Abstract
Background
Detecting heart failure (HF) patients at risk is a relevant clinical problem. Our goal was to define associations of clinical HF-markers and exercise parameters with respect to their prognostic power in HF-patients.
Methods
We performed cardiopulmonary exercise testing (CPET) in 103 ischemic HF-patients. CPET-parameters included peak VO2, VO2 at AT, peak oxygen pulse, minimal CO2 and O2 equivalents, VE/VCO2 and s1, a motivation-independent and submaximal parameter representing the initial slope of the VCO2/VO2-curve that has not been described in HF-patients so far.
Results
Median follow-up was 668 days. The combined endpoint of cardiovascular death and rehospitalization due to HF occurred in 14 patients. Patients with/without events differed significantly regarding their age, NYHA-class, LVEF and NT-proBNP serum-levels. Patients with events had significantly lower peak VO2- and higher s1-values. NT-proBNP serum-levels, NYHA-class and LVEF were significantly correlated with peak VO2. Only age, peak VO2 and s1 were independent predictors of adverse events. Using multivariate analysis, s1 was a strong and independent parameter with good sensitivity and specificity.
Conclusion
s1 is an independent and powerful predictor in HF-patients. Since s1 is independent of maximal exercise capacity, s1 might be more accurate for the evaluation of HF-patients not willing or unable to perform maximal exercise.
Similar content being viewed by others
Introduction
The increasing prevalence of heart failure in western civilizations creates a substantial burden on national healthcare systems [11]. Despite novel diagnostic and therapeutic options, prognosis of heart failure patients remains poor [18]. Therefore, the identification of patients at risk for adverse events and the need for more intensive treatment plays a major role in clinical practice. Besides clinical and laboratory parameters such as left ventricular ejection fraction (LVEF), NYHA-class [9, 24], and natriuretic peptide serum levels, cardiopulmonary exercise testing (CPET) provides important information to upscale heart failure therapy. A number of CPET-derived variables have been shown to predict adverse outcome in patients with heart failure [8, 15, 17, 19, 21]. In fact, current guidelines for the evaluation of eligibility for heart transplantation include the measurement of peak oxygen consumption during exercise (peak VO2) [21]. So far, patients with a peak VO2 below 14 ml/kg/min are generally considered for heart transplantation. However, the prognostic data regarding peak VO2 values have been collected in the pre-betablocker-era [33]. Indeed, recent studies provided controversial results for the prognostic power of peak VO2 [23, 33] in patients on betablocker therapy and raised the question whether a lower cut-off value would be more accurate [25, 38]. More importantly, the usefulness of peak VO2 is restricted to patients, who are able and willing to perform at their cardio-respiratory maximum.
Therefore, the goal of our study was to identify CPET parameters, which are independent from the patients` motivation to exercise to their cardiorespiratory maximum and which can be obtained already at submaximal exercise levels, in order to predict outcome in patients with chronic ischemic heart failure under optimized therapy. Our results demonstrate that calculation of the initial slope of the VCO2/VO2-curve (s1), which had so far not been described in heart failure patients [10, 30], significantly improved the prediction of cardiovascular outcome.
Methods
Patients
We included 103 consecutive patients with coronary artery disease into the study, who had a documented myocardial infarction at least 3 months prior to enrollment. All patients were referred to our heart failure clinic for further evaluation of documented or assumed heart failure. All patients had residual well demarcated region of left ventricular systolic dysfunction and a patent infarct related artery as documented by angiography (performed and evaluated by BA and VS). No patient had flow-limiting coronary stenosis at the time of exercise testing, thus excluding the induction of myocardial ischemia during exercise. Clinical symptoms of heart failure were not required for inclusion. All patients were in clinically stable condition for at least 4 weeks and showed no signs of acute cardiac decompensation. Patients with relevant comorbidity such as cancer, infection or severe pulmonary disease were not included in our study. Medical therapy required beta blockers, ACE-inhibitors or ARBs, unless specific contraindications were present (see Table 1).
Measurement of BNP-serum levels
NT-proBNP was analysed in blood serum samples drawn from an antecubital vein in a Heparin-coated tube. All samples were collected before cardiopulmonary exercise testing. Immediately after venipuncture, blood was stored on ice and the supernatant was stored at −70°C after centrifugation, until analysis with an Elecsys® NT-proBNP Assay (Hoffmann-LaRoche AG, Basel) was performed.
Cardiopulmonary exercise testing
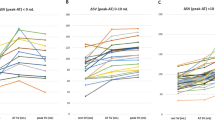
All patients performed a standard bicycle exercise protocol to maximum tolerance. Exercise started with 50 W after a 4 min unload-phase, followed by stepwise increase by 25 W every 180 s using a Jaeger bicycle ergometer ER 900 l (Viasys GmbH, Hoechberg, Germany). Continuous monitoring by 12-lead ECG was performed in order to detect arrhythmias or signs of myocardial ischemia. Blood pressure was measured every 3 min by a cuff sphygmomanometer. Breath-by-breath gas exchange measurements were analysed with a Jaeger Oxycon Alpha testing station (Viasys GmbH, Hoechberg, Germany). All VO2-data were averaged automatically every 30 s and reviewed by the authors. Maximal VO2 was determined as the peak value of oxygen uptake during exercise. O2 uptake at the anaerobic threshold (VO2 AT) was determined according to the V-slope-method of Beaver et al. [4]. IS and LG independently determined peak VO2 and examined the AT, blinded to the patients clinical characteristics. Peak Oxygen pulse (peak O2 pulse) was calculated as the ratio of peak VO2 and the corresponding heart rate. Ventilatory efficiency (VE/VCO2) was defined as the slope of the VE/VCO2 curve, calculated from beginning of exercise until peak effort. The minimal oxygen equivalent (EqO2 min) describes the minimal ratio of VE/VO2. S1, the aerobic slope of the VCO2/VO2-curve, was calculated by linear regression analysis including all (y;x) pairs of the VCO2–VO2 data points until reaching the anaerobic threshold. In patients not reaching the AT, s1 was calculated for the slope until the highest level of exercise and oxygen uptake that was measured (see Fig. 1).
a s1 depicts the initial slope of the VCO2/VO2-ratio, calculated by linear regression analysis including all (x;y) pairs of the VCO2–VO2 data points until reaching the anaerobic threshold. b example of a patient with poor exercise performance. The highest capable values of VCO2 and VO2 were used for analysis of s1
Patient follow-up and endpoint
All patients were followed at the heart failure clinic of the J. W. Goethe-University Hospital by telephone or personal interviews. The median follow-up period was 668 (range 2–1,229 days) days. Cardiovascular death, necessity for heart transplantation and/or rehospitalization due to worsening heart failure were defined as a combined endpoint. Events were documented by copies of discharge reports or certificates of death. JH and UFR followed the clinical follow-up blinded to the patients’ CPET results, JH performed statistical analysis of clinical follow-up and exercise results. AZ and IS reviewed the work.
Statistical analysis
Continuous variables are presented as mean values ± standard deviation. Discrete variables were compared using χ2-analysis. Continuous variables were compared by the non-parametric Mann–Whitney-test. Data from continuous variables depicted as boxplots show median and quartiles as a horizontal line in the box. Correlations were performed using bivariate Pearson’s correlations, presenting results as coefficients of correlation (r). Cumulative survival was calculated by Kaplan–Meier-analysis, differences between groups were compared with a log rank test. Cut off values, sensitivity and specificity were determined by receiver operating characteristic curve analysis. Stepwise forward Cox proportional hazard analysis determined the independent predictors of cardiac death and rehospitalization due to worsening heart failure. Only parameters with a univariate P-value ≤ 0.05 were included in the analysis. Independent relative risks (RR) are presented with 95% CI. P < 0.05 was considered statistically significant. The differences between Hazard ratios were calculated with a likelihood ratio test according to Wald, a P-value of <0.05 was considered significant. All statistical analyses were performed with the SPSS 12.0 (SPSS Inc., Chicago, IL) software package.
Results
Patient characteristics
Table 1 summarizes the clinical characteristics of the study cohort. 55% of patients had a history of hypertension, and 17% were diabetics. Global LVEF was moderately impaired (mean EF 41%, range 21%–69% by quantitative angiography), the median NT-proBNP-serum-levels were markedly increased.
All patients received antiplatelet therapy with aspirin, clopidogrel or both. 87% of patients were on ACE-inhibitors or ARB-agents, 88% on betablockers, 83% on statins and 33% of the patients on aldosterone antagonists. All patients were in clinically stable condition without symptoms of decompensated heart failure, when examined by CPET.
During the median follow-up of 668 days (range 2–1,229 days), five patients deceased and were classified as cardiovascular deaths. One patient underwent successful cardiac transplantation, one patient was referred to cardiac surgery for aneurysmectomy after anterior wall myocardial infarction. Seven patients had to be hospitalized due to worsening of heart failure. No patient was lost to follow up. Patients with and without events differed significantly with respect to age, family history of CAD, NYHA-class and NT-proBNP-levels (Table 1). Patients with events were older, had lower exercise tolerance and higher NT-proBNP-levels.
Cardiopulmonary exercise testing parameters
Patients without events performed better at CPET (Table 1); they achieved higher values for peak VO2 (17 ± 4 vs. 12 ± 3 ml/min/kg, P < 0.01) and peak oxygen pulse, whereas EqCO2min and EqO2min. were significantly lower in patients without events. The submaximal exercise parameter s1 was significantly lower among patients without events (0.83 ± 0.08 vs. 0.89 ± 0.09, P < 0.01). VE/VCO2 slope differed significantly between groups. The mean maximal heart rate was 117 ± 21 min, RER at peak 1.12 ± 0.11. Mean power at peak exercise was 94 ± 27 W. Ninty-five (92%) patients reached AT, 3 (3%) interrupted CPET before AT. In 2 (2%) patients, AT could not be determined adequately.
Interdependence of clinical, laboratory and exercise-dependent parameters
As expected, both global LVEF (r = −0.4, P < 0.01) and peak VO2 (r = −0.47, P < 0.01) correlated significantly with NT-proBNP serum levels (Fig. 2). In parallel, NYHA-class correlated with global LVEF (r = −0.31, P = 0.002), NT-proBNP serum level (r = 0.33, P = 0.001), peak VO2 (r = −0.51, P < 0.01) and EqCO2min (r = 0.42, P < 0.01). However, neither NYHA-class, global LVEF, NT-proBNP nor peak VO2 correlated significantly with s1.
Prediction of survival and adverse events by NT-proBNP, peak VO2 and s1
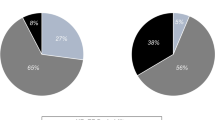
In order to evaluate the prognostic power of NT pro-BNP serum level, peak VO2 and s1, we performed a Kaplan–Meier-analysis for the occurrence of the combined clinical endpoint (cardiovascular death or progressive heart failure with the need of rehospitalization). All three analyzed parameters demonstrated significant discriminatory power (Fig. 3). As cut-off value for s1 used in Fig. 4, 0.87 as the value with the highest sensitivity (0.769) and specificity (0.644) was chosen. Regarding peak VO2, a cut-off value of ≤10 ml/min/kg (P < 0.001) was a better prognosticator of outcome compared to ≤14 ml/min/kg (P < 0.01, log-rank test). The superiority of ≤10 ml/min/kg compared to ≤14 ml/min/kg as a cut-off value is underscored by its higher sensitivity and specificity (sensitivity 0.69 and specificity 0.96 for peak VO2 ≤10 ml/min/kg, sensitivity 0.39 and specificity 0.69 for peak VO2 ≤14 ml/min/kg, Fig. 4). Besides the parameters described above, higher NYHA-class and age also correlated significantly with increased incidence of death and heart failure rehospitalization (Table 3).
Discriminatory power of NT-proBNP, s1 and peak VO2
The drawback of the Kaplan–Meier analysis is the requirement of a specific cut-off value. Analysis of receiver-operator curves (ROC) supplies additional information regarding overall discriminatory power of a parameter. Figure 4 and Table 3 demonstrate the ROC characteristics of peak VO2, s1 and NT-proBNP for the combined endpoint. Peak VO2 turned out by far as the weakest discriminatory parameter of all three, illustrated by the small area under the curve (AUC for peak VO2 0.188 [0.059–0.317], s1 0.717 [0.543–0.891] and NT-proBNP 0.778 [0.652–0.905], Table 2). Among submaximal CPET-parameters, VO2 at AT and VE/VCO2 also had lower under the curve values (VO2 at AT: 0.313 [0.144–0.482] and VE/VCO2: 0.635 [0.479–0.79]). This somewhat surprising finding results from the poor overall specificity of peak VO2, most likely related to a high number of false-positive results in patients with only submaximal effort.
Independent predictors of cardiovascular events
Finally, we performed a multivariate stepwise forward Cox regression analysis to identify independent predictors of the combined endpoint. Only NYHA-class and age (descripted as decades of patients’ age) were used as categorized variables. All continuous and categorized parameters, which showed statistical significance of less than 0.05 in the univariate analysis for outcome, were included into the stepwise forward Cox model. Only age (hazard ratio 1.163 [1.025–1.319]), peak VO2 (0.758 [0.588–0.978]) and s1 (1.141 [1.027–1.267]) remained as independent predictors of the combined endpoint (Table 3). Again, s1 was the strongest independent predictor of an unfavourable outcome among the three. VO2 AT as second submaximal CPET-parameter did not show significant predictive power in this model. When LVEF (univariate P = 0.07) was included, no significant changes in distribution of independent predictors occurred (data not shown). Similar findings were observed, when cardiac death was chosen as the single endpoint (data not shown).
Discussion
Prognostic relevance of cardiopulmonary exercise parameters
A substantial number of prognostically relevant CPET parameters have been previously established [8, 13, 15, 17, 21, 22, 35]. Table 4 provides an overview of important CPET-studies highlighting the significant ones with respect to the etiology of heart failure and pharmacological therapy. It appears obvious that most studies did not include patients being chronically treated with beta blockers, statins and ACE inhibitors to a high extent. Betablockers and other neurohumoral blockers [34] are well established to improve prognosis in patients with heart failure [1, 3, 5, 26–28, 32, 36]. Interestingly, there is controversy whether maximal effort during CPET is mandatory in order to predict prognosis [12, 14, 15]. Although peak VO2 itself can be affected by a variety of factors [8, 20, 29, 37], and other CPET-parameters offer even more reliable prognostic value [31], peak VO2 is still often regarded as an enduring gold standard for prognostic evaluation of CHF-patients. Nevertheless, a number of submaximal and motivation-independent parameters have been described and linked to prognosis (VO2 at AT [7], VE/VCO2 slope [8, 16], oxygen uptake efficiency slope (OUES) [2]). In the present study, peak VO2 turned out to be of significant prognostic power also in patients under the combined treatment with betablockers and ACE inhibitors/ARBs.
The fact that a lower cut off of ≤10 ml/min/kg of peak VO2 was associated with higher sensitivity and specificity than ≤14 ml/kg/min supports the assumption that in patients under beta blockers, lower peak VO2 threshold values appear to be more appropriate to predict prognosis [25].
Physiological and prognostic meaning of s1
S1 represents the slope of increasing CO2-elimination and oxygen uptake before reaching the anaerobic threshold. The respiratory exchange ratio (RER) is a measure of the CO2/O2 ratio as well, but is only used for single time points. In contrast, s1 is calculated over the entire time span of aerobic exercise by regression analysis and, therefore, provides dynamic information about altered gas exchange in heart failure patients at lower exercise levels. In patients with heart failure, the ventilatory response and increasing CO2-production is already impaired at lower levels of exercise. According to Bohr’s formula on dead space ventilation, EqCO2 increases concomitantly to rising dead space ventilation. This happens as a result of (a) higher breathing frequency with lower tidal volumes and (b) pulmonary hypoperfusion due to reduced cardiac output in patients with heart failure. As ventilatory response to exercise can be influenced by many factors especially at the beginning of effort (e.g. individual exercise status, hyperventilation and effort), minute ventilation (VE) can confound many CPET parameters such as VO2 at AT and VE/VCO2, all derived from measurement of VE. In contrast, s1 should be largely independent from the influence of ventilation: Polynomic calculation of the s1-slope contains division of ventilation values for both VCO2 and VO2, eliminating the potentially interacting and pathologically altered ventilatory volumes for both equivalents, CO2 and O2. Patients with events and unfavourable outcome had higher s1-levels, indicating incremental proportions of CO2-production versus oxygen-uptake over time under aerobic exercise conditions. To our surprise, s1 was the strongest independent predictor of outcome in the multivariate analysis including important clinical (NYHA-class, LVEF, NT-proBNP) and exercise-related parameters (peak VO2, VE/VCO2 slope). The overall discriminatory power of s1 was better than that of peak VO2 and comparable to NT-proBNP. Importantly, whereas s1 did not yield additional prognostic information in patients with peak VO2 ≤ 10 ml/min/kg, s1 might be specifically powerful to discriminate clinical outcome in patients with peak VO2 > 10- ≤ 14 ml/min/kg. Thus, s1 appears to be specifically useful to distinguish between patients already at their exercise limit or those with reduced effort. Based on our data, we propose a possible algorithm to identify patients at risk using the combined parameters of peak VO2 and s1 (Fig. 5). However, prognostic value of s1 has to be substantiated in larger prospective trials.
Study limitations
Although the present work is an analysis of stable post-myocardial infarction heart failure patients, the described collective of patients consists of rather young patients with an only moderately impaired LVEF and a low rate of relevant comorbidities. The number of events during follow-up is also rather limited. Thus, based on our data and study population, we cannot provide a definite threshold for s1 yet. Further prospective validation of s1 will be necessary in a larger cohort of patients with more severe heart failure.
Fasting and glycogen depletion, which alters s1-levels in healthy men [10], could also have influenced the results of our study. Nevertheless, none of our patients underwent CPET after fasting episodes or heavy muscular work.
Finally, our exercise protocol, a modified Bruce protocol [6], might partially not correspond with protocols which are used in other publications. Therefore, the influence of different exercise protocols on s1-levels remains to be elucidated. Whether s1 also plays a role in evaluation of other pathologic conditions such as the diastolic dysfunction, pulmonary hypertension or the evaluation of perioperative risk, also remains unclear.
Taken together, the aerobic VCO2/VO2-slope, s1, is an important independent predictor of death and progression of heart failure in patients with compromised systolic function ≥3 months after an acute myocardial infarction. S1 appears to be specifically useful to predict clinical outcome in patients unable or unwilling to achieve their peak VO2 during exercise testing, and, thus, might provide important complimentary information during exercise testing of patients with heart failure.
Abbreviations
- AT:
-
Anaerobic threshold
- AUROC:
-
Area under the receiver operating characteristic curve
- ACE:
-
Angiotensin converting enzyme
- ARB:
-
Angiotensin receptor blocker
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- CAD:
-
Coronary artery disease
- CHF:
-
Chronic heart failure
- CPET:
-
Cardiopulmonary exercise test
- CI:
-
Confidence interval
- EqCO2 :
-
Ventilatory equivalent for CO2-exhalation
- EqO2 :
-
Ventilatory equivalent for O2-inhalation
- EqO2 min, EqCO2 min:
-
Minimal ventilatory equivalents for O2- and Co2-exchange
- LVEF:
-
Left ventricular ejection fraction
- Peak VO2 :
-
Peak oxygen uptake
- Peak O2 pulse:
-
Peak oxygen uptake, adjusted to corresponding heart rate
- RER:
-
Respiratory exchange ratio
- RR:
-
Relative risk
- S1:
-
Initial slope of the VCO2/VO2-curve
- NYHA:
-
New York heart association
- VE:
-
Minute ventilation
- VE/VCO2 :
-
Slope of the VE/VCO2 curve
- VO2 AT:
-
Oxygen uptake at the anaerobic threshold
References
(1999) The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomised trial. Lancet 353:9–13
Baba R, Nagashima M, Goto M, et al (1996) Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol 28:1567–1572
Basat O, Ucak S, Seber S, Oztekin E, Altuntas Y (2006) After myocardial infarction carvedilol improves insulin resistance compared to metoprolol. Clin Res Cardiol 95:99–104
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60:2020–2027
Bohm M, Werner N, Kindermann M (2006) Drug treatment of chronic heart failure. Clin Res Cardiol 95(Suppl 4):36–54; quiz 55–56
Bruce RA, Blackmon JR, Jones JW, Strait G (1963) Exercising testing in adult normal subjects and cardiac patients. Pediatrics 32(suppl):742–756
Buller NP, Poole-Wilson PA (1988) Extrapolated maximal oxygen consumption: a new method for the objective analysis of respiratory gas exchange during exercise. Br Heart J 59:212–217
Chua TP, Ponikowski P, Harrington D, et al (1997) Clinical correlates and prognostic significance of the ventilatory response to exercise in chronic heart failure. J Am Coll Cardiol 29:1585–1590
Cohn JN, Johnson GR, Shabetai R, et al (1993) Ejection fraction, peak exercise oxygen consumption, cardiothoracic ratio, ventricular arrhythmias, and plasma norepinephrine as determinants of prognosis in heart failure. the V-HeFT VA Cooperative Studies Group. Circulation 87:VI5–VI16
Cooper CB, Beaver WL, Cooper DM, Wasserman K (1992) Factors affecting the components of the alveolar CO2 output-O2 uptake relationship during incremental exercise in man. Exp Physiol 77:51–64
Cowie MR, Mosterd A, Wood DA, et al (1997) The epidemiology of heart failure. Eur Heart J 18:208–225
Davies LC, Francis DP, Piepoli M, Scott AC, Ponikowski P, Coats AJ (2000) Chronic heart failure in the elderly: value of cardiopulmonary exercise testing in risk stratification. Heart 83:147–151
Davies LC, Wensel R, Georgiadou P, et al (2006) Enhanced prognostic value from cardiopulmonary exercise testing in chronic heart failure by non-linear analysis: oxygen uptake efficiency slope. Eur Heart J 27:684–690
Francis DP, Shamim W, Davies LC, et al (2000) Cardiopulmonary exercise testing for prognosis in chronic heart failure: continuous and independent prognostic value from VE/VCO(2) slope and peak VO(2). Eur Heart J 21:154–161
Gitt AK, Wasserman K, Kilkowski C, et al (2002) Exercise anaerobic threshold and ventilatory efficiency identify heart failure patients for high risk of early death. Circulation 106:3079–3084
Ingle L, Goode K, Carroll S, et al (2007) Prognostic value of the VE/VCO2 slope calculated from different time intervals in patients with suspected heart failure. Int J Cardiol 118:350–355
Kleber FX, Vietzke G, Wernecke KD, et al (2000) Impairment of ventilatory efficiency in heart failure: prognostic impact. Circulation 101:2803–2809
Krumholz HM, Chen YT, Wang Y, Vaccarino V, Radford MJ, Horwitz RI (2000) Predictors of readmission among elderly survivors of admission with heart failure. Am Heart J 139:72–77
Lavie CJ, Milani RV, Mehra MR (2004) Peak exercise oxygen pulse and prognosis in chronic heart failure. Am J Cardiol 93:588–593
Lipkin DP, Jones DA, Round JM, Poole-Wilson PA (1988) Abnormalities of skeletal muscle in patients with chronic heart failure. Int J Cardiol 18:187–195
Mancini DM, Eisen H, Kussmaul W, Mull R, Edmunds LH Jr, Wilson JR (1991) Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation 83:778–786
Mudge GH, Goldstein S, Addonizio LJ, et al (1993) 24th Bethesda conference: cardiac transplantation. Task force 3: recipient guidelines/prioritization. J Am Coll Cardiol 22:21–31
Myers J, Gullestad L, Vagelos R, et al (2000) Cardiopulmonary exercise testing and prognosis in severe heart failure: 14 ml/kg/min revisited. Am Heart J 139:78–84
Norozi K, Wessel A, Buchhorn R, et al (2007) Is the ability index superior to the NYHA classification for assessing heart failure?: comparison of two classification scales in adolescents and adults with operated congenital heart defects. Clin Res Cardiol 96:542–547
O’Neill JO, Young JB, Pothier CE, Lauer MS (2005) Peak oxygen consumption as a predictor of death in patients with heart failure receiving beta-blockers. Circulation 111:2313–2318
Packer M, Fowler MB, Roecker EB, et al (2002) Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation 106:2194–2199
Peters-Klimm F, Muller-Tasch T, Schellberg D, et al. (2007) Guideline adherence for pharmacotherapy of chronic systolic heart failure in general practice: a closer look on evidence-based therapy. Clin Res Cardiol 97(4):244–252
Pitt B, Williams G, Remme W, et al (2001) The EPHESUS trial: eplerenone in patients with heart failure due to systolic dysfunction complicating acute myocardial infarction. Eplerenone post-AMI heart failure efficacy and survival study. Cardiovasc Drugs Ther 15:79–87
Poole-Wilson PA, Buller NP, Lipkin DP (1988) Regional blood flow, muscle strength and skeletal muscle histology in severe congestive heart failure. Am J Cardiol 62:49E–52E
Reybrouck T, Mertens L, Schepers D, Vinckx J, Gewillig M (1997) Assessment of cardiorespiratory exercise function in obese children and adolescents by body mass-independent parameters. Eur J Appl Physiol Occup Physiol 75:478–483
Robbins M, Francis G, Pashkow FJ, et al (1999) Ventilatory and heart rate responses to exercise: better predictors of heart failure mortality than peak oxygen consumption. Circulation 100:2411–2417
Schuler J, Maier B, Behrens S, Thimme W (2006) Present treatment of acute myocardial infarction in patients over 75 years–data from the Berlin myocardial infarction registry (BHIR). Clin Res Cardiol 95:360–367
Shakar SF, Lowes BD, Lindenfeld J, et al (2004) Peak oxygen consumption and outcome in heart failure patients chronically treated with beta-blockers. J Card Fail 10:15–20
Simon T, Becker R, Voss F, et al (2008) Elevated B-type natriuretic peptide levels in patients with nonischemic cardiomyopathy predict occurrence of arrhythmic events. Clin Res Cardiol 97(5):306–309
Stevenson LW (1996) Selection and management of candidates for heart transplantation. Curr Opin Cardiol 11:166–173
Voller H (2006) Significance of changes in habits followed by risk reduction. Clin Res Cardiol 95(Suppl 6):VI6–VI11
Yasaka Y, Yamabe H, Yokoyama M (1997) Dependence of peak oxygen uptake on oxygen transport capacity in chronic heart failure: comparison of graded protocol and fixed protocol. Int J Cardiol 59:149–156
Zugck C, Haunstetter A, Kruger C, et al (2002) Impact of beta-blocker treatment on the prognostic value of currently used risk predictors in congestive heart failure. J Am Coll Cardiol 39:1615–1622
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Honold, J., Geiger, L., Assmus, B. et al. The initial slope of the VCO2/VO2-curve (s1) in cardiopulmonary exercise testing is a strong and independent predictor of outcome in patients with previous myocardial infarction. Clin Res Cardiol 97, 882–890 (2008). https://doi.org/10.1007/s00392-008-701-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-008-701-6