Abstract
Purpose
Patient-reported outcomes are essential to patient-centered cancer care. We sought to determine the relationships between colorectal cancer (CRC) diagnosis and trends in self-reported general health status (GHS) and mental health status (MHS) among racial/ethnic groups.
Methods
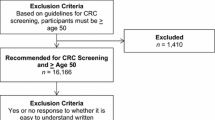
We used population-based Surveillance, Epidemiology, and End Results (SEER)-Consumer Assessment of Healthcare Providers and Systems (CAHPS) data to identify CRC patients diagnosed from 1996 to 2011 who reported GHS and/or MHS on a CAHPS survey within 6 years before or after diagnosis and were 65 or older at survey completion. Multivariable logistic regression assessed relationships of patient race/ethnicity and CRC diagnosis with the odds of reporting fair or poor GHS or MHS.
Results
Five thousand five hundred forty-five patients reported GHS and/or MHS within 6 years before CRC diagnosis and 4,604 reported GHS and/or MHS within 6 years after diagnosis. 80.9% were non-Hispanic white (NHW), 7.1% were non-Hispanic black (NHB), 6.7% were Hispanic, and 5.3% were non-Hispanic Asian. Being diagnosed with CRC was associated with increased odds of reporting fair or poor GHS (OR = 1.55, 95% CI = 1.40–1.72) and MHS (OR = 1.33, 95% CI = 1.13–1.58). For GHS, this trend held for all race/ethnicities except NHBs, and for MHS, this trend held for NHWs and Hispanics only.
Conclusion
CRC diagnosis is an important driver of increased likelihood of fair and poor GHS and MHS, but the relationship is complicated by effect modification by race/ethnicity. Efforts to further understand the race/ethnicity-specific relationships between CRC diagnosis and declines in GHS and MHS are necessary to promote equitable care for all patients.


Similar content being viewed by others
Data availability
This study used the linked SEER-CAHPS data resource. The interpretation and reporting of these data are the sole responsibility of the authors.
References
Gotay CC, Kawamoto CT, Bottomley A, Efficace F (2008) The prognostic significance of patient-reported outcomes in cancer clinical trials. J Clin Oncol 26:1355–1363
Valderas JM, Kotzeva A, Espallargues M, Guyatt G, Ferrans CE, Halyard MY, Revicki DA, Symonds T, Parada A, Alonso J (2008) The impact of measuring patient-reported outcomes in clinical practice: a systematic review of the literature. Qual Life Res 17:179–193
Mawani FN, Gilmour H (2010) Validation of self-rated mental health
Santana MJ, Manalili K, Jolley RJ, Zelinsky S, Quan H, Lu M (2018) How to practice person-centred care: a conceptual framework. Heal Expect 21:429–440
Chen J, Ou L, Hollis SJ (2013) A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Serv Res. https://doi.org/10.1186/1472-6963-13-211
Lavallee DC, Chenok KE, Love RM, Petersen C, Holve E, Segal CD, Franklin PD (2016) Incorporating patient-reported outcomes into health care to engage patients and enhance care. Health Aff 35:575–582
DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P (2006) Mortality prediction with a single general self-rated health question: a meta-analysis. J Gen Intern Med 21:267–275
Dwyer-Lindgren L, Mackenbach JP, van Lenthe FJ, Mokdad AH (2017) Self-reported general health, physical distress, mental distress, and activity limitation by US county, 1995–2012. Popul Health Metr. https://doi.org/10.1186/s12963-017-0133-5
Ahmad F, Jhajj AK, Stewart DE, Burghardt M, Bierman AS (2014) Single item measures of self-rated mental health: a scoping review. BMC Health Serv Res. https://doi.org/10.1186/1472-6963-14-398
Wu S, Wang R, Zhao Y, Ma X, Wu M, Yan X, He J (2013) The relationship between self-rated health and objective health status: a population-based study. BMC Public Health 13:1–9
Gandhi K, Lim E, Davis J, Chen JJ (2020) Racial-ethnic disparities in self-reported health status among US adults adjusted for sociodemographics and multimorbidities, National Health and Nutrition Examination Survey 2011–2014. Ethn Heal 25:65–78
Doll KM, Pinheiro LC, Reeve BB (2017) Pre-diagnosis health-related quality of life, surgery, and survival in women with advanced epithelial ovarian cancer: a SEER-MHOS study. Gynecol Oncol 144:348–353
Pinheiro LC, Zagar TM, Reeve BB (2017) The prognostic value of pre-diagnosis health-related quality of life on survival: a prospective cohort study of older Americans with lung cancer. Qual Life Res 26:1703–1712
Klapheke AK, Keegan THM, Ruskin R, Cress RD (2020) Pre-diagnosis health-related quality of life and survival in older women with endometrial cancer. Support Care Cancer 28:4901–4909
Moseholm E, Rydahl-Hansen S, Overgaard D, Wengel HS, Frederiksen R, Brandt M, Lindhardt B (2016) Health-related quality of life, anxiety and depression in the diagnostic phase of suspected cancer, and the influence of diagnosis. Health Qual Life Outcomes. https://doi.org/10.1186/s12955-016-0484-9
Folker AP, Hegelund ER, Mortensen EL, Wimmelmann CL, Flensborg-Madsen T (2019) The association between life satisfaction, vitality, self-rated health, and risk of cancer. Qual Life Res 28:947–954
Secord AA, Coleman RL, Havrilesky LJ, Abernethy AP, Samsa GP, Cella D (2015) Patient-reported outcomes as end points and outcome indicators in solid tumours. Nat Rev Clin Oncol 12:358–370
Petrick JL, Foraker RE, Kucharska-Newton AM, Reeve BB, Platz EA, Stearns SC, Han X, Windham BG, Irwin DE (2014) Trajectory of overall health from self-report and factors contributing to health declines among cancer survivors. Cancer Causes Control 25:1179–1186
Williams K, Jackson SE, Beeken RJ, Steptoe A, Wardle J (2016) The impact of a cancer diagnosis on health and well-being: a prospective, population-based study. Psychooncology 626–632
Pinheiro LC, Wheeler SB, Chen RC, Mayer DK, Lyons JC, Reeve BB (2015) The effects of cancer and racial disparities in health-related quality of life among older Americans: a case-control, population-based study. Cancer 121:1312–1320
Siegel RL, Miller KD, Fedewa SA, Ahnen DJ, Meester RGS, Barzi A, Jemal A (2017) Colorectal cancer statistics, 2017. CA Cancer J Clin 67:177–193
Irby K, Anderson WF, Henson DE, Devesa SS (2006) Emerging and widening colorectal carcinoma disparities between blacks and whites in the United States (1975–2002). Cancer Epidemiol Biomarkers Prev 15:792–797
May FP, Glenn BA, Crespi CM, Ponce N, Spiegel BMR, Bastani R (2017) Decreasing black-white disparities in colorectal cancer incidence and stage at presentation in the United States. Cancer Epidemiol Biomarkers Prev 26:762–768
Chan C, Lopez A, Castaneda G, Bhuket T, Liu B, Yee S, Irwin D, Wong RJ (2017) Black patients with colorectal cancer have more advanced cancer stage at time of diagnosis: a community-based safety-net hospital experience. J Community Health 42:724–729
Pergolotti M, Deal AM, Williams GR, Bryant AL, Bensen JT, Muss HB, Reeve BB (2017) Activities, function, and health-related quality of life (HRQOL) of older adults with cancer. J Geriatr Oncol 8:249–254
Jayadevappa R, Johnson JC, Chhatre S, Wein AJ, Malkowicz SB (2007) Ethnic variation in return to baseline values of patient-reported outcomes in older prostate cancer patients. Cancer 109:2229–2238
Chawla N, Urato M, Ambs A et al (2015) Unveiling SEER-CAHPS®: a new data resource for quality of care research. J Gen Intern Med 30:641–650
Bombak AE (2013) Self-rated health and public health: a critical perspective. Front Public Heal. https://doi.org/10.3389/fpubh.2013.00015
Zaslavsky AM, Cleary PD (2002) Dimensions of plan performance for sick and healthy members on the Consumer Assessments of Health Plans Study 2.0 survey. Med Care 40:951–964
Alcalá HE (2014) Differential mental health impact of cancer across racial/ethnic groups: findings from a population-based study in California. BMC Public Health. https://doi.org/10.1186/1471-2458-14-930
Kurtz ME, Kurtz JC, Stommel M, Given CW, Given B (2002) Predictors of depressive symptomatology of geriatric patients with colorectal cancer: a longitudinal view. Support Care Cancer 10:494–501
Fleishman JA, Zuvekas SH (2007) Global self-rated mental health: associations with other mental health measures and with role functioning. Med Care 45:602–609
Reese AM, Thorpe RJ, Bell CN, Bowie JV, La Veist TA (2012) The effect of religious service attendance on race differences in depression: findings from the EHDIC-SWB study. J Urban Heal 89:510–518
Schnittker J, Freese J, Powell B (2000) Nature, nurture, neither, nor: black-white differences in beliefs about the causes and appropriate treatment of mental illness. Soc Forces 78:1101–1132
Bell C, Thorpe R, LaVeist T (2018) The role of social context in racial disparities in self-rated health. J Urban Health 95:13–20
Karliner LS, Hwang ES, Nickleach D, Kaplan CP (2011) Language barriers and patient-centered breast cancer care. Patient Educ Couns 84:223–228
U.S. Census Bureau QuickFacts: United States. https://www.census.gov/quickfacts/fact/table/US/PST045221. Accessed 3 Mar 2022
Number of persons by race and Hispanic ethnicity for SEER participants - SEER Registries. https://seer.cancer.gov/registries/data.html#a6. Accessed 11 Aug 2021
Acknowledgements
The authors acknowledge the efforts of the National Cancer Institute; the Centers for Medicare & Medicaid Services; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-CAHPS data resource.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by all authors. The first draft of the manuscript was written by Navarro, Barzi, and Farias. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This research was granted exempt status by the Institutional Review Board of the University of Texas Health Sciences Center at Houston.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Navarro, S., Barzi, A., Jiao, X. et al. Temporal trends in self-reported general and mental health status among colorectal cancer patients: racial/ethnic disparities in a population-based analysis. Int J Colorectal Dis 37, 1073–1085 (2022). https://doi.org/10.1007/s00384-022-04139-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04139-1