Abstract
Purpose
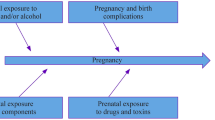
The aim of this study was to evaluate maternal, prenatal, perinatal, and postpartum parameters as risk factors for the later development of an attention deficit hyperactivity disorder (ADHD) in the child.
Methods
Women who had given birth at Erlangen University Hospital between 1996 and 1999 were sent a questionnaire in 2009. The results of the questionnaire were correlated with the prospectively collected data for the births in 1996–1999.
Results
A total of 573 mother and child pairs were analyzed. Forty-four of the mothers reported that their child had ADHD (7.7%). No significant associations were found for the following parameters: mother’s age; mother’s educational level; number of the pregnancy; maternal weight before and at the end of pregnancy; mother’s height; alcohol consumption during pregnancy; mode of delivery; gestational week; birthweight; umbilical artery blood values; Apgar score at 5 and 10 min; or breastfeeding. The parameters of smoking in pregnancy and an Apgar score lower than 7 after 1 min were significantly associated with a risk for later development of ADHD.
Conclusions
This analysis of maternal, prenatal, perinatal, and postnatal parameters found that smoking in pregnancy and a low Apgar score 1 min after birth are associated with a significantly greater risk for the development of ADHD. Beyond the question of the causal mechanism involved, this is a relevant finding, since smoking during pregnancy is a preventable risk factor.

Similar content being viewed by others
References
Froehlich TE et al (2007) Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Arch Pediatr Adolesc Med 161(9):857–864
Getahun D et al (2013) In utero exposure to ischemic-hypoxic conditions and attention-deficit/hyperactivity disorder. Pediatrics 131(1):e53–e61
Harris MN et al (2013) ADHD and learning disabilities in former late preterm infants: a population-based birth cohort. Pediatrics 132(3):e630–e636
Kotimaa AJ et al (2003) Maternal smoking and hyperactivity in 8-year-old children. J Am Acad Child Adolesc Psychiatry 42(7):826–833
Merikangas KR et al (2010) Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics 125(1):75–81
Pires TD, da Silva CMFP, de Assis SG (2013) Association between family environment and attention deficit hyperactivity disorder in children–mothers and teachers views. BMC Psychiatry 13
Sagiv SK et al (2013) Pre- and postnatal risk factors for ADHD in a nonclinical pediatric population. J Atten Disord 17(1):47–57
Visser SN et al (2014) Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry 53(1):34-46 e2
Golmirzaei J et al (2013) Evaluation of attention-deficit hyperactivity disorder risk factors. Int J Pediatr 2013:953103
Schlack R et al (2007) The prevalence of attention-deficit/hyperactivity disorder (ADHD) among children and adolescents in Germany. Initial results from the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 50(5–6):827–835
Getahun D et al (2013) Recent trends in childhood attention-deficit/hyperactivity disorder. JAMA Pediatr 167(3):282–288
Elia J et al (2010) Rare structural variants found in attention-deficit hyperactivity disorder are preferentially associated with neurodevelopmental genes. Mol Psychiatry 15(6):637–646
Faraone SV, Biederman J, Milberger S (1994) An exploratory study of ADHD among second-degree relatives of ADHD children. Biol Psychiatry 35(6):398–402
Eaves LJ et al (1997) Genetics and developmental psychopathology: 2. The main effects of genes and environment on behavioral problems in the Virginia Twin Study of Adolescent Behavioral Development. J Child Psychol Psychiatry 38(8):965–980
Samuel VJ et al (1999) A pilot controlled family study of DSM-III-R and DSM-IV ADHD in African–American children. J Am Acad Child Adolesc Psychiatry 38(1):34–39
Elia J et al (2012) Genome-wide copy number variation study associates metabotropic glutamate receptor gene networks with attention deficit hyperactivity disorder. Nat Genet 44(1):78–84
Nyman ES et al (2007) ADHD candidate gene study in a population-based birth cohort: association with DBH and DRD2. J Am Acad Child Adolesc Psychiatry 46(12):1614–1621
Gustafsson P, Kallen K (2011) Perinatal, maternal, and fetal characteristics of children diagnosed with attention-deficit-hyperactivity disorder: results from a population-based study utilizing the Swedish Medical Birth Register. Dev Med Child Neurol 53(3):263–268
Jaekel J, Wolke D, Bartmann P (2013) Poor attention rather than hyperactivity/impulsivity predicts academic achievement in very preterm and full-term adolescents. Psychol Med 43(1):183–196
Silva D et al (2014) Environmental risk factors by gender associated with attention-deficit/hyperactivity disorder. Pediatrics 133(1):e14–e22
Treyvaud K et al (2013) Psychiatric outcomes at age seven for very preterm children: rates and predictors. J Child Psychol Psychiatry 54(7):772–779
Milberger S et al (1997) Pregnancy, delivery and infancy complications and attention deficit hyperactivity disorder: issues of gene-environment interaction. Biol Psychiatry 41(1):65–75
Li J et al (2011) Low Apgar scores and risk of childhood attention deficit hyperactivity disorder. J Pediatr 158(5):775–779
Grizenko N et al (2016) Apgar Scores are associated with attention-deficit/hyperactivity disorder symptom severity. Can J Psychiatry 61(5):283–290
Froehlich TE et al (2009) Association of tobacco and lead exposures with attention-deficit/hyperactivity disorder. Pediatrics 124(6):e1054–e1063
Gustavson K et al (2017) Smoking in pregnancy and child ADHD. Pediatrics 139(2)
Chen Q et al (2014) Maternal pre-pregnancy body mass index and offspring attention deficit hyperactivity disorder: a population-based cohort study using a sibling-comparison design. Int J Epidemiol 43(1):83–90
Andersen S et al (2014) Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: a Danish nationwide cohort study. BJOG
Daseking M et al (2015) Smoking during pregnancy is a risk factor for executive function deficits in preschool-aged children. Geburtshilfe Frauenheilkd 75(1):64–71
Langley K et al (2012) Maternal and paternal smoking during pregnancy and risk of ADHD symptoms in offspring: testing for intrauterine effects. Am J Epidemiol 176(3):261–268
Ketzer CR et al (2012) Is there an association between perinatal complications and attention-deficit/hyperactivity disorder-inattentive type in children and adolescents? Rev Bras Psiquiatr 34(3):321–328
Acknowledgments
The authors are grateful for support from Friedrich Alexander University (FAU) of Erlangen–Nuremberg, provided in the framework of the Open Access Publishing funding program.
Author information
Authors and Affiliations
Contributions
E. Schwenke: investigation, methodology, project administration, writing. P. Fasching: supervision, methodology, project administration. F. Faschingbauer: funding acquisition, project administration. J. Pretscher: project administation. S. Kehl: writing review. R. Peretz: funding acquisition. A. Keller: formal analysis. L. Häberle: formal analysis. A. Eichler: writing review. V. Irlbauer-Mueller: writing review. U. Dammer: conceptualization, investigation. M.W. Beckmann: supervision. M. Schneider: data curation, writing review.
Corresponding author
Ethics declarations
Conflict of interest
The authors hereby declare that there were no conflicts of interest during the research conducted for this study.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Schwenke, E., Fasching, P.A., Faschingbauer, F. et al. Predicting attention deficit hyperactivity disorder using pregnancy and birth characteristics. Arch Gynecol Obstet 298, 889–895 (2018). https://doi.org/10.1007/s00404-018-4888-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4888-0