Abstract
Objectives
To assess the feasibility, safety and preliminary efficacy of magnetic resonance-guided focused ultrasound (MRgFUS) for the treatment of extra-abdominal desmoid tumours.
Methods
Fifteen patients with desmoid fibromatosis (six males, nine females; age range, 7–66 years) were treated with MRgFUS, with seven patients requiring multiple treatments (25 total treatments). Changes in viable and total tumour volumes were measured after treatment. Efficacy was evaluated using an exact one-sided Wilcoxon test to determine if the median reduction in viable tumour measured immediately after initial treatment exceeded a threshold of 50 % of the targeted volume. Median decrease after treatment of at least two points in numerical rating scale (NRS) worst and average pain scores was tested with an exact one-sided Wilcoxon test. Adverse events were recorded.
Results
After initial MRgFUS treatment, median viable targeted tumour volume decreased 63 %, significantly beyond our efficacy threshold (P = 0.0013). Median viable total tumour volume decreased (105 mL [interquartile range {IQR}, 217 mL] to 54 mL [IQR, 92 mL]) and pain improved (worst scores, 7.5 ± 1.9 vs 2.7 ± 2.6, P = 0.027; average scores, 6 ± 2.3 vs 1.3 ± 2, P = 0.021). Skin burn was the most common complication.
Conclusions
MRgFUS significantly and durably reduced viable tumour volume and pain in this series of 15 patients with extra-abdominal desmoid fibromatosis.
Key Points
• Retrospective four-centre study shows MRgFUS safely and effectively treats extra-abdominal desmoid tumours
• This non-invasive procedure can eradicate viable tumour in some cases
• Alternatively, MRgFUS can provide durable control of tumour growth through repeated treatments
• Compared to surgery or radiation, MRgFUS has relatively mild side effects


Similar content being viewed by others
References
Kasper B, Strobel P, Hohenberger P (2011) Desmoid tumors: clinical features and treatment options for advanced disease. Oncologist 16:682–93
Bonvalot S, Desai A, Coppola S et al (2012) The treatment of desmoid tumors: a stepwise clinical approach. Ann Oncol 23:x158–66
Walczak BE, Rose PS (2013) Desmoid: the role of local therapy in an era of systemic options. Curr Treat Options Oncol 14:465–73
Salas S, Dufresne A, Bui B et al (2011) Prognostic factors influencing progression-free survival determined from a series of sporadic desmoid tumors: a wait-and-see policy according to tumor presentation. J Clin Oncol 29:3553–8
Melis M, Zager JS, Sondak VK (2008) Multimodality management of desmoid tumors: how important is a negative surgical margin? J Surg Oncol 98:594–602
Kujak JL, Liu PT, Johnson GB, Callstrom MR (2009) Early experience with percutaneous cryoablation of extra-abdominal desmoid tumors. Skelet Radiol 39:175–82
Wang Y, Wang W, Tang J (2011) Ultrasound-guided high intensity focused ultrasound treatment for extra-abdominal desmoid tumours: preliminary results. Int J Hyperth 27:648–53
Mullen JT, DeLaney TF, Kobayashi WK et al (2012) Desmoid tumor: analysis of prognostic factors and outcomes in a surgical series. Ann Surg Oncol 19:4028–35
Peng PD, Hyder O, Mavros MN et al (2012) Management and recurrence patterns of desmoids tumors: a multi-institutional analysis of 211 patients. Ann Surg Oncol 19:4036–42
Gronchi A, Colombo C, Le Pechoux C et al (2014) Sporadic desmoid-type fibromatosis: a stepwise approach to a non-metastasising neoplasm—a position paper from the Italian and the French Sarcoma Group. Ann Oncol 25:578–83
Rutenberg MS, Indelicato DJ, Knapik JA et al (2011) External-beam radiotherapy for pediatric and young adult desmoid tumors. Pediatr Blood Cancer 57:435–42
Guadagnolo BA, Zagars GK, Ballo MT (2008) Long-term outcomes for desmoid tumors treated with radiation therapy. Int J Radiat Oncol Biol Phys 71:441–7
Mindjuk I, Trumm CG, Herzog P, Stahl R, Matzko M (2014) MRI predictors of clinical success in MR-guided focused ultrasound (MRgFUS) treatments of uterine fibroids: results from a single center. Eur Radiol 25:1317–28
Hurwitz MD, Ghanouni P, Kanaev SV et al (2014) Magnetic resonance-guided focused ultrasound for patients with painful bone metastases: phase III trial results. J Natl Cancer Inst 106 doi:10.1093/jnci/dju082
Schmitz AC, Gianfelice D, Daniel BL, Mali WPTM, van den Bosch MAAJ (2008) Image-guided focused ultrasound ablation of breast cancer: current status, challenges, and future directions. Eur Radiol 18:1431–41
Napoli A, Anzidei M, De Nunzio C et al (2013) Real-time magnetic resonance–guided high-intensity focused ultrasound focal therapy for localised prostate cancer: preliminary experience. Eur Urol 63:395–8
Hynynen K (2010) MRI-guided focused ultrasound treatments. Ultrasonics 50:221–9
National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) v4.0. NCI, NIH, DHHS. 2009; NIH publication # 09–7473. URL: http://evs.nci.nih.gov/ftp1/CTCAE/About.html. Accessed 15 Nov 2015
Clark SK, Smith TG, Katz DE, Reznek RH, Phillips RK (1998) Identification and progression of a desmoid precursor lesion in patients with familial adenomatous polyposis. Br J Surg 85:970–3
Nuyttens JJ, Rust PF, Thomas CR, Turrisi AT (2000) Surgery versus radiation therapy for patients with aggressive fibromatosis or desmoid tumors: a comparative review of 22 articles. Cancer 88:1517–23
Shapeero LG, De Visschere PJL, Verstraete KL et al (2009) Post-treatment complications of soft tissue tumours. Eur J Radiol 69:209–21
Dineen SP, Roland CL, Feig R et al (2015) Radiation-associated undifferentiated pleomorphic sarcoma is associated with worse clinical outcomes than sporadic lesions. Ann Surg Oncol 22:3913–20
Avedian RS, Bitton R, Gold G, Butts Pauly K, Ghanouni P (2016) Is MR-guided high-intensity focused ultrasound a feasible treatment modality for desmoid tumors? Clin Orthop Relat Res 474:697–704
Acknowledgments
The authors are grateful to Dr. Sheri Spunt for her comments on the manuscript.
The scientific guarantor of this publication is Pejman Ghanouni. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. This study has received funding by NIH P01 CA159992. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Some study subjects have been previously reported in Avedian et al. [23].
Methodology: retrospective, observational, multicentre study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For retrospective studies, formal consent is not required.
Additional information
Alberto Bazzocchi and Matthew Bucknor contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
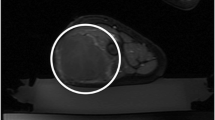
Fig. 1-S
Positioning for MRgFUS ablation of desmoid tumour in the posterior ankle of a 66-year-old man, with additional post-treatment images. This is the same tumour shown in Fig. 1 (patient no. 4). In a, an axial T1-weighted 3D SPGR fat-suppressed image of the ankle used for treatment planning is presented. The white arrow points to the tumour, located between the Achilles tendon (+), and the flexor hallucis longus tendon (*), talus (T) and fibula (F). The patient was in a left lateral decubitus position, with the medial aspect of the ankle located closer to the ultrasound transducer (Tr). Moistened gel pads (GP) are positioned around the ankle, in the near field to allow acoustic coupling to the transducer, and in the far field superficial to the lateral ankle to avoid an air-skin interface, which could otherwise lead to a skin burn. In b, a coronal post-contrast T1-weighted 2D SPGR fat-saturated image obtained 2 weeks before initial treatment shows an enhancing mass in the posterior ankle (white arrow), above the calcaneus (Cal). Sonications were directed from the medial side (M), even though the tumour is closer here to the skin, because the sural nerve traverses the region lateral (L) to the tumour. In c, a coronal post-contrast image obtained 14 months after initial treatment and 5 months after a second treatment, the tumour (white arrow) is predominantly necrotic. Enhancement consistent with residual tumour is present laterally (red asterisk). A curvilinear enhancing line in the medial aspect of the calcaneus represents inflammation related to osteonecrosis from thermal ablation (yellow arrow). In d, a coronal post-contrast image obtained 20 months after initial treatment, the tumour (white arrow) has declined in volume and remains predominantly necrotic. Residual enhancement (red asterisk) is present laterally, but the overall volume of enhancing tumour was unchanged from the prior MR imaging (TIF 7006 kb)
Fig. 2-S
MRgFUS treatment of an enlarging, painful desmoid tumour in the right calf in a 15-year-old girl (patient no. 9). She and her family refused surgery and radiation. MRgFUS was used to debulk the portion of the tumour in the superior medial calf, avoiding tumour near the Achilles tendon, and then the remaining tumour was treated with chemotherapy. In a, an axial post-contrast T1-weighted fat-saturated image shows an enhancing infiltrative mass involving the medial gastrocnemius and soleus muscles (white arrow). In b, an axial post-contrast T1-weighted 3D SPGR fat-suppressed image obtained immediately after treatment shows that the majority of the tumour has been ablated (white arrow). Out of 135 mL of tumour volume targeted, 110 mL were non-perfused after treatment (81 %). This represented ablation of 56 % of the total tumour volume (110 of 195 mL). In c, an axial post-contrast T1-weighted fat-saturated image obtained 3 months after MRgFUS ablation and before initiation of chemotherapy shows necrotic tumour with surrounding peripheral enhancement (white arrow), which may represent residual tumour. In d, an axial post-contrast T1-weighted fat-saturated image obtained 7 months after MRgFUS ablation and 4 months after initiation of chemotherapy shows decrease in size of the tumour, and decrease in surrounding peripheral enhancement (white arrow), indicating response to treatment. Total tumour volume decreased at that point from 195 to 156 mL (20 % decline), and viable tumour volume decreased to 118 mL (39 % decline). The patient’s severe pain also improved after MRgFUS treatment (NRS: pre, 9; post, 4) (TIF 11487 kb)
Fig. 3-S
MRgFUS treatment of a 14-year-old boy with recurrent, painful desmoid tumour in the right buttock, posterior to the hip joint (patient no. 1). Three years earlier, the patient underwent primary resection of a desmoid tumour in the right popliteal fossa, with recurrence, ultimately leading to above-the-knee amputation. Despite this, there was recurrence in the thigh and buttock, which did not respond to chemotherapy. Tumour in the buttock was targeted for initial MRgFUS treatment, as the tumour was reaching the pelvis, with surgical alternative of hemipelvectomy. In a, an axial post-contrast T1-weighted fat-suppressed image obtained prior to treatment shows bulky tumour (white arrow) posterior to the ischium. In b, an axial post-contrast T1-weighted fat-suppressed image obtained immediately after MRgFUS treatment shows the non-perfused volume of the ablated tumour (white arrow); 74 % (73 of 98 mL) of the tumour was ablated. A small rim of residual enhancement is present laterally; this area was not targeted because of concern for potential damage to cartilage in the hip joint, which was in the far field. In addition, there is a hypoperfused area in the gluteus maximus muscle (between red arrows) that resulted from near-field heating in the muscle. Periosteal hyperemia from far-field heating is also present in the posterior ischium (yellow arrow). In c, an axial post-contrast T1-weighted fat-suppressed image obtained 1 year after treatment shows recurrent tumour (white arrow) posterior to the ischium. The hypoperfused area in the gluteal muscle is smaller (red asterisk), compatible with healing. In d, an axial post-contrast T1-weighted fat suppressed image shows ablation of the recurrent tumour (white arrow). In e, an axial post-contrast T1-weighted fat-suppressed image obtained 23 months after initial treatment, by which time he had received four total treatments to the tumour in his buttock and thigh, shows no solid enhancing component to indicate residual tumour in the buttock at this time (white arrow). Overall, the enhancing volume declined from 98 to 4 cc (96 % decline). The patient’s moderate pain also improved (NRS: pre, 6; post, 0) (TIF 14360 kb)
Fig. 4-S
MRgFUS treatment of an enlarging, painful desmoid tumour in the hypothenar region of the right hand in a 14-year-old boy (patient no. 10). Surgery was not recommended by his orthopaedic surgeon, and the patient and his family opted for MRgFUS treatment rather than radiation or chemotherapy. In a, an axial post-contrast T1-weighted fat-saturated image demonstrates an enhancing mass (white arrow) that is exophytic and also infiltrates the central palm around the ulnar nerve and vessels to reach the flexor retinaculum. In b, an axial post-contrast T1-weighted fat-suppressed image of the tumour (white arrow) obtained immediately after treatment shows ablation of 58 % of the desmoid (2.3 out of 4 mL). In c, an axial post-contrast T1-weighted fat-saturated image obtained 4 months after treatment demonstrates decreased volume of the tumour to 0.9 mL (78 % decline). The patient’s mild pretreatment pain also improved (NRS: pre, 2; post, 0) (TIF 26507 kb)
Rights and permissions
About this article
Cite this article
Ghanouni, P., Dobrotwir, A., Bazzocchi, A. et al. Magnetic resonance-guided focused ultrasound treatment of extra-abdominal desmoid tumors: a retrospective multicenter study. Eur Radiol 27, 732–740 (2017). https://doi.org/10.1007/s00330-016-4376-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4376-5