Abstract
Introduction
An increasing proportion of women in the US and other countries delay initiation of childbearing until their thirties. Little is known about their subsequent pregnancies, particularly with regard to pregnancy spacing.
Objectives
To determine interpregnancy interval (IPI) patterns, factors associated with IPI among women delaying initiation of childbearing until their thirties, and ascertain if delay in initiation of childbearing is associated with increased likelihood for short interpregnancy interval of less than 6 months.
Methods
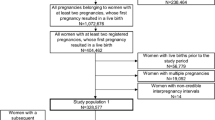
A retrospective cohort study was performed using the Missouri maternal linked file for 1978–1997, inclusive. Analysis was limited to mothers aged 20–50 years at first pregnancy, having a first and second pregnancy during the study period; the sample size included 242,559 mother–infant pairs. Analysis strategies included stratified analysis, and multivariable logistic regression. Interpregnancy interval was main outcome variable, and was grouped in seven categories: 0–5, 6–11, 12–17, 18–23, 24–59, 60–119, ≥120 months.
Results
The mean interpregnancy interval was significantly shorter for women delaying start of childbearing (≥30 years) compared to 20–29 year olds. Observed intervals are 31 (±24) months for mothers aged 20–29 years, 25 (±17) months for mothers aged 30–34 years, 21 (± 14) for 35–39 year olds, and 19 (±16) for 40–50 year olds (P < 0.0001). A significant trend for shorter intervals was noted as maternal age at first pregnancy increased (P < 0.0001). Factors associated with interpregnancy interval for women delaying initiation of childbearing included adverse outcome in preceding pregnancy, and low educational status. Mothers aged 35 and above at first pregnancy had increased odds for a second pregnancy following short IPI <6 months; (35–39 years OR = 1.26 95% CI 1.11–1.44; 40–50 OR = 1.91 95% CI 1.13–3.24). Mothers aged 30–34 years have lower odds for short IPI (OR = 0.93 95% CI 0.87–0.99).
Conclusion
First time mothers aged 35 and above have higher odds of having a second pregnancy shortly after their first pregnancy. Given the increasing number of first time mothers aged 35 and above, these findings are of relevance for preconception counseling for this unique population of women.


Similar content being viewed by others
References
Ventura SJ (1989) Trends and variations in first births to older mothers, United States, 1970–86. Vital Health Stat 21:1–27
Breart G (1997) Delayed childbearing. Eur J Obstet Gynecol Reprod Biol 75:71–73. doi:10.1016/S0301-2115(97)00190-5
Nabukera S, Wingate MS, Alexander GR, Salihu HM (2006) First-time births among women 30 years and older in the United States: patterns and risk of adverse outcomes. J Reprod Med 51:676–682
Berkowitz GS, Skovron ML, Lapinski RH, Berkowitz RL (1990) Delayed childbearing and the outcome of pregnancy. N Engl J Med 322:659–664
Ales KL, Druzin ML, Santini DL (1990) Impact of advanced maternal age on outcome of pregnancy. Surg Gynecol Obstet 85:65–70
Astolfi P, Zonta LA (2002) Delayed maternity and risk of delivery. Paediatr Perinat Epidemiol 16:67–72. doi:10.1046/j.1365-3016.2002.00375.x
Barkan SE, Bracken MB (1987) Delayed childbearing: no evidence for increased risk of low birth weight and preterm delivery. Am J Epidemiol 125:101–109
Brassil MJ, Turner MJ, Egan DM, MacDonald DW (1987) Obstetric outcomes in first time mothers aged 40 years and over. Eur J Obstet Gynecol Reprod Biol 25:115–120. doi:10.1016/0028-2243(87)90114-6
Callaway LK, Lust K, Mcintyre DH (2005) Pregnancy outcomes in women of very advanced maternal age. Aust N Z J Obstet Gynaecol 45:12–16. doi:10.1111/j.1479-828X.2005.00333.x
Carolan M (2003) The graying of the obstetric population: implications for the older mother. J Obstet Gynecol Neonatal Nurs 32:19–27. doi:10.1177/0884217502239797
St John C (1982) Race differences in age at first birth and the pace of subsequent fertility: implications of the minority group status hypothesis. Demography 19:301–314. doi:10.2307/2060973
Zhu BP, Rolfs RT, Nangle BE, Horan JM (1999) Effect of the interval between pregnancies on perinatal outcomes. N Engl J Med 340:589–594. doi:10.1056/NEJM199902253400801
Cnattingius S, Berendes HW, Forman MR (1993) Do delayed childbearers face increased risks of adverse pregnancy outcomes after the first birth? Obstet Gynecol 81:512–516
Kaharuza FM, Sabroe S, Basso O (2001) Choice and chance: determinants of short interpregnancy intervals in Denmark. Acta Obstet Gynecol Scand 80:532–538. doi:10.1034/j.1600-0412.2001.080006532.x
Upadhyay UD, Hindin MJ (2005) Do higher status and more autonomous women have longer birth intervals? Results from Cebu, Philippines. Soc Sci Med 60:2641–2655. doi:10.1016/j.socscimed.2004.11.032
Spratley E, Taffel S (1981) Interval between births, United States: 1970–77 an analytical review of recent trends and differentials in the interval between current live birth and previous live birth or fetal death. Vital Health Stat 21:1–47
Centers for Disease Control (1998) Risk factors for short interpregnancy interval-Utah, June 1996–June 1997. MMWR 47:930–934
Kalmuss DS, Namerow PB (1994) Subsequent childbearing among teenage mothers: the determinants of a closely spaced second birth. Fam Plann Perspect 26(159):149–153
Mott FL (1986) The pace of repeated childbearing among young American mothers. Fam Plann Perspect 18:5–12. doi:10.2307/2135193
Klebanoff MA (1988) Short interpregnancy interval and the risk of low birthweight. Am J Public Health 78:667–670
Smith GC, Pell JP, Dobbie R (2003) Interpregnancy interval and risk of preterm birth and neonatal death: retrospective cohort study. BMJ 327:313–319. doi:10.1136/bmj.327.7410.313
Majinge CR, Lema VM (1993) Pregnancy intervals: their determinants and fetal outcome at the KCMC, Moshi, Tanzania. East Afr Med J 70:544–550
Klerman LV, Cliver SP, Goldenberg RL (1998) The impact of short interpregnancy interval on pregnancy outcomes in a low income population. Am J Public Health 88:1182–1185
Basso O, Olsen J, Knudsen LB, Christensen K (1998) Low birth weight and preterm birth after short interpregnancy intervals. Am J Obstet Gynecol 178:259–263. doi:10.1016/S0002-9378(98)80010-0
Adams MM, Delaney KM, Stupp PW, McCarthy BJ, Rawlings JS (1997) The relationship of interpregnancy interval to infant birth weight and length of gestation among low-risk women, Georgia. Paediatr Perinat Epidemiol 11:48–62. doi:10.1046/j.1365-3016.11.s1.8.x
Rousso D, Panidis D, Gkoutzioulis F, Kourtis A, Mavromatidis G, Kalahanis I (2002) Effect of interval between pregnancies on the health of mother and child. Eur J Obstet Gynecol Reprod Biol 105:4–6. doi:10.1016/S0301-2115(02)00077-5
Norton M (2005) New evidence on birth spacing: promising findings for improving newborn, infant, child and maternal health. Int J Gynaecol Obstet 89:S1–S6. doi:10.1016/j.ijgo.2004.12.012
Conde-Agudelo A, Rosas-Bermudez A, Kafury-Goeta AC (2006) Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA 295:1809–1823. doi:10.1001/jama.295.15.1809
Conde-Agudelo A, Rosas-Bermudez A, Kafury-Goeta AC (2007) Effects of birth spacing on maternal health: a systematic review. Am J Obstet Gynecol 196:297–308. doi:10.1016/j.ajog.2006.05.055
DeFranco EA, Stamilio DM, Boslaugh SE, Gross GA, Muglia LJ (2007) A short interpregnancy interval is a risk factor for preterm birth and its recurrence. Am J Obstet Gynecol 197:264–6
Herman AA, McCarthy BJ, Bakewell JM, Ward RH, Mueller BA, Maconochie NE et al (1997) Data linkage methods used in maternally-linked birth and infant death surveillance data sets from the United States (Georgia, Missouri, Utah and Washington State), Israel, Norway, Scotland and Western Australia. Paediatr Perinat Epidemiol 11(Suppl 1):5–22. doi:10.1046/j.1365-3016.11.s1.11.x
Salihu HM, Sharma PP, Aliyu MH, Kristensen S, Grimes-Dennis J, Kirby RS et al (2006) Is small for gestational age a marker of future fetal survival in utero? Obstet Gynecol 107:851–856
Casterline JB (1989) Maternal age, gravidity, and pregnancy spacing effects on spontaneous fetal mortality. Soc Biol 36:186–212
Cleary-Goldman J, Malone FD, Vidaver J, Ball RH, Faster C (2005) Impact of maternal age on obstetric outcome. Obstet Gynecol 105:983–990
Petersen DJ, Alexander GR (1992) Seasonal variation in adolescent conceptions, induced abortions, and late initiation of prenatal care. Public Health Rep 107:701–706
Alexander GR, Kotelchuck M (1996) Quantifying the adequacy of prenatal care: a comparison of indices. Public Health Rep 111:408–418
Centers for Disease Control Body mass index for adults. http://www.cdc.gov/nccdphp/dnpa/bmi/adult_BMI/about_adult_BMI.htm. Accessed 11 June 2007
Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M (1996) A United States national reference for fetal growth. Obstet Gynecol 87:163–168. doi:10.1016/0029-7844(95)00386-X
Millman SR, Hendershot GE (1980) Early fertility and lifetime fertility. Fam Plann Perspect 12:139–149. doi:10.2307/2134568
Lydon-Rochelle MT, Cardenas V, Nelson JL, Tomashek KM, Mueller BA, Easterling TR (2005) Validity of maternal and perinatal risk factors reported on fetal death certificates. Am J Public Health 95:1948–1951. doi:10.2105/AJPH.2004.044305
Cahill AG, Macones GA (2006) Vital considerations for the use of vital statistics in obstetrical research. Am J Obstet Gynecol 194:909–910. doi:10.1016/j.ajog.2006.02.031
Kirby RS, Malnory M (1999) Limitations of databases. Pediatrics 103:531–532. doi:10.1542/peds.103.2.531
Author information
Authors and Affiliations
Corresponding author
Additional information
Greg R. Alexander was deceased.
Rights and permissions
About this article
Cite this article
Nabukera, S.K., Wingate, M.S., Salihu, H.M. et al. Pregnancy spacing among women delaying initiation of childbearing. Arch Gynecol Obstet 279, 677–684 (2009). https://doi.org/10.1007/s00404-008-0793-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-008-0793-2