in individuals with myocardial infarction, ischemic heart disease or stroke: data from the 1995 population–based Nova Scotia Health Survey. Can J Cardiol 15:291–296
Sappok T, Faulstich A, Stuckert E, Kruck H, Marx P, Koennecke HC (2001) Compliance with secondary prevention of ischemic stroke: a prospective evaluation. Stroke 32:1884–1889
Schroeder K, Fahey T, Ebrahim S (2004) How can we improve adherence to blood pressure–lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med 164:722–732
Smith NL, Psaty BM, Heckbert SR, Tracy RP, Cornell ES (1999) The reliability of medication inventory methods compared to serum levels of cardiovascular drugs in the elderly. J Clin Epidemiol 52:143–146
Svensson S, Kjellgren KI, Ahlner J, Saljo R (2000) Reasons for adherence with antihypertensive medication. Int J Cardiol 76:157–163
The Dutch TIA Trial Study Group (1991) A comparison of two doses of aspirin (30 mg vs. 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med 325:1261–1266
The Stroke Prevention in Reversible Ischemia Trial (SPIRIT) Study Group (1997) A randomized trial of anticoagulants versus aspirin after cerebral ischemia of presumed arterial origin. Ann Neurol 42:857–865
Vermeire E, Hearnshaw H, Van Royen P, Denekens J (2001) Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther 26:331–342
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
De Schryver, E.L.L.M., van Gijn, J., Kappelle, L.J. et al. Non–adherence to aspirin or oral anticoagulants in secondary prevention after ischaemic stroke. J Neurol 252, 1316–1321 (2005). https://doi.org/10.1007/s00415-005-0858-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-005-0858-0