Abstract
Purpose
This systematic review aims to determine if there are evidence-based recommendations for the optimal mode of delivery for non-cephalic presenting first- and/or second twins. We investigated the impact of the mode of delivery on neonatal outcome for twin deliveries with (1) the first twin (twin A) in non-cephalic presentation, (2) the second (twin B) in non-cephalic presentation and (3) both twins in non-cephalic presentation.
Methods
A computer-aided search of Medline, Embase, Cinahl and Cochrane databases was carried out and quality of the studies was assessed with the Cochrane Collaboration’s tool for assessing risk of bias and the GRADE approach.
Results
One high-quality clinical trial (60 twin pairs) and 16 moderate/low-quality observational studies (3,167 twin pairs) showed no difference in neonatal outcome between vaginal and caesarean delivery in twin A and/or B.
Conclusion
Our results do not suggest benefit of caesarean over vaginal delivery for selected twin gestations with twin A and/or twin B in non-cephalic presentation. However, no final conclusion can be drawn due to the small sample sizes and statistic limitations of the included studies. Randomized studies with sufficient power are required to make a strong recommendation.
Similar content being viewed by others
Introduction
The incidence of twin pregnancy has increased largely because of the proliferation of assisted reproductive technologies and the rise in maternal age [1]. Twin gestations comprise approximately 1 % of all pregnancies but account for nearly 10 % of perinatal mortality [2, 3]. The increased morbidity and mortality of twin gestations is frequently attributed to preterm birth, intrauterine growth restriction and other unique complications of twin gestations such as twin–twin transfusion syndrome [4]. Hazards of twin delivery can be attributed to non-cephalic presentation as well [5]. Non-cephalic presentation of the first twin (twin A), the second twin (twin B) or both twins occurs in about 60 % of all twin pregnancies [2, 4, 5].
No consensus about the appropriate mode of delivery for non-cephalic presenting twins exists [6, 7]. Neither the practice bulletin on multiple gestation of the American College of Obstetricians and Gynecologists (ACOG) nor the guideline on multiple gestation of the Dutch Society for Obstetrics and Gynecology (NVOG) makes a recommendation for their route of delivery [6, 7]. Additionally, there is a general uncertainty about vaginal delivery of non-cephalic presenting twins, which is reflected by an increasing number of caesarean deliveries in twin gestations. In the United States, in 2003, 67 % of all twins were delivered by a caesarean section. Some obstetricians cite ‘twins’ as their only indication [8]. A policy of planned caesarean section might increase the risk of neonatal and maternal complications, like neonatal respiratory problems [2] or maternal febrile morbidity [9].
This systematic review aims to determine if there are evidence-based recommendations for the optimal mode of delivery for non-cephalic presenting first and/or second twins. We will investigate the impact of the mode of delivery on neonatal outcome for twin deliveries with (1) twin A in non-cephalic presentation, (2) twin B in non-cephalic presentation and (3) both twins in non-cephalic presentation.
Methods
Search strategy
A computer-aided search of Medline, Embase, Cinahl and Cochrane databases was carried out. The following search terms (with synonyms) were used: ‘twins’, ‘non-cephalic’ and ‘delivery’ (Appendix 1). Reference lists of identified studies were searched for additional relevant studies.
Inclusion criteria
Studies that compared the neonatal outcome (5-min Apgar scores and neonatal mortality) after vaginal delivery with the neonatal outcome after caesarean delivery for non-cephalic presenting twins were included. Twin A, twin B or both twin(s) had to be in non-cephalic presentation. Data of neonatal outcome had to be presented according to the mode of delivery. The twin pregnancy had to reach at least 32 weeks of gestation and both of the twins had to weigh at least 1,500 g. Every study that was published in English language was considered for inclusion, except review articles, case reports or poster session abstracts.
Selection of studies
The first reviewer (CN) screened the titles and abstracts of identified studies for eligibility. Papers that seemed to be relevant were obtained, and the full text articles were read for inclusion. If there was doubt about the suitability of the studies, they were discussed with another independent reviewer (TE).
Quality assessment
The first reviewer (CN) independently assessed various aspects of methodological quality of the included studies without masking the source or authorship of the articles. The Cochrane Collaboration’s tool for assessing risk of bias was used [10]. This tool consists of nine items about selection-, performance-, detection-, attribution- and reporting bias. Furthermore, the included studies were scored according to the GRADE approach [10].
Data extraction and analysis
Due to the heterogeneity of the data, studies could not be pooled. Therefore, we described per study whether a significant difference between vaginal and caesarean delivery was found in (1) low 5-min Apgar scores (<7) and (2) neonatal mortality. The 5-min Apgar scores <7 are widely used in the literature as measurement for poor neonatal outcome [2, 3, 8]. We made a distinction between the neonatal outcome of twin A and twin B. Significant differences were defined according to the definitions and statistics used in the different studies. We described the studies according to the presentation of the twins, i.e. (1) twin A in non-cephalic presentation, (2) twin B in non-cephalic presentation and (3) both twins in non-cephalic presentation.
Results
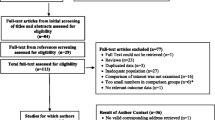
We identified 578 articles. Nineteen articles reporting the results of 18 studies that compared vaginal delivery with caesarean delivery for non-cephalic presenting twins were included [9, 11–28] (Fig. 1).
Literature search. Search updated September 18th 2011. N number of articles. Single asterisk indicates that one study was published in two articles [14, 15]. Double asterisks indicate that two articles [24, 27] included one subgroup with twin A and one subgroup with twin B in non-cephalic presentation
Quality assessment (Table 1)
None of the 18 included studies were blinded since blinding for the mode of delivery was not possible for patients, personnel and outcome assessors.
According to the GRADE classification [10], only one randomized clinical trial was identified which was of high quality [9]. According to the Cochrane Collaboration’s Tool for assessing the risk of bias [10], this trial described adequate methods of randomisation and concealment of allocation. Two out of 33 women randomized for vaginal delivery subsequently underwent caesarean section (one because of inadequate progress of labour and another because of heart rate monitoring of twin B suggesting foetal distress). Neonatal outcome was completely described for both twins in this study.
The remaining moderate- [11] or low-quality [12–28] observational studies reported different completeness of neonatal outcome data for both twins. None of the observational studies provided information about how the possibility of selective outcome reporting was examined.
Twin A in non-cephalic presentation (Tables 2, 3)
Eight low-quality observational studies including 1,475 twin pairs compared the mode of delivery of twins with the twin A in non-cephalic presentation [12–16, 23–25, 27]. For twin A, none of the eight studies reported a significant difference in low 5-min Apgar scores or in neonatal mortality. For the twin B, no significant differences were reported, but in 50 % of the studies information about the neonatal outcome of twin B was lacking.
Twin B in non-cephalic presentation (Tables 2, 4)
Eleven studies including 2,166 twin pairs compared the mode of delivery of twins with twin B in non-cephalic presentation, including one high-quality randomized clinical trial [9] (60 twin pairs) and ten low-quality observational studies [17–22, 24, 26–28].
The randomized clinical trial that compared vaginal with caesarean delivery did not report a significant difference in low 5-min Apgar scores or in neonatal mortality for the twin A and B [9].
For the twin A, none of the studies did report significant differences in neonatal outcome but information about the neonatal outcome of twin A was lacking in 64 % (low 5-min Apgar scores) and 55 % (neonatal mortality) of the studies.
For the twin B, most studies (82 %) did not report a significant difference in low 5-min Apgar scores or neonatal mortality but one study [22] (482 twin pairs) did report a significant difference in low 5-min Apgar scores favouring caesarean delivery (p < 0.05). This study [22] did not report a significant difference in neonatal mortality.
Both twins in non-cephalic presentation (Tables 2, 5)
One moderate-quality observational study [11] including 68 twin pairs compared the mode of delivery of twins with both twins in non-cephalic presentation. No significant differences were reported for twins A and B.
Discussion
The aim of the current review was to compare vaginal with caesarean delivery for twin deliveries with twin A in non-cephalic presentation, twin B in non-cephalic presentation and both twins in non-cephalic presentation. This evaluation is important because of the increasing numbers of caesarean sections without adequate supporting evidence for their use [8].
One high-quality clinical trial [9] (60 twin pairs) and 16 moderate/low-quality observational studies [11–21, 23–28] (3,167 twin pairs) showed no difference in neonatal outcome between vaginal and caesarean deliveries in twin A and/or B. Only one low-quality observational study [22] (482 twin pairs) reported a significant difference in low 5-min Apgar scores favouring caesarean delivery but there was no significant difference in neonatal mortality.
A reason to recommend caesarean over vaginal delivery if twin A is presenting non-cephalically might be to avoid the possibility of interlocking twins, which theoretically could occur in breech/cephalic and breech/transverse presenting twins. However, the incidence of interlocked twins is very low [1]. Furthermore, according to Hannah et al. [29] in term breech singletons, planned caesarean section is better than vaginal delivery. However, a previous Cochrane review did describe the maternal and neonatal outcome of the same clinical trial [9] we cited, and they stated that caesarean delivery of a non cephalic presenting twin B is associated with increased maternal morbidity but not with improved neonatal outcome, and that a policy of caesarean delivery should not be adopted without further controlled trials [30]. Additionally, previous research did not find excessive morbidity or mortality associated with vaginal delivery of non-cephalic presenting twins compared with cephalic presenting twins [31–35]. Because we include only studies that compared non-cephalic presenting twins with each other, these reports were excluded.
A few studies provided detailed information about the mode of vaginal delivery like external cephalic version or (assisted) breech extraction. Both external version [36–38] and breech extraction [39–41] are recommended in the literature. To our knowledge, there are no randomized controlled data comparing external version with breech extraction. Future research about this subject might be useful.
A limitation of this review is that the included studies had relatively small sample sizes. However, in a meta-analysis from 2003, Hodge et al. [2] pooled the data of four studies that we described separately [9, 13, 17, 25]. They remarked that even the sample size of the pooled data was too small to draw conclusions. Therefore, although after including more recent studies statistic evidence for the best mode of delivery for twins presenting non-cephalically is still missing and no strong recommendation can be made. Furthermore, most studies did not correct (statistically or by randomisation) for confounding factors. Important confounding factors are parity or medical, obstetric or emergency indications for a caesarean section.
Additionally, most studies did not provide information about monoamnioticity. Therefore, it is mostly unknown if only diamniotic twins were included, or if monoamniotic and diamniotic twins were mixed. Ideally, you should analyse these groups separately. However, the bias due to this cause might be limited if the percentage of monoamniotic twins is equal in both the vaginal and the caesarean delivery group.
Finally, in two studies [11, 16], we used information from the abstract only because we were not able to get full text of both papers. However, we were able to retrieve all information we needed from the abstract, but ideally studies should be assessed with the full text available.
Therefore, our results have to be interpreted with caution.
Conclusion
Our results do not suggest benefit of caesarean over vaginal delivery for selected twin gestations with twin A and/or twin B in non-cephalic presentation. However, no final conclusion can be drawn. Randomized studies with sufficient power are required to make a strong recommendation.
References
Cruikshank DP (2007) Intrapartum management of twin gestations. Obstet Gynecol 109:1167–1176
Hogle KL, Hutton EK, McBrien KA et al (2003) Cesarean delivery for twins: a systematic review and meta-analysis. Am J Obstet Gynecol 188:220–227
Stichting Perinatale Registratie Nederland, Perinatale Zorg in Nederland 2008. Utrecht: Stichting Perinatale Registratie nederland. (2011)
Pope RJ, Weintraub AY, Sheiner E (2010) Vaginal delivery of vertex–nonvertex twins: a fading skill? Arch Gynecol Obstet 282:117–120
Boggess KA, Chisholm CA (1997) Delivery of the nonvertex second twin: a review of the literature. Obstet Gynecol Surv 52:728–735
Dutch Society for Obstetrics and Gynecology (2011) Guideline Multiple Gestation version 2.0. March 2005. Available at http://www.nvog.nl
American College of Obstetricians and Gynecologsits Committee on Practice Bulletins-Obstetrics et al (2004) ACOG Practice Bulletin #56: multiple gestation: complicated twin, triplet, and high-order multifetal pregnancy. Obstet Gynecol 104(4):869–883
Carroll MA, Yeomans ER (2006) Vaginal delivery of twins. Clin Obstet Gynecol 49:154–166
Rabinovici J, Barkai G, Reichman B et al (1987) Randomized management of the second nonvertex twin: vaginal delivery or cesarean section. Am J Obstet Gynecol 156:52–56
Higgins JPT, Green S (2011) Cochrane handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration, 2011. Available at http://www.cohrane-handbook.org
Essel JK, Opai-Tetteh ET (1996) Is routine caesarean section necessary for breech-breech and breech-transverse twin gestations? S Afr Med J 86:1196–1200
Sentilhes L, Goffinet F, Talbot A et al (2007) Attempted vaginal versus planned cesarean delivery in 195 breech first twin pregnancies. Acta Obstet Gynecol Scand 86:55–60
Grisaru D, Fuchs S, Kupferminc MJ et al (2000) Outcome of 306 twin deliveries according to first twin presentation and method of delivery. Am J Perinatol 17:303–307
Bu-Heija AT, Ziadeh S, Obeidat A (1998) Mode of delivery and perinatal results of the breech first twin. J Obstet Gynaecol 18:47–49
Bu-Heija AT, Ziadeh S, Abukteish F et al (1998) Retrospective study of outcome on vaginal and abdominal delivery in twin pregnancy in which twin 1 is presenting by the breech. Arch Gynecol Obstet 261:71–73
Blickstein I, Weissman A, Ben-Hur H et al (1993) Vaginal delivery of breech-vertex twins. J Reprod Med 38:879–882
Wells SR, Thorp JM Jr, Bowes WA Jr (1991) Management of the nonvertex second twin. Surg Gynecol Obstet 172:383–385
Gocke SE, Nageotte MP, Garite T et al (1989) Management of the nonvertex second twin: primary cesarean section, external version, or primary breech extraction. Am J Obstet Gynecol 161:111–114
Caukwell S, Murphy DJ (2002) The effect of mode of delivery and gestational age on neonatal outcome of the non-cephalic- presenting second twin. Am J Obstet Gynecol 187:1356–1361
Winn HN, Cimino J, Powers J et al (2001) Intrapartum management of nonvertex second-born twins: a critical analysis. Am J Obstet Gynecol 185:1204–1208
Acker D, Lieberman M, Holbrook RH et al (1982) Delivery of the second twin. Obstet Gynecol 59:710–711
Atis A, Aydin Y, Donmez M et al (2011) Apgar scores in assessing morbidity of the second neonate of cephalic/non-cephalic twins in different delivery modes. J Obstet Gynaecol 31:43–47
Nassar AH, Maarouf HH, Hobeika EM et al (2004) Breech presenting twin A: is vaginal delivery safe? J Perinat Med 32:470–474
Roopnarinesingh AJ, Sirjusingh A, Bassaw B et al (2002) Vaginal breech delivery and perinatal mortality in twins. J Obstet Gynaecol 22:291–293
Blickstein I, Goldman RD, Kupferminc M (2000) Delivery of breech first twins: a multicenter retrospective study. Obstet Gynecol 95:37–42
Mauldin JG, Newman RB, Mauldin PD (1998) Cost-effective delivery management of the vertex and nonvertex twin gestation. Am J Obstet Gynecol 179:864–869
Kelsick F, Minkoff H (1982) Management of the breech second twin. Am J Obstet Gynecol 144:783–786
Greig PC, Veille JC, Morgan T et al (1992) The effect of presentation and mode of delivery on neonatal outcome in the second twin. Am J Obstet Gynecol 167:901–906
Hannah ME, Hannah WJ, Hewson SA, Term Breech Trial Collaborative Group et al (2000) Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Lancet 356:1375–1383
Crowther CA (2000) Caesarean delivery for the second twin. Cochrane Database Syst Rev:CD000047
Fishman A, Grubb DK, Kovacs BW (1993) Vaginal delivery of the nonvertex second twin. Am J Obstet Gynecol 168:861–864
Mazor M, Leiberman JR, Dreval D et al (1986) Management and outcome of vertex-breech and vertex-vertex presentation in twin gestation: a comparative study. Eur J Obstet Gynecol Reprod Biol 22:69–75
Blickstein I, Schwartz-Shoham Z, Lancet M et al (1987) Vaginal delivery of the second twin in breech presentation. Obstet Gynecol 69:774–776
Sibony O, Touitou S, Luton D et al (2006) Modes of delivery of first and second twins as a function of their presentation. Study of 614 consecutive patients from 1992 to 2000. Eur J Obstet Gynecol Reprod Biol 126:180–185
Oettinger M, Ophir E, Markovitz J et al (1993) Is cesarean section necessary for delivery of a breech first twin? Gynecol Obstet Invest 35:38–43
Chervenak FA, Johnson RE, Berkowitz RL et al (1983) Intrapartum external version of the second twin. Obstet Gynecol 62:160–165
Tchabo JG, Tomai T (1992) Selected intrapartum external cephalic version of the second twin. Obstet Gynecol 79:421–423
Kaplan B, Peled Y, Rabinerson D et al (1995) Successful external version of B-twin after the birth of A-twin for vertex–non-vertex twins. Eur J Obstet Gynecol Reprod Biol 58:157–160
Berglund L, Axelsson O (1989) Breech extraction versus cesarean section for the remaining second twin. Acta Obstet Gynecol Scand 68:435–438
Smith SJ, Zebrowitz J, Latta RA (1997) Method of delivery of the nonvertex second twin: a community hospital experience. J Matern Fetal Med 6:146–150
Chauhan SP, Roberts WE, McLaren RA et al (1995) Delivery of the nonvertex second twin: breech extraction versus external cephalic version. Am J Obstet Gynecol 173:1015–1020
Conflict of interest
None of the authors have conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Medline: (((((twins[Title/Abstract] OR twin[Title/Abstract]) OR sibling[Title/Abstract]) OR siblings[Title/Abstract]) OR reciprocal[Title/Abstract]) OR reciprocals[Title/Abstract])) AND (((((((((breech presentation[Title/Abstract] OR breech-presentation[Title/Abstract]) OR breech-presentations[Title/Abstract]) OR breech[Title/Abstract]) OR non-vertex[Title/Abstract]) OR non-vertex-presentation[Title/Abstract]) OR non-vertex-presentations[Title/Abstract]) OR non-cephalic[Title/Abstract]) OR non-cephalic-presentation[Title/Abstract]) OR non-cephalic-presentations[Title/Abstract])) AND ((((((((((((((((((((((((((vaginal delivery[Title/Abstract] OR vaginal[Title/Abstract]) OR vaginally[Title/Abstract]) OR deliver[Title/Abstract]) OR delivered[Title/Abstract]) OR delivery[Title/Abstract]) OR deliveries[Title/Abstract]) OR childbirth[Title/Abstract]) OR childbirths[Title/Abstract]) OR accouchement[Title/Abstract]) OR bearing[Title/Abstract]) OR birth[Title/Abstract]) OR births[Title/Abstract]) OR birthing[Title/Abstract]) OR bringing forth[Title/Abstract]) OR childbearing[Title/Abstract]) OR confinement[Title/Abstract]) OR geniture[Title/Abstract]) OR labor[Title/Abstract]) OR labour[Title/Abstract]) OR lying-in[Title/Abstract]) OR paturition[Title/Abstract]) OR parturitions[Title/Abstract]) OR travail[Title/Abstract]) OR extraction[Title/Abstract]) OR extractions[Title/Abstract]) OR (((((((caesarian section[Title/Abstract] OR caesarian sections[Title/Abstract]) OR caesarian[Title/Abstract]) OR caesarian[Title/Abstract]) OR section[Title/Abstract]) OR sections[Title/Abstract]) OR abdominal[Title/Abstract]) OR abdominally[Title/Abstract])).
Embase: (((((twins:ab,ti OR twin:ab,ti) OR sibling:ab,ti) OR siblings:ab,ti) OR reciprocal:ab,ti) OR reciprocals:ab,ti) AND (((((((((breech presentation:ab,ti OR breech-presentation:ab,ti) OR breech-presentations:ab,ti) OR breech:ab,ti) OR non-vertex:ab,ti) OR non-vertex-presentation:ab,ti) OR non-vertex-presentations:ab,ti) OR non-cephalic:ab,ti) OR non-cephalic-presentation:ab,ti) OR non-cephalic-presentations:ab,ti) AND ((((((((((((((((((((((((((vaginal delivery:ab,ti OR vaginal:ab,ti) OR vaginally:ab,ti) OR deliver:ab,ti) OR delivered:ab,ti) OR delivery:ab,ti) OR deliveries:ab,ti) OR childbirth:ab,ti) OR childbirths:ab,ti) OR accouchement:ab,ti) OR bearing:ab,ti) OR birth:ab,ti) OR births:ab,ti) OR birthing:ab,ti) OR bringing forth:ab,ti) OR childbearing:ab,ti) OR confinement:ab,ti) OR geniture:ab,ti) OR labor:ab,ti) OR labour:ab,ti) OR lying-in:ab,ti) OR paturition:ab,ti) OR parturitions:ab,ti) OR travail:ab,ti) OR extraction:ab,ti) OR extractions:ab,ti) OR (((((((caesarian section:ab,ti OR caesarian sections:ab,ti) OR caesarian:ab,ti) OR caesarian:ab,ti) OR section:ab,ti) OR sections:ab,ti) OR abdominal:ab,ti) OR abdominally:ab,ti)).
Cochrane: (Twin OR twins OR sibling OR siblings OR reciprocal OR reciprocals) AND (breech-presentation OR breech-presentation OR breech OR non-vertex OR non-cephalic) AND (vaginal OR vaginally or deliver OR delivered OR delivery OR deliveries OR childbirth OR childbirths OR accouchement OR bearing OR birth OR births OR birthing OR brining forth OR childbearing OR confinement OR geniture OR labor OR labour OR caesarian OR caesarians OR section OR sections OR abdominal OR abdominally) Field: abstract.
CINAHL: (Twin OR twins OR sibling OR siblings OR reciprocal OR reciprocals) AND (breech-presentation OR breech-presentation OR breech OR non-vertex OR non-cephalic) AND (vaginal OR vaginally or deliver OR delivered OR delivery OR deliveries OR childbirth OR childbirhs OR accouchement OR bearing OR birth OR births OR birthing OR brining forth OR childbearing OR confinement OR geniture OR labor OR labour OR caesarian OR caesarians OR section OR sections OR abdominal OR abdominally) Field: abstract.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Steins Bisschop, C.N., Vogelvang, T.E., May, A.M. et al. Mode of delivery in non-cephalic presenting twins: a systematic review. Arch Gynecol Obstet 286, 237–247 (2012). https://doi.org/10.1007/s00404-012-2294-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-012-2294-6