Abstract
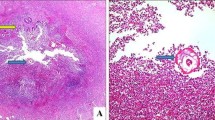
The association of Enterobius vermicularis infestation with acute appendicitis varies from 0.2–41.8% worldwide. Our purpose was to determine the significance of Enterobius-associated appendicitis by retrospective review of appendectomies performed during a 5-year period at a major children’s hospital. The Surgical Pathology database at Children’s Hospital, Columbus, Ohio, was reviewed for appendiceal specimens found to have Enterobius infestation. Corresponding patient charts were evaluated for age, gender, presenting symptoms, laboratory data, operative findings, and clinical course. Of the 1,549 appendectomies performed from January 1998 through January 2003, 21 specimens (1.4%) were found to contain Enterobius vermicularis. Fifteen of the appendectomies were performed for symptoms of acute appendicitis; the remaining six were incidental appendectomies in conjunction with other operations. The mean age was 8.9 years. Ten patients were male; 11 were female. Of the 15 symptomatic children, nine presented with fever >99.0ºF, and 11 had a WBC count >10,000. Intra-operative appearance of the appendix ranged from normal to perforation. Pathologic evaluation showed neutrophil or eosinophil infiltration in 15 of the 21 specimens. Enterobius infestation is an uncommon cause of acute appendicitis in children in the United States. It may be associated with acute appendicitis, “chronic appendicitis,” ruptured appendicitis, or with no significant clinical symptoms.
Similar content being viewed by others
References
Gatti S, Lopes R, Cevini C (2000) Intestinal parasitic infections in an institution for the mentally retarded. Ann Trop Med Parasitol 94:453–460
Henley M, Sears JR (1985) Pinworms: a persistent pediatric problem. MCN Am J Matern Child Nurs 10:111–113
Lee DS, Chung BH, Lee NS (1999) A survey of helminthic infections in the residents of rural areas near Ulaanbaatar, Mongolia. Korean J Parasitol 37:145–147
Liu LX, Weller PF (1994) Intestinal nematodes. In: Isselbacher KJ. Braunwald E (eds) Harrison’s principles of internal medicine, 13th edn. McGraw-Hill, New York, p 919
Yoon HJ, Choi YJ, Lee SU (2000) Enterobius vermicularis egg positive rate of pre-school children in Chunchon, Korea (1999). Korean J Parasitol 38:279–281
Ball MT, Hay J (1990) Simultaneous demonstration of eosinophilic granulocytes and mast cells in tissue sections containing helminths. Ann Trop Med Parasitol 84:195–196
Bredesen J, Lauritzen AF, Kristiansen VB, et al. (1988) Appendicitis and enterobiasis in children. Acta Chir Scand 154:585–587
Sterba J, Vlcek M (1984) Appendiceal enterobiasis—its incidence and relationships to appendicitis. Folia Parasitol (Praha) 31:311–318
Still GF (1899) Oxyuriasis vermicularis in children. Br Med J 1:898–900
Williams DJ, Dixon MF (1988) Sex, Enterobiasis vermicularis and the appendix. Br J Surg 75:1225–1226
Symmers W St C (1950) Pathology of oxyuris with special reference to granulomas due to presence of Oxyuris vermicularis and its ova in tissues. Arch Path 50:475
Fry FG, More JG (1969) Enterobius vermicularis: 10,000 year-old human infection. Science 166:1620
Sterba J, Vxcek M, Noll P, et al. (1985) Contribution to the question of relationships between Enterobius vermicularis (L.) and inflammatory processes in the appendix. Folia Parasitol (Praha) 32:231–235
Macedo T, MacCarty RL (2000) Eosinophilic ileocolitis secondary to Enterobius vermicularis: case report. Abdom Imaging 25:530–2
Sridhar R, Kapila K, Verma K (1999) Cytologic diagnosis of Enterobius vermicularis eggs in an enterocutaneous fistula. Indian J Pathol Microbiol 42:355–357
Ok UZ, Ertan P, Limoncu E, et al. (1999) Relationship between pinworm and urinary tract infections in young girls. APMIS107:474–476
Beeson BB, Woodruff AW (1971) Mesenteric abscess caused by threadworm infection. Trans R Soc Trop Med Hyg 65:433
Nutting SA, Murphy F, Inglis FG (1980) Abdominal pain due to Enterobius vermicularis. Can J Surg 23:286–287
Abramson DJ (1966) Acute appendicitis and a Meckel’s diverticulum with Enterobius vermicularis–first reported case. Am Surg 32:343–346
Dorfman S, Talbot IC, Torres R, et al. (1995) Parasitic infestation in acute appendicitis. Ann Trop Med Parasitol 89:99–101
Gross RE (1953) The surgery of infancy and childhood—its principles and techniques. Saunders, Philadelphia, pp 277–278
Morgenson K, Pahle E, Kowalski K(1985) Enterobius vermicularis and acute appendicitis. Acta Chir Scand 151:705–707
Saxena AK, Springer A, Tsokas J, et al. (2001) Laparoscopic appendectomy in children with Enterobius vermicularis. Surg Laparosc Endosc Percutan Tech 11:284–286
Tolstedt GE (1968) Pinworm infestation of the appendix. Am J Surg 116:454–455
Ajao OG, Malatani TS, ElDawi NE, et al. (1997) Enterobius vermicularis (pin worm) causing symptoms of appendicitis. Trop Doct 27:182–183
Batistatou A, Solota V, Scopa CD (2002) Images in pathology: Oxyuris (Enterobius) vermicularis in human cecum and appendix. Int J Surg Pathol 10:58
Boulos PB, Cowie GA (1973) Pinworm infestation of the appendix. Br J Surg 60:975–6
Budd JS, Armstrong C (1987) Role of Enterobius vermicularis in the aetiology of appendicitis. Br J Surg 74:748–749
Cerva L, Schrotenbaum M, Kliment V (1991) Intestinal parasites: a study of human appendices. Folia Parasitol (Praha) 38:5–9
Dahlstrom JE, Macarthur EB (1994) Enterobius vermicularis: a possible cause of symptoms resembling appendicitis. Aust N Z J Surg 64:692–694
Dalimi A, Khoshzaban F (1993) Comparative study of two methods for the diagnosis of Enterobius vermicularis in the appendix. J Helminthol 67:85–86
Duran-Jorda F (1957) Appendicitis and enterobiasis in children—a histological study of 691 appendices. Arch Dis Child 13:208–217
Gupta SC, Gupta AK, Keswani NK (1989) Pathology of tropical appendicitis. J Clin Pathol 42:1169–1172
Sinnah B, Leopairut J, Neafie RC, et al. (1991) Enterobiasis: a histopathological study of 259 patients. Ann Trop Med Parasitol 85:625–635
Wiebe BM (1991) Appendicitis and Enterobius vermicularis. Scand J Gastroenterol 26:336–338
Zoorob RJ (1996) Appendiceal colic caused by Enterobius vermicularis. J Am Board Fam Pract 9:57–59
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Arca, M.J., Gates, R.L., Groner, J.I. et al. Clinical manifestations of appendiceal pinworms in children: an institutional experience and a review of the literature. Ped Surgery Int 20, 372–375 (2004). https://doi.org/10.1007/s00383-004-1151-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-004-1151-5