Abstract
Purpose
To evaluate long-term outcomes of pure esophageal atresia (EA) repair with preservation of native esophagus.
Methods
Infants with pure EA treated at our institution (2000–2010) and with minimum 5-year follow-up were reviewed (REB:1000046653). Data analysed included demographics, management and outcomes and are reported as mean ± SD/median (range).
Results
Of 185 infants with EA, 12 (7 %) had pure EA (gestational age: 36 ± 2.4 weeks, birth weight: 2353 ± 675 g). Ten had associated anomalies, including trisomy-21 (n = 2) and duodenal atresia (n = 1). Surgery: 1 patient (short gap) underwent primary thoracoscopic anastomosis, 11 had gastrostomy (Stamm, n = 5; image-guided, n = 6) as initial procedure. At definitive repair (age: 128 ± 91 days; weight 5.5 ± 2.3 kg): ten had primary anastomosis and 1 had Collis gastroplasty. No patient had esophageal replacement surgery. Outcomes: three patients had gastrostomy dehiscence requiring re-operation. At post-operative esophagram, seven had anastomotic leak successfully treated conservatively. Seven patients developed strictures requiring balloon dilatations (median two dilatations, range 1–10), six received antireflux surgery. At 7-year follow-up (range 5–15 years), all patients had the gastrostomy closed and were on full oral feeds.
Conclusions
The management of pure EA continues to be challenging. The preservation of native esophagus is possible with significant morbidity. The long-term outcomes are favourable.

Similar content being viewed by others
References
Harmon CM, Coran AG (1998) Congenital anomalies of the esophagus. In: St Louis KY (ed) Pediatric Surgery, vol 5. Elsevier Science Health Science Division, Oxford
Gross RE (1953) Surgery of infancy and childhood. WB Sauders, Philadelphia
Bagolan P, Iacobelli BD, De Angelis P et al (2004) Long gap esophageal atresia and esophageal replacement: moving toward a separation? J Pediatr Surg 39:1084–1090
Sri Paran T, Decaluwe D, Corbally M et al (2007) Long-term results of delayed primary anastomosis for pure oesophageal atresia: a 27-year follow up. Pediatr Surg Int 23:647–651
Holland AJA, Ron O, Pierro A et al (2009) Surgical outcomes of esophageal atresia without fistula for 24 years at a single institution. J Pediatr Surg 44:1928–1932
Burjonrappa S, Thiboutot E, Castilloux J et al (2010) Type A esophageal atresia: a critical review of management strategies at a single center. J Pediatr Surg 45:865–871
Ein SH, Shandling B, Heiss K (1993) Pure esophageal atresia: outlook in the 1990. J Pediatr Surg 28:1147–1150
Ein SH, Shandling B (1994) Pure esophageal atresia: a 50-year review. J Pediatr Surg 9:1208–1211
Kunisaki SM, Bruch SW, Hirschl RB et al (2014) The diagnosis of fetal esophageal atresia and its implications on perinatal outcome. Pediatr Surg Int 30:971–977
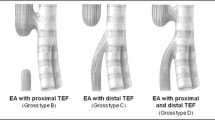
Holder TM, Cloud DT, Lewis JE Jr et al (1964) Esophageal atresia and tracheoesophageal fistula. A survey of its members by the Surgical Section of the American Academy of Pediatrics. Pediatrics 34:542–549
Zamiara P, Thomas KE, Connolly BL et al. (2015) Long-term burden of care and radiation exposure in survivors of esophageal atresia. J Pediatr Surg 50:1686–1690
Zani A, Eaton S, Hoellwarth M et al (2014) International survey on the management of esophageal atresia. Eur J Pediatr Surg 24:3–8
Friedmacher F, Puri P (2012) Delayed primary anastomosis for management of long-gap esophageal atresia: a meta-analysis of complications and long-term outcome. Pediatr Surg Int 28:899–906
Puri P, Blake N, O’Donnel B et al (1981) Delayed primary anastomosis following spontaneous growth of esophageal segments in esophageal atresia. J Pediatr Surg 16:180–183
Aziz D, Shiller D, Gerstle JT et al (2003) Can long-gap esophageal atresia be safely managed at home while awaiting anastomosis. J Pediatr Surg 5:705–708
Aziz D, Chait P, Kreichmn F et al (2004) Image-guided percutaneous gastrostomy in neonates with esophageal atresia. J Pediatr Surg 11:1648–1650
Spitz L (2006) Esophageal atresia. Lesson I have learned in a 40-year experience. J Pediatr Surg 41:1635–1640
Kluth D (1976) Atlas of esophageal atresia. J Pediatr Surg 11:901–919
Sanal M, Haeussler B, Tabareli W et al (2007) Pure esophageal atresia with normal outer appearance: case report. J Pediatr Surg 42:E1–E3
Foker JE, Linden BC, Boyle EM et al (1997) Development of a true primary repair for the full spectrum of esophageal atresia. Ann Surg 226:533–543
Foker JE, Kendall Krosch TC, Catton K et al (2009) Long-gap esphageal atresia treated by growth induction: the biological potential and early follow-up results. Semin Pediatr Surg 18:23–29
Bobanga ID, Barksdale EM (2015) Foker technique for the management of pure esophageal atresia: long-term outcomes at a single institution. Eur J Pediatr Surg [Epub ahead of print] PubMed PMID: 25774957
Lobe TE, Rothemberg SS, Waldshmitt J et al (1999) Thoracoscopic repair of esophageal atresia in an infant: a surgical first. Pediatr Endosurg Innov Tech 3:141–148
MacKinlay GA (2009) Esophageal atresia surgery in the 21st century. Seminars Pediatr Surg 18:20–22
Collis JL (1957) An operation for hiatus hernia with short oesophagus. Thorax 12:181–188
Al-Shanafey S, Harvey J (2008) Long gap esophageal atresia: an Australian experience. J Pediatr Surg 43:597–601
Ng J, Loukogeorgakis SP, Pierro A et al (2014) Comparison of minimally invasive and open gastric transposition in children. J Laparoendosc Adv Surg Tech 24:742–749
Thakkar HS, Cooney J, Kumar N et al (2014) Measured gap lenght and outcomes in oesophageal atresia. J Pediatr Surg 49:1343–1346
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zani, A., Cobellis, G., Wolinska, J. et al. Preservation of native esophagus in infants with pure esophageal atresia has good long-term outcomes despite significant postoperative morbidity. Pediatr Surg Int 32, 113–117 (2016). https://doi.org/10.1007/s00383-015-3821-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3821-x