Abstract
Background
Recanalization of the culprit lesion is the main goal of primary angioplasty for acute ST-segment elevation myocardial infarction (STEMI). Patients presenting with acute myocardial infarction and multivessel disease are, therefore, usually subjected to staged procedures, with the primary percutaneous coronary intervention (PCI) confined to recanalization of the infarct-related artery (IRA). Theoretically at least, early relief of stenoses of non-infarctrelated arteries could promote collateral circulation, which could help to limit the infarct size. However, the safety and feasibility of such an approach has not been adequately established.
Methods
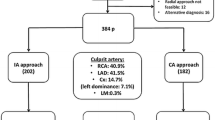
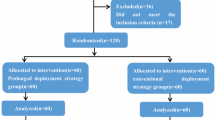
In this single-center prospective study we examined 73 consecutive patients who had an acute STEMI and at least one or more lesions ≥ 70% in a major epicardial vessel other than the infarctrelated artery. In the first 28 patients, forming the multi-vessel (MV) PCI group, all lesions were treated during the primary procedure. In the following 45 patients, forming the culprit-only (CO) PCI group, only the culprit lesion was treated during the initial procedure, followed by either planned-staged or ischemiadriven revascularization of the non-culprit lesions. Fluoroscopy time and contrast dye amount were compared between both groups, and patients were followed up for one year for major adverse cardiac events (MACE) and other significant clinical events.
Results
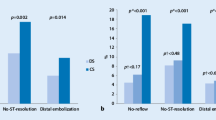
The two groups were well balanced in terms of clinical characteristics, number of diseased vessels and angiographic characteristics of the culprit lesion. In the MV-PCI group, 2.51 lesions per patient were treated using 2.96 ± 1.34 stents (1.00 lesions and 1.76 ± 1.17 stents in the CO-PCI group, both p < 0.001). The fluoroscopy time increased from 10.3 (7.2–16.9) min in the CO-PCI group to 12.5 (8.5–19.3) min in the MV-PCI group (p = 0.22), and the amount of contrast used from 200 (180–250) ml to 250 (200–300) ml, respectively (p = 0.16). Peak CK and CK-MB were significantly lower in patients of the MV-PCI group (843 ± 845 and 135 ± 125 vs 1652 ± 1550 and 207 ± 155 U/l, p < 0.001 and 0.01, respectively). Similar rates of major adverse cardiac events at one year were observed in the two groups (24% and 28% in multi-vessel and culprit treatment groups, p = 0.73). The incidence of new revascularization in both infarct- and noninfarct-related arteries was also similar (24% and 28%, respectively, p = 0.73).
Conclusion
We may state from this limited experience that a multi-vessel stenting approach for patients with acute STEMI and multi-vessel disease is feasible and probably safe during routine clinical practice. Our data suggest that this approach may help to limit the infarct size. However, larger studies, perhaps using drug-eluting stents, are still needed to further evaluate the safety and efficiency of this procedure, and whether it is associated with a lower need of subsequent revascularization and lower costs.
Similar content being viewed by others
References
Califf RM, Bengtson JR (1994) Cardiogenic shock. N Engl J Med 330:1724–1730
Maroko PR, Braunwald E (1973) Modification of myocardial infarct size after coronary occlusion. Ann Intern Med 79:720–733
Grines CL, Cox DA, Stone GW et al (1999) Coronary angioplasty with or without stent implantation for acute myocardial infarction. Stent Primary Angioplasty in Myocardial Infarction Group. N Engl J Med 341:1949
De Wood MA, Spores J, Notske RN et al (1980) Prevalence of total coronary artery occlusion during the early hours of transmural myocardial infarction. N Engl J Med 303:897–902
Martin GV, Kennedy JW (1994) Choice of thrombolytic agent. In: Julian D, Braunwald E (eds) Management of Acute Myocardial Infarction. WB Saunders, London, pp 71–105
Silber S, Albertsson P, Avilés FF et al (2005) Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur Heart J 26:804–847
Smith SC Jr, Feldman TE, Hirshfeld JW Jr et al: ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines (ACC/ AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). American College of Cardiology Web Site. Available at: http://www.acc.org/ clinical/guidelines/percutaneous/ update/index_rev.pdf
Cook S, Walker A, Hügli O et al (2007) Percutaneous coronary interventions in Europe. Prevalence, numerical estimates, and projections based on data up to 2004. Clin Res Cardiol 96:375–382
Lane GE, Holmes DR (2003) The modern strategy for cardiogenic shock. In: Cannon CP (ed) Management of Acute Coronary Syndromes. Humana Press, Totowa, NJ, pp 603–652
Corpus RA, House JA, Marso SP et al (2004) Multivessel percutaneous intervention in patients with multivessel disease and acute myocardial infarction. Am Heart J 148 (3):493–500
Di Mario C, Sansa M, Airoldi F et al (2004) Single versus multivessel treatment during primary angioplasty: results of the multicentre randomized HEpacoatTM for culprit or multivessel stenting for Acute Myocardial Infarction (HELP AMI) Study. Int J Cardiovasc Intervent 6:128–133
Roe MT, Cura FA, Joski PS et al (2001) Initial experience with multivessel percutaneous coronary intervention during mechanical reperfusion for acute myocardial infarction. Am J Cardiol 88:170–173
Serruys PW, Ong ATL, Morice MC et al (2005) Arterial revascularization therapies part II – Sirolimus-Eluting Stents for the treatment of patients with multivessel de novo coronary artery lesions. EuroInterv 2:147–156
Kaiser C, Brunner-La Rocca HP, Buser PT et al (2005) Incremental costeffectiveness of drug-eluting stents compared with a third generation bare-metal stent in a real world setting: randomized Basel Stent Kosten Effektivitäts Trial (BASKET). Lancet 366:921–992
Hedström E, Astrom-Olsson K, Ohlin H et al (2007) Peak CKMB and cTnT accurately estimates myocardial infarct size after reperfusion. Scand Cardiovasc J 41:44–50
Stone PH, Raabe DS, Jaffe AS et al (1988) Prognostic significance of location and type of myocardial infarction: independent adverse outcome associated with anterior location. J Am Coll Cardiol 11:453–463
Assali AR, Teplitsky I, Ben-Dor I et al (2007) Prognostic importance of right ventricular infarction in an acute myocardial infarction cohort referred for contemporary percutaneous reperfusion therapy. Am Heart J 153:231–237
Pasceri V, Patti G, Speciale G et al (2007) Meta-analysis of clinical trials on use of drug eluting stents for treatment of acute myocardial infarction. Am Heart J 153:749–754
Carlsson J, von Wagenheim B, Linder R et al (2007) Is late stent thrombosis in drug-eluting stents a real clinical issue? A single-center experience and review of the literature. Clin Res Cardiol 96:86–93
Bavry AA, Bhatt DL (2007) Acute myocardial infarction and drug-eluting stents: a green light for their use or time for measured restraint? Am Heart J 153:719–721
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by an educational grant from Guidant, Germany
Rights and permissions
About this article
Cite this article
Khattab, A.A., Abdel-Wahab, M., Röther, C. et al. Multi-vessel stenting during primary percutaneous coronary intervention for acute myocardial infarction. Clin Res Cardiol 97, 32–38 (2008). https://doi.org/10.1007/s00392-007-0570-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-007-0570-4