Abstract
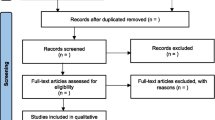
This umbrella review is the first to systematically examine psychological trauma as a transdiagnostic risk factor across psychiatric conditions. We searched Pubmed, Scopus, and PsycNET databases from inception until 01/05/2021 for systematic reviews/meta-analyses evaluating the association between psychological trauma and at least one diagnosed mental disorder. We re-calculated the odds ratio (OR), then classified the association as convincing, highly suggestive, suggestive, or weak, based on the number of cases and controls with and without psychological trauma, random-effects p value, the 95% confidence interval of the largest study, heterogeneity between studies, 95% prediction interval, small-study effect, and excess significance bias. Additional outcomes were the association between specific trauma types and specific mental disorders, and a sensitivity analysis for childhood trauma. Transdiagnosticity was assessed using TRANSD criteria. The review was pre-registered in Prospero CRD42020157308 and followed PRISMA/MOOSE guidelines. Fourteen reviews met inclusion criteria, comprising 16,277 cases and 77,586 controls. Psychological trauma met TRANSD criteria as a transdiagnostic factor across different diagnostic criteria and spectra. There was highly suggestive evidence of an association between psychological trauma at any time-point and any mental disorder (OR = 2.92) and between childhood trauma and any mental disorder (OR = 2.90). Regarding specific trauma types, convincing evidence linked physical abuse (OR = 2.36) and highly suggestive evidence linked sexual abuse (OR = 3.47) with a range of mental disorders, and convincing evidence linked emotional abuse to anxiety disorders (OR = 3.05); there were no data for emotional abuse with other disorders. These findings highlight the importance of preventing early traumatic events and providing trauma-informed care in early intervention and psychiatric services.



Similar content being viewed by others
Data availability
The data that support the findings of this study are openly available in Figshare at https://doi.org/10.6084/m9.figshare.18677786
References
Tyrer P (2015) Mental Illness, Etiology of. International Encyclopedia of the Social & Behavioral Sciences, 2nd edn. Elsevier Inc, Amsterdam, pp 204–208
Huang L, Flatow R, Tenly B, et al (2014) SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS Publication No. (SMA) 14–4884. Subst Abus Ment Heal Serv Adm US Dep Heal Hum Serv 1–27
Varese F, Smeets F, Drukker M et al (2012) Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophr Bull 38:661–671. https://doi.org/10.1093/schbul/sbs050
Frazier PA (2012) Trauma psychology. In Altmaier EM, Hansen J-IC (eds) The Oxford handbook of counselling psychology. Oxford University Press, p 807–836
Friedman MJ, Resick PA, Bryant RA et al (2011) Classification of trauma and stressor-related disorders in DSM-5. Depress Anxiety 28:737–749. https://doi.org/10.1002/da.20845
Green JG, McLaughlin KA, Berglund PA et al (2010) Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry 67:113–123. https://doi.org/10.1001/archgenpsychiatry.2009.186
Hughes K, Bellis MA, Hardcastle KA et al (2017) The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Heal 2:e356–e366. https://doi.org/10.1016/S2468-2667(17)30118-4
McGrath JJ, Saha S, Lim CCW et al (2017) Trauma and psychotic experiences: transnational data from the world mental health survey. Br J Psychiatry 211:373–380. https://doi.org/10.1192/bjp.bp.117.205955
McLaughlin KA, Green JG, Gruber MJ et al (2012) Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry 69:1151–1160. https://doi.org/10.1001/archgenpsychiatry.2011.2277
Copeland WE, Shanahan L, Hinesley J et al (2018) Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2018.4493
Mauritz MW, Goossens PJJ, Draijer N, van Achterberg T (2013) Prevalence of interpersonal trauma exposure and trauma-related disorders in severe mental illness. Eur J Psychotraumatol. https://doi.org/10.3402/ejpt.v4i0.19985
Cuijpers P, Smit F, Unger F et al (2011) The disease burden of childhood adversities in adults: a population-based study. Child Abus Negl 35:937–945. https://doi.org/10.1016/j.chiabu.2011.06.005
Bellis MA, Hughes K, Ford K et al (2019) Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Heal 4:e517–e528. https://doi.org/10.1016/S2468-2667(19)30145-8
Benjet C, Bromet E, Karam EG et al (2016) The epidemiology of traumatic event exposure worldwide: results from the world mental health survey consortium. Psychol Med 46:327–343. https://doi.org/10.1017/S0033291715001981
Kilpatrick DG, Resnick HS, Milanak ME et al (2013) National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress 26:537–547. https://doi.org/10.1002/jts.21848
Kessler RC, McLaughlin KA, Green JG et al (2010) Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br J Psychiatry 197:378–385. https://doi.org/10.1192/bjp.bp.110.080499
Maj M (2005) “Psychiatric comorbidity”: an artefact of current diagnostic systems? Br J Psychiatry 186:182–184. https://doi.org/10.1192/bjp.186.3.182
Dalgleish T, Black M, Johnston D, Bevan A (2020) Transdiagnostic approaches to mental health problems: current status and future directions. J Consult Clin Psychol 88:179. https://doi.org/10.1037/CCP0000482
Nolen-Hoeksema S, Watkins ER (2011) A heuristic for developing transdiagnostic models of psychopathology: explaining multifinality and divergent trajectories. Perspect Psychol Sci 6:589–609. https://doi.org/10.1177/1745691611419672
McLaughlin KA, Colich NL, Rodman AM, Weissman DG (2020) Mechanisms linking childhood trauma exposure and psychopathology: a transdiagnostic model of risk and resilience. BMC Med 18:1–11. https://doi.org/10.1186/s12916-020-01561-6
Fusar-Poli P, Solmi M, Brondino N et al (2019) Transdiagnostic psychiatry: a systematic review. World Psychiatry 18:192–207. https://doi.org/10.1002/wps.20631
Fusar-Poli P (2019) TRANSD recommendations: improving transdiagnostic research in psychiatry. World Psychiatry 18:361–362. https://doi.org/10.1002/wps.20681
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Arlington, VA
World Health Organization (2022) International Classification of Diseases, Eleventh Revision (ICD-11). https://icd.who.int/browse11. Accessed 27 Jul 2022
Fusar-Poli P, Radua J (2018) Ten simple rules for conducting umbrella reviews. Evid Based Ment Health 21:95–100. https://doi.org/10.1136/ebmental-2018-300014
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:332–336. https://doi.org/10.1136/bmj.b2535
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. J Am Med Assoc 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Shea BJ, Grimshaw JM, Wells GA et al (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 7:10. https://doi.org/10.1186/1471-2288-7-10
Higgins JPT, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Radua J, Ramella-Cravaro V, Ioannidis JPA et al (2018) What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry 17:49–66. https://doi.org/10.1002/wps.20490
Ioannidis JPA (2009) Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ 181:488–493. https://doi.org/10.1503/cmaj.081086
Petereit-Haack G, Bolm-Audorff U, Romero Starke K, Seidler A (2020) Occupational risk for post-traumatic stress disorder and trauma-related depression: a systematic review with meta-analysis. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17249369
Wang C-W, Chan CLW, Ho RTH (2013) Prevalence and trajectory of psychopathology among child and adolescent survivors of disasters: a systematic review of epidemiological studies across 1987–2011. Soc Psychiatry Psychiatr Epidemiol 48:1697–1720. https://doi.org/10.1007/s00127-013-0731-x
van Denderen M, de Keijser J, Kleen M, Boelen PA (2015) Psychopathology among homicidally bereaved individuals: a systematic review. Trauma Violence Abuse 16:70–80. https://doi.org/10.1177/1524838013515757
Spencer AE, Faraone SV, Bogucki OE et al (2016) Examining the association between posttraumatic stress disorder and attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. J Clin Psychiatry 77:72–83. https://doi.org/10.4088/JCP.14r09479
Bendall S, Jackson HJ, Hulbert CA, McGorry PD (2008) Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull 34:568–579. https://doi.org/10.1093/schbul/sbm121
Martins CMS, de Tofoli SM, von BaesJuruena CWM (2011) Analysis of the occurrence of early life stress in adult psychiatric patients: a systematic review. Psychol Neurosci 4:219–227. https://doi.org/10.3922/j.psns.2011.2.007
Palmier-Claus JE, Berry K, Bucci S et al (2016) Relationship between childhood adversity and bipolar affective disorder: systematic review and meta-analysis. Br J Psychiatry 209:454–459. https://doi.org/10.1192/bjp.bp.115.179655
Brander G, Pérez-Vigil A, Larsson H, Mataix-Cols D (2016) Systematic review of environmental risk factors for obsessive-compulsive disorder: a proposed roadmap from association to causation. Neurosci Biobehav Rev 65:36–62. https://doi.org/10.1016/j.neubiorev.2016.03.011
Cabizuca M, Marques-Portella C, Mendlowicz MV et al (2009) Posttraumatic stress disorder in parents of children with chronic illnesses: a meta-analysis. Heal Psychol 28:379–388. https://doi.org/10.1037/a0014512
Cunningham T, Hoy K, Shannon C (2016) Does childhood bullying lead to the development of psychotic symptoms? A meta-analysis and review of prospective studies. Psychosis 8:48–59. https://doi.org/10.1080/17522439.2015.1053969
de Aquino Ferreira LF, Queiroz Pereira FH, Neri Benevides AML, Aguiar Melo MC (2018) Borderline personality disorder and sexual abuse: a systematic review. Psychiatry Res 262:70–77. https://doi.org/10.1016/j.psychres.2018.01.043
Fernandes V, Osorio FL (2015) Are there associations between early emotional trauma and anxiety disorders? Evidence from a systematic literature review and meta-analysis. Eur Psychiatry 30:756–764. https://doi.org/10.1016/j.eurpsy.2015.06.004
Swartzman S, Booth JN, Munro A, Sani F (2017) Posttraumatic stress disorder after cancer diagnosis in adults: a meta-analysis. Depress Anxiety 34:327–339. https://doi.org/10.1002/da.22542
Teicher MH, Samson JA, Anderson CM, Ohashi K (2016) The effects of childhood maltreatment on brain structure, function and connectivity. Nat Rev Neurosci 1710(17):652–666. https://doi.org/10.1038/nrn.2016.111
Cross D, Fani N, Powers A, Bradley B (2017) Neurobiological development in the context of childhood trauma. Clin Psychol Sci Pract 24:111–124. https://doi.org/10.1111/cpsp.12198
Miller AH, Haroon E, Raison CL, Felger JC (2013) Cytokine targets in the brain: impact on neurotransmitters and neurocircuits. Depress Anxiety 30:297–306. https://doi.org/10.1002/da.22084
Houtepen LC, Vinkers CH, Carrillo-Roa T et al (2016) Genome-wide DNA methylation levels and altered cortisol stress reactivity following childhood trauma in humans. Nat Commun 7:10967. https://doi.org/10.1038/ncomms10967
Fries GR, Vasconcelos-Moreno MP, Gubert C et al (2015) Hypothalamic-pituitary-adrenal axis dysfunction and illness progression in bipolar disorder. Int J Neuropsychopharmacol 18:pyu043. https://doi.org/10.1093/ijnp/pyu043
Wright CE, Strike PC, Brydon L, Steptoe A (2005) Acute inflammation and negative mood: Mediation by cytokine activation. Brain Behav Immun 19:345–350. https://doi.org/10.1016/j.bbi.2004.10.003
Dziurkowska E, Wesolowski M (2021) Cortisol as a biomarker of mental disorder severity. J Clin Med 10:5204. https://doi.org/10.3390/jcm10215204
Faravelli C, Lo SC, Godini L et al (2012) Childhood stressful events, HPA axis and anxiety disorders. World J Psychiatry 2:13. https://doi.org/10.5498/WJP.V2.I1.13
Thomas N, Gurvich C, Kulkarni J (2019) Borderline personality disorder, trauma, and the hypothalamus-pituitary-adrenal axis. Neuropsychiatr Dis Treat 15:2601–2612. https://doi.org/10.2147/NDT.S198804
Masten CL, Guyer AE, Hodgdon HB et al (2008) Recognition of facial emotions among maltreated children with high rates of post-traumatic stress disorder. Child Abus Negl 32:139–153. https://doi.org/10.1016/j.chiabu.2007.09.006
Stanton KJ, Denietolis B, Goodwin BJ, Dvir Y (2020) Childhood trauma and psychosis: an updated review. Child Adolesc Psychiatr Clin N Am 29:115–129. https://doi.org/10.1016/j.chc.2019.08.004
Misiak B, Stramecki F, Gawęda Ł et al (2018) Interactions between variation in candidate genes and environmental factors in the etiology of schizophrenia and bipolar disorder: a systematic review. Mol Neurobiol 55:5075–5100. https://doi.org/10.1007/s12035-017-0708-y
Cattane N, Rossi R, Lanfredi M, Cattaneo A (2017) Borderline personality disorder and childhood trauma: exploring the affected biological systems and mechanisms. BMC Psychiatry 17:221. https://doi.org/10.1186/s12888-017-1383-2
Lopizzo N, Chiavetto LB, Cattane N et al (2015) Gene-environment interaction in major depression: focus on experience-dependent biological systems. Front Psychiatry. https://doi.org/10.3389/fpsyt.2015.00068
Witt SH, Streit F, Jungkunz M et al (2017) Genome-wide association study of borderline personality disorder reveals genetic overlap with bipolar disorder, major depression and schizophrenia. Transl Psychiatry 7:e1155. https://doi.org/10.1038/tp.2017.115
Ji D, Francesconi M, Flouri E, Papachristou E (2022) The role of inflammatory markers and cortisol in the association between early social cognition abilities and later internalising or externalising problems: evidence from a U.K. birth cohort. Brain Behav Immun. https://doi.org/10.1016/J.BBI.2022.07.002
Révész D, Verhoeven JE, Milaneschi Y et al (2014) Dysregulated physiological stress systems and accelerated cellular aging. Neurobiol Aging 35:1422–1430. https://doi.org/10.1016/j.neurobiolaging.2013.12.027
Tomiyama AJ, O’Donovan A, Lin J et al (2012) Does cellular aging relate to patterns of allostasis?. An examination of basal and stress reactive HPA axis activity and telomere length. Physiol Behav 106:40–45. https://doi.org/10.1016/j.physbeh.2011.11.016
Porter C, Palmier-Claus J, Branitsky A et al (2020) Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand 141:6–20. https://doi.org/10.1111/ACPS.13118
Bozzatello P, Rocca P, Baldassarri L et al (2021) The role of trauma in early onset borderline personality disorder: a biopsychosocial perspective. Front Psychiatry 12:1512
Cattane N, Rossi R, Lanfredi M, Cattaneo A (2017) Borderline personality disorder and childhood trauma: exploring the affected biological systems and mechanisms. BMC Psychiatry 17:1–14. https://doi.org/10.1186/s12888-017-1383-2
Stoltenborgh M, Bakermans-Kranenburg MJ, Van Ijzendoorn MH (2013) The neglect of child neglect: a meta-analytic review of the prevalence of neglect. Soc Psychiatry Psychiatr Epidemiol 48:345–355. https://doi.org/10.1007/s00127-012-0549-y
Kessler RC, Ruscio AM, Shear K, Wittchen HU (2010) Epidemiology of anxiety disorders. Curr Top Behav Neurosci 2:21–35
Choi J, Jeong B, Rohan ML et al (2009) Preliminary evidence for white matter tract abnormalities in young adults exposed to parental verbal abuse. Biol Psychiatry 65:227–234. https://doi.org/10.1016/j.biopsych.2008.06.022
Heim CM, Mayberg HS, Mletzko T et al (2013) Decreased cortical representation of genital somatosensory field after childhood sexual abuse. Am J Psychiatry 170:616–623. https://doi.org/10.1176/appi.ajp.2013.12070950
Kleber RJ (2019) Trauma and public mental health: a focused review. Front Psychiatry. https://doi.org/10.3389/FPSYT.2019.00451
Sweeney A, Filson B, Kennedy A et al (2018) A paradigm shift: relationships in trauma-informed mental health services. BJPsych Adv 24:319–333. https://doi.org/10.1192/bja.2018.29
Fredrickson R (2019) Trauma-informed care for infant and early childhood abuse. J Aggress Maltreatment Trauma 28:389–406. https://doi.org/10.1080/10926771.2019.1601143
Purgato M, Gross AL, Betancourt T et al (2018) Focused psychosocial interventions for children in low-resource humanitarian settings: a systematic review and individual participant data meta-analysis. Lancet Glob Heal 6:e390–e400. https://doi.org/10.1016/S2214-109X(18)30046-9
Marie-Mitchell A, Kostolansky R (2019) A systematic review of trials to improve child outcomes associated with adverse childhood experiences. Am J Prev Med 56:756–764. https://doi.org/10.1016/j.amepre.2018.11.030
Barlow DH, Harris BA, Eustis EH, Farchione TJ (2020) The unified protocol for transdiagnostic treatment of emotional disorders. World Psychiatry 19:245–246. https://doi.org/10.1002/wps.20748
Keen N, Hunter ECM, Peters E (2017) Integrated trauma-focused cognitive-behavioural therapy for post-traumatic stress and psychotic symptoms: a case-series study using imaginal reprocessing strategies. Front Psychiatry 8:1. https://doi.org/10.3389/fpsyt.2017.00092
Valiente-Gómez A, Moreno-Alcázar A, Treen D et al (2017) EMDR beyond PTSD: a systematic literature review. Front Psychol 8:1668. https://doi.org/10.3389/fpsyg.2017.01668
Novo P, Landin-Romero R, Radua J et al (2014) Eye movement desensitization and reprocessing therapy in subsyndromal bipolar patients with a history of traumatic events: a randomized, controlled pilot-study. Psychiatry Res 219:122–128. https://doi.org/10.1016/j.psychres.2014.05.012
Faretta E, Farra MD (2019) Efficacy of EMDR therapy for anxiety disorders. J EMDR Pract Res 13:325–332. https://doi.org/10.1891/1933-3196.13.4.325
Marsden Z, Lovell K, Blore D et al (2018) A randomized controlled trial comparing EMDR and CBT for obsessive–compulsive disorder. Clin Psychol Psychother 25:e10–e18. https://doi.org/10.1002/cpp.2120
Carletto S, Malandrone F, Berchialla P et al (2021) Eye movement desensitization and reprocessing for depression: a systematic review and meta-analysis. Eur J Psychotraumatol. https://doi.org/10.1080/20008198.2021.1894736
Peters E, Hardy A, Dudley R et al (2022) Multisite randomised controlled trial of trauma-focused cognitive behaviour therapy for psychosis to reduce post-traumatic stress symptoms in people with co-morbid post-traumatic stress disorder and psychosis, compared to treatment as usual: study protoco. Trials. https://doi.org/10.1186/s13063-022-06215-x
Valiente-Gómez A, Pujol N, Moreno-Alcázar A et al (2020) A Multicenter phase II RCT to compare the effectiveness of EMDR versus TAU in patients with a first-episode psychosis and psychological trauma: a protocol design. Front Psychiatry 10:1023. https://doi.org/10.3389/fpsyt.2019.01023
Moreno-Alcázar A, Radua J, Landín-Romero R et al (2017) Eye movement desensitization and reprocessing therapy versus supportive therapy in affective relapse prevention in bipolar patients with a history of trauma: study protocol for a randomized controlled trial. Trials 18:160. https://doi.org/10.1186/s13063-017-1910-y
Frissa S, Hatch SL, Fear NT et al (2016) Challenges in the retrospective assessment of trauma: comparing a checklist approach to a single item trauma experience screening question. BMC Psychiatry 16:20. https://doi.org/10.1186/s12888-016-0720-1
Danese A, Widom CS (2020) Objective and subjective experiences of child maltreatment and their relationships with psychopathology. Nat Hum Behav 4:811–818. https://doi.org/10.1038/s41562-020-0880-3
Blanco L, Sió A, Hogg B et al (2020) Traumatic events in dual disorders: prevalence and clinical characteristics. J Clin Med 9:1–14. https://doi.org/10.3390/jcm9082553
Acknowledgements
The authors would like to thank Prof. Paolo Fusar-Poli for guidance on applying the TRANSD criteria, and also to Prof. Jordi Alsono for guidance. B.L. Amann received two project grants (PI/15/02242, PI18/00009) and a mobility grant (BA21/00002) from the Instituto de Salud Carlos III-Subdirección General de Evaluación y Fomento de la Investigación, Plan Nacional 2008-2011 and 2013-2016, a NARSARD Independent Investigator Grant from the Brain & Behavior Research Foundation (24397) and a grant within the “Pla estratègic de recerca i innovació en salut” (PERIS; G60072253) by the Catalan Government. A. Moreno-Alcázar wants to thank also to the “Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement (2017 SGR 46 to “Unitat de Recerca del Centre Fòrum”), Generalitat de Catalunya (Government of Catalonia)” for the recognition as an emerging research group. B. Hogg thanks the support and funding of the Instituto de Salud Carlos III with a PFIS grant (FI10/00017). We acknowledge also the continuous support by the CIBERSAM (Centro de Investigación Biomédica en Red de Salud Mental). Alicia Valiente-Gómez thanks the support and funding of by the Instituto de Salud Carlos III with a Juan Rodés grant (JR19/00001).
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
BLA conceived the original idea for the paper. AM-A, AV-G, BH, BLA, IG-S and JR were involved in the design of the work. AM-A, ARR, AV-G, BH and IG-S carried out the article search and data extraction. LF and JR were involved in the analysis of the data. All authors were involved in the interpretation of the data and in writing and revising the draft of the manuscript. All authors have given final approval of the version to be published and are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hogg, B., Gardoki-Souto, I., Valiente-Gómez, A. et al. Psychological trauma as a transdiagnostic risk factor for mental disorder: an umbrella meta-analysis. Eur Arch Psychiatry Clin Neurosci 273, 397–410 (2023). https://doi.org/10.1007/s00406-022-01495-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-022-01495-5