Abstract
Necrotizing enterocolitis (NEC) is a serious condition with a high morbidity and mortality commonly affecting premature babies. Data for the impact of the long-term disease burden in developing countries are limited although poor long-term outcome of surgically managed patients has been shown in terms of increased risk of neurodevelopmental delay, increased infectious disease burden and abnormal neurological outcomes in the developed world.
Purpose
To evaluate the long-term outcome of a pre-human immunodeficiency virus pandemic NEC cohort to characterize common risk factors and outcome in a developing world setting.
Methods
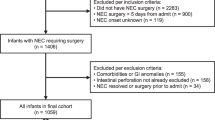
A retrospective review of medical records was carried out on a cohort of 128 premature neonates with surgical NEC (1992–1995). Morbidity, mortality and long-term outcome were evaluated.
Results:
Data for 119 of 128 sequentially managed neonates with surgically treated NEC was available. Mean gestational age was 32 weeks and average birth weight was 1,413 g. Early (30-day postoperative) survival was 69% (n = 82) overall and 71% in the <1,500 g birth weight group (n = 68; 53%). Overwhelming sepsis (n = 16) or pan-intestinal necrosis (n = 18) accounted for most of the early deaths. Late deaths (>30 days postoperatively, n = 22) resulted from short bowel syndrome (5), sepsis (9), intraventricular hemorrhage (1) and undetermined causes (7). On follow-up (mean follow-up 39 months, 30 for >2 years), long-term mortality increased to 50%. Late surgical complications included late colonic strictures (9), incisional hernias (2) and adhesive bowel obstruction (3). Fifteen patients had short bowel syndrome, of which 10 (66%) survived. Of the long-term survivors, 8 (20%) had severe neurological deficits and 20 (49%) had significant neurodevelopmental delay. Neurological deficits included severe auditory impairment [5 (12%)] and visual impairment [4 (10%)]. Recurrent infections and gastrointestinal tract complaints requiring hospital admission occurred in 16 (39%) of survivors.
Conclusion
Necrotizing enterocolitis in premature infants impacts morbidity and mortality considerably. A number do well in a developing country, but septic complications may be ongoing and recurrent. The high risk of neurodevelopmental and other problems continue beyond the neonatal period and patients should be “flagged” on for careful follow-up.

Similar content being viewed by others
References
Wilson R, Kanto WPJ, McCarthy BJ, Burton T, Lewin P, Terry J et al (1981) Epidemiologic characteristics of necrotizing enterocolitis: a population-based study. Am J Epidemiol 114:880–887
Stoll BJ (1994) Epidemiology of necrotizing enterocolitis. Clin Perinatol 21:205–218
Henry MC, Moss LR (2009) Necrotizing enterocolitis. Annu Rev Med 60:111–124
Kosloske AM, Musemeche CA, Ball WSJ, Ablin DS, Bhattacharyya N (1988) Necrotizing enterocolitis: value of radiographic findings to predict outcome. AJR 151:771–774
Grosfeld JL, Cheu H, Schlatter M, West KW, Rescorla FJ (1991) Changing trends in necrotizing enterocolitis: experience with 302 cases in two decades. Ann Surg 214:300–306
Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B et al (2004) Neurodevelopmental and growth impairment among extremely low birth-weight infants with neonatal infection. J Am Med Assoc 292:2357–2365
Rees CM, Pierro A, Eaton S (2007) Neurodevelopmental outcomes of neonates with medically and surgically treated necrotizing enterocolitis. Arch Dis Child Fetal Neonatal Ed 92:F193–F198
Chacko J, Ford WD, Haslam R (1999) Growth and neurodevelopmental outcome in extremely low-birth-weight infants after laparotomy. Pediatr Surg Int 15:496–499
Salhab WA, Perlman JM, Silver L, Broyles SR (2004) Necrotizing enterocolitis and neurodevelopmental outcome in extremely low birth weight infants <1000 g. J Perinatol 24:534–540
Sonntag J, Grimmer I, Scholz T, Metze B, Wit J, Obladen M (2000) Growth and neurodevelopmental outcome of very low birthweight infants with necrotizing enterocolitis. Acta Paediatr 89:528–532
Soraisham AS, Amin HJ, Al-Hindi MY, Singhal N, Sauve RS (2006) Does necrotising enterocolitis impact the neurodevelopmental and growth outcomes in preterm infants with birthweight ≤1250 g? J Paediatr Child Health 42:499–504
Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF et al (2005) Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics 115:696–703
Schulzke SM, Deshpande GC, Patole SK (2007) Neurodevelopmental outcomes of very low-birth-weight infants with necrotizing enterocolitis: a systematic review of observational studies. Arch Pediatr Adolesc Med 161:583–590
Tobiansky R, Lui K, Roberts S, Veddovi M (1995) Neurodevelopmental outcome in very low birthweight infants with necrotizing enterocolitis requiring surgery. J Paediatr Child Health 31(233):236
Walsh MC, Kliegman RM (1986) Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am 33:179–201
Adesanya OA, O’Shea TM, Turner CS, Amoroso RM, Morgan TM, Aschner JL (2005) Intestinal perforation in very low birth weight infants: growth and neurodevelopment at 1 year of age. J Perinatol 25:583–589
Wilson-Costello D (2007) Is there evidence that long-term outcomes have improved with intensive care? Semin Fetal Neonatal Med 12:344–354
Thompson CM, Buccimazza SS, Webster J, Malan AF, Molteno CD (1993) Infants of less than 1250 grams birth weight at Groote Schuur Hospital: outcome at 1 and 2 years of age. Pediatrics 91:961–968
Couper J (2002) Prevalence of childhood disability in rural KwaZulu-Natal. S Afr Med J 92:549–552
Christianson AL, Zwane ME, Manga P, Rosen E, Venter A, Downs D et al (2002) Children with intellectual disability in rural South Africa: prevalence and associated disability. J Intellect Disabil Res 46(2):179–186
High Risk Follow-Up Working Group (Kowloon Region) (2008) Neurodevelopmental outcomes of extreme-low-birth-weight infants born between 2001 and 2002. Hong Kong Med J 14:21–28
Vohr BR, Wright LL, Dusick AM, Perritt R, Poole WK, Tyson JE et al (2004) Center differences and outcomes of extremely low birth weight infants. Pediatrics 113:781–789
Adams-Chapman I, Stoll BJ (2006) Neonatal infection and long-term neurodevelopmental outcome in the preterm infant. Curr Opin Infect Dis 19:290–297
(1998) South Africa’s 1997 antenatal results give mixed messages. AIDS Anal Afr 8(3):3
Karpelowsky JS, Leva E, Kelley B, Numanoglu A, Rode H, Millar AJW (2009) Outcomes of human immunodeficiency virus-infected and -exposed children undergoing surgery: a prospective study. J Pediatr Surg 44(4):681–687
Chase C, Ware J, Hittelman J, Blasini I, Smith R, Llorente A et al (2000) Early cognitive and motor development among infants born to women infected with human immunodeficiency virus. Pediatrics 106:E25
Smith R, Malee K, Charurat M, Magder L, Mellins C, Macmillan C et al (2000) Timing of perinatal human immunodeficiency virus type 1 infection and rate of neurodevelopment. Pediatr Infect Dis J 19:862–871
Msellati P, Lepage P, Hitimana D-G, Van Goethem C, Van de Perre P, Dabis F (1993) Neurodevelopmental testing of children born to human immunodeficiency virus type 1 seropositive and seronegative mothers: a prospective cohort study in Kigali, Rwanda. Pediatrics 92:843–848
Pollack H, Kuchuk A, Cowan L, Hacimamutoglu S, Glasberg H, David R et al (1996) Neurodevelopment, growth, and viral load in HIV-infected infants. Brain Behav Immun 10:298–312
Brocklehurst P, French R (1998) The association between maternal HIV infection and perinatal outcome: a systemic review of the literature and meta-analysis. Br J Ostet Gynaecol 105:836–848
Blakely ML, Tyson JE, Lally KP, McDonald S, Stoll BJ, Stevenson DK et al (2006) Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: outcomes through 18 months adjusted age. Pediatrics 117:e680–e687
O’Connor A, Sawin RS (1998) High morbidity of enterostomy and its closure in premature infants with necrotizing enterocolitis. Arch Surg 133:875–880
Banieghbal B, Schoeman L, Kalk F, da Fonseca JM, Davies MR (2002) Surgical indications and strategies for necrotizing enterocolitis in low income countries. World J Surg 26:444–447
Henry MC, Moss RL (2008) Neonatal necrotizing enterocolitis. Semin Pediatr Surg 17(98):109
Olieman JF, Tibboel D, Penning C (2008) Growth and nutritional aspects of infantile short bowel syndrome for the past 2 decades. J Pediatr Surg 43:2061–2069
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arnold, M., Moore, S.W., Sidler, D. et al. Long-term outcome of surgically managed necrotizing enterocolitis in a developing country. Pediatr Surg Int 26, 355–360 (2010). https://doi.org/10.1007/s00383-010-2583-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-010-2583-8