Abstract
Physical activity (PA) is increasingly recognised as an important factor within studies of osteoarthritis (OA). However, subjective methods used to assess PA are highly variable and have not been developed for use within studies of OA, which creates difficulties when comparing and interpreting PA data in OA research. The aim of this study was, therefore, to gain expert agreement on the appropriate methods to harmonise PA data among existing population cohorts to enable the investigation of the association of PA and OA. The definition of PA in an OA context and methods of harmonization were established via an international expert consensus meeting and modified Delphi exercise using a geographically diverse committee selected on the basis of individual expertise in physical activity, exercise medicine, and OA. Agreement was met for all aims of study: (1) The use of Metabolic Equivalent of Task (MET) minutes per week (MET-min/week) as a method for harmonising PA variables among cohorts; (2) The determination of methods for treating missing components of MET-min/week calculation; a value will be produced from comparable activities within a representative cohort; (3) Exclusion of the domain of occupation from total MET-min/week; (4) The need for a specific measure of joint loading of an activity in addition to intensity and time, in studies of diseases, such as OA. This study has developed a systematic method to classify and harmonise PA in existing OA cohorts. It also provides minimum requirements for future studies intending to include subjective PA measures.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is a chronic condition of the synovial joint, which includes the progressive degeneration of cartilage and the excess growth of bone, often leading to pain and functional impairment [1]. It is one of the leading causes of global disability, with adult prevalence rates reported between 8.5–22% for symptomatic radiographic knee OA [2–4] and 3.4–8.9% for symptomatic radiographic hip OA [3, 5, 6]. To determine risk factors for this disease, it is necessary to analyse previously collected data from longitudinal population cohorts. While there are some well-established risk factors for hip and knee OA, the relationship between physical activity (PA) and OA is inconsistent. This, in part, may be due to the heterogeneous definition of PA used in cohorts and the lack of differentiation between weight-bearing and non-weight-bearing activity.
PA is defined as any bodily movement that results in energy expenditure and is categorised by domains, including occupation, leisure time, daily living, and active travel. Assessment of PA in cohort studies of OA is usually captured by self-report questionnaires, typically including measures of frequency, intensity, duration, and type [7]. Much of the previous research on PA has been completed within the area of cardiovascular disease and obesity and many of the questionnaires and assessments were developed with such health outcomes in mind. Although observational OA-related cohorts have collected information on PA, the parameters measured differ between studies and the number of domains varies, making comparison and interpretation of results difficult. Equally as important is the lack of an available method to assess the degree of joint loading for different physical activities, which is a known risk factor for OA.
A recent systematic review of observational studies, subject to the above limitations, confirmed the association of injury, obesity, and occupational activity with knee and hip OA; however, increased volume and intensity of PA were found to be a risk factor for OA in four studies and protective in another [8]. Due to the heterogeneity in the definition of PA, meta-analysis was not possible for the risk of PA on OA.
To address the difficulties in comparing heterogeneous aggregate data within epidemiological research, an increasingly popular alternative to meta-analysis is individual participant data (IPD) meta-analysis, where the raw individual level data are used for statistical synthesis [9]. This method allows for using the combined power of multiple international cohort studies to address more complex research questions, such as the association between PA and OA [10–18]. A key element of IPD meta-analysis is the harmonization of the variables, which requires a standard measure of both PA and OA from all the included cohorts. Unfortunately, population-based cohort studies have collected PA data using a variety of validated questionnaires and individual questions, which need to be harmonised to be included in any analysis.
To enable this, a number of issues need to be addressed: PA questionnaires and questions vary between cohorts; not all domains are available in all cohorts; some activities are attributes to varying domains (e.g., walking and cycling is included with sport and recreation in a number of cohorts, yet travel in others); duration, intensity, and frequency of PA are not addressed consistently between cohorts; and PA has not previously been assessed by degree of weight-bearing for use in studies of lower limb OA.
A consensus study, including an expert meeting and Delphi approach, was developed to address these issues. The aims of this study were to:
-
1.
Determine the usability of a common metric (Metabolic equivalent of task [MET]) as a key method for harmonising PA assessments/questions between cohorts, and agree upon specific assumptions required to generate METs for each cohort (objectives 1 and 2).
-
2.
Assess the available domains of PA and establish the appropriate assumptions needed to harmonise information between cohorts (objectives 3 and 4).
-
3.
Evaluate the potential to use of a lower limb OA-specific PA measure within the cohorts, taking weight-bearing into consideration (objective 5).
-
4.
Evaluate the use of national PA guidelines to determine the effect of meeting such recommendations on the association with lower limb OA (objective 6).
Methods
The process consisted of the following steps
PA expert committee
A multidisciplinary, geographically diverse expert committee was selected on the basis of individual expertise in PA; exercise medicine and OA and each were invited to participate in developing a PA variable for use in normal population-based cohort studies. The expert committee (n = 9 of the listed co-authors) met by video conference link in December 2014.
Expert consensus meeting
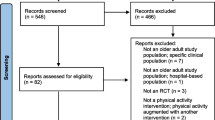
The steering group (consisting of authors LG, KL, and NA) conducted a systematic evaluation of international cohorts containing PA and OA data. Four key issues were identified by the steering group whilst establishing the methods to harmonise PA data between cohorts which had not been adequately addressed in the previous literature. Background topic information, the previous research where applicable and specific factors relating to individual cohorts were provided to experts before the meeting to assist informed decision-making. Each issue was presented and facilitated discussion undertaken until agreement was reached.
Delphi
If a question was raised within the expert meeting and no agreement could be made, due to either a requirement for further investigation or exploration of cohort data, then these items were addressed within a follow-up Delphi technique to obtain consensus. The Delphi technique, which is a structured process of anonymous iteration [19], consisted of an online questionnaire, which was sent to each expert, following the meeting. In accordance with the previous OARSI Delphi exercises to define OA diagnostic criteria [20], inclusion for measures within each round was based on having ≥60% of the votes. Evidenced-based information was provided to inform each item, and where applicable more in depth data from individual cohorts were provided. Unanimous decision-making was made within the first round.
The aims of the consensus study were addressed via six methodological objectives:
-
1.
Determine the suitability of using METs as a key method for harmonising PA exposure variables between cohorts.
-
2.
Determine methods for treating missing components of MET-min/week calculation.
-
3.
Assess the domains of physical activity: how to treat missing domains.
-
4.
Assess the domains of physical activity: the use of occupation as a PA domain in studies with OA as an outcome.
-
5.
Evaluate the use of an OA-specific PA measure taking weight-bearing vs. non-weight-bearing activity into consideration.
-
6.
Establish if thresholds based on national PA guidelines should be used to investigate the association of PA with OA.
Results
Determine the suitability of using METs as a key method for harmonising PA exposure variables between cohorts
Background information provided to experts
The steering group proposed using the MET to harmonise PA data across population cohorts, based on the results of the literature search and availability of measures within cohorts. PA data can be converted to MET-min/week using the 2011 Compendium of Physical Activities [21] if METs were not already reported. MET is a physiological measure which expresses the intensity and energy expenditure of an activity, and is defined as the ratio of the rate of energy expended during an activity to the rate of energy expended at rest (e.g., 1 MET is the rate of energy expenditure while at rest) [22]. Standard intensity thresholds have been established for MET values of activities with <3 as light, 3–5.9 as moderate, and ≥6 as vigorous [23]. MET-min/week is calculated by multiplying the MET value of an activity (from a standard Compendium of Physical Activities values [21] by the number of minutes per week an activity is done [24]). METs have been used for recommending activity in adults for chronic disease prevention and health promotion [23].
Points for expert discussion
Due to the variability between cohorts in the way PA exposure was reported and the wording of PA questions, the benefits, limitations, and feasibility of converting the questions from each cohort into MET-min/week as the standard unit were proposed as the first discussion point to be addressed within the expert consensus meeting.
Determine methods for treating missing components of MET-min/week calculation
Background information provided to experts
To convert PA exposure data to MET-min/week, the duration, frequency, and intensity of an activity are required. In certain cohorts within the current study, some of these parameters were not collected, and a number of assumptions needed to be made. The previous studies have adopted a standard bout time of 30 min when duration was missing from the physical activity question, but the validity of this assumption is unclear [25].
Points for expert discussion
Several common PA questionnaires do not include intensity, frequency, or duration of the activity, preventing a direct calculation of MET-min/week. A possible solution proposed by the steering group was to use a standard intensity MET value when calculating MET-min/week if the terminology included “low”, “moderate”, or “high”, and to use a standard of 30 min when duration was missing. These issues raised a requirement for additional investigation via a further Delphi study.
Further investigation recommended
For the Delphi exercise, median duration data for individual activities were prepared by the steering group from the cohorts where these data were available (Supplementary Appendix 1). These data were to be presented for agreement within the Delphi to ascertain agreement on the generalisability of the median durations for each activity. Due to some variation between standard activity times between countries, a proposal was made to use the median durations from the Hertfordshire Cohort Study ; a UK study of 3000 men and women born during the period 1931–1939 [15], for other UK cohorts with missing duration data, and similarly to use the durations from Johnston County Osteoarthritis Study: a US community-based, longitudinal study of approximately 3200 rural Caucasian and African American residents aged 45 and older [11], for US cohorts with missing data. The same method was proposed where frequency was identified as missing in one UK cohort (Supplementary Appendix 2).
Assess the domains of physical activity: how to treat missing domains
Background information provided to experts
In previous research, household activities have been included as an essential domain of PA to determine the minimum amount of PA associated with significantly lower risks of all-cause mortality [26, 27]. Household activities have also been specifically included within PA health guidelines [28]. The importance of household activities is also anticipated in determining the association of PA with lower limb OA, particularly due to the known risks of increased cumulative loads seen in such activities and knee OA [29]. Household activities are largely modifiable and are, therefore, an important consideration for any public health message involving physical activity.
Points for expert discussion
A significant number of the population-based cohorts did not ask questions regarding household activities and/or gardening, both of which have been identified as important contributors to daily activity loads. Experts were asked to consider the impact of excluding these domains from the primary physical activity variable, and if there were alternative actions to consider.
Assess the domains of physical activity: the use of occupation as a PA domain in studies with OA as an outcome
Background information provided to experts
Occupation, in particular manual labour occupations, is a well-established risk factor for OA [30, 31], and is, therefore, an important consideration in an analysis using OA as the primary outcome. The occupation section within the Compendium of Physical Activities [21] was designed for counting different tasks within one occupation over 1 day and is of limited use for providing an “average” MET value for a specific occupation (i.e., MET values of individual tasks which make up a complete occupation are given and are expected to be done for an entire hour). Occupation is the least modifiable domain of PA and approximately 50% of the consortium cohorts had no or limited occupation data available. It would, therefore, be difficult to calculate a valid exposure in MET-min/week from the available data. The potential for occupation activities to be overestimated is greater than for any other domain, particularly because the occupation MET value within the Compendium of Physical Activities assumes that a specific MET activity is completed for entire hour. To multiply this by hours, worked in 1 week would potentially overestimate weekly METs. The majority of consortium cohorts, which did have occupation data available, did not define tasks within occupation in anything less than 1 day.
Points for expert discussion
Experts were asked to discuss the limitations of excluding occupation from the overall physical activity variable specific to studies using osteoarthritis as an outcome. The preferred treatment of an osteoarthritis variable (e.g., MET-min/week and categories) was also explored.
Further investigation recommended
A method was required for categorisation into levels, defining occupations into manual and non-manual tasks. Due to the variety of occupation-related tasks available in each cohort, the occupation level reported in the Physical Activity Scale for the Elderly (PASE) questionnaire was used to facilitate the categorisation of occupation-related tasks. The PASE questionnaire is designed to assess the duration, frequency, exertion level, and amount of physical activity undertaken over a 7 day period [32]. The steering group matched the PASE occupation levels to the corresponding four levels of occupation, which were suggested in the expert consensus meeting. The selection of occupation-related tasks with each of the four levels of occupation (sedentary, light, light manual and heavy manual) was prepared to be presented within the follow-up Delphi exercise (Supplementary Appendix 3).
Evaluate the use of an OA-specific PA measure taking weight-bearing vs. non-weight-bearing activity into consideration
Background information provided to experts
OA is at least in part a mechanically driven disease [33]. The association between PA and risk of OA may, therefore, be dependent on joint loading and type of PA [34].
Points for expert discussion
There was a need to identify a method that could account for the weight-bearing component of PA. The fifth proposed discussion point for the meeting was, therefore, the potential to use previously established bone and joint loading questionnaires to quantify loading [35, 36].
Further investigation recommended
Informed by these decisions, each activity listed within the study cohorts was placed into corresponding loading categories of low, moderate, and high joint loading based on the degree of impact and loading (Supplementary Appendix 4). These were prepared by the steering group for presentation within a follow-up Delphi exercise.
Establish if thresholds based on national PA guidelines should be used to investigate the association of PA with OA
Background information provided to experts
It is important to ensure that a translatable public health message is provided; however, the relationship of meeting or not meeting PA guidelines and the risk of OA are unknown. The use of a threshold based on national guidelines such as those from the American College of Sports Medicine and the American Heart Association [37], the US Physical Activity Guidelines Advisory Committee (US PAGAC) report [23], and the U.K. Department of Health [38] (150 min/week of moderate-equivalent activity) was, therefore, proposed to investigate the effect of meeting current guidelines on the risk of OA.
An additional threshold was suggested to investigate the risk of inactivity on risk of OA; however, there is no global consensus on a defined threshold for inactivity. According to the US PAGAC report [23], <10 min/week of moderate activity is defined as ‘inactive’ and this is in comparison to the UK definition of ‘inactivity’ of <30 min/week moderate activity.
There is growing evidence that increasing steps per day provides health benefits [39–42]. Although originally based on minimal evidence, the 10,000 steps a day guideline now provides a translatable and applicable PA recommendation [43].
Points for expert discussion
The final points proposed for discussion within the expert meeting were the use of current national guidelines as a threshold for PA in the investigation of the PA and OA. Also discussed was the use of either a previous arbitrary threshold for inactivity or a new data driven threshold, and the use of steps per day as an equivalent for the translatable outcome instead of 150 min of weekly moderate-equivalent activity.
Expert consensus meeting results
Within the expert meeting, each aim was discussed until consensus reached. Where new questions were raised, these were addressed within a follow-up Delphi exercise. There was unanimous agreement for every objective within the consensus meeting and follow-up Delphi. In summary, key agreements were made based upon: the use of MET-min/week as a method for harmonising PA variables between cohorts; defining methods for treating missing components of MET-min/week calculation, in particular the use of a value produced from comparable activities within a representative cohort; the exclusion of the domain of ‘occupation’ from total MET-min/week; and the need for a specific measure of ‘joint loading’ of an activity in studies of bone diseases, such as osteoarthritis.
Details of the decisions made within the consensus meeting and follow-up Delphi are shown in Tables 1 and 2.
Discussion
Our research describes a method to classify and harmonise PA data for epidemiology research in population-based OA-related cohorts, based on international consensus. The recommendations will allow the IPD meta-analysis of PA and incident lower limb OA to be undertaken using the most comprehensive PA data possible. In addition, it will be useful not only for future epidemiology research into OA that uses physical activity and IPD studies, but also to guide researchers planning to collect PA data for current or future epidemiological research.
Recommendations for combining data between cohorts, based on expert opinion in this study, are to use MET-min/week as a standardised measure of PA. In the instance of a missing parameter, such as duration, frequency, or intensity, the methods of assigning values using data derived from representative cohorts or the Compendium of Physical Activities have been agreed. The likely effects of occupation should be accounted for by categorisation of occupation type and stratification. The weight-bearing aspect within PA should be taken into consideration when using OA as an outcome.
Although national PA guidelines are an essential and translatable source of health prescription, they were not designed with OA in mind. Guidelines are required to address health and, therefore, recommendations relative to OA, an increasing global burden, are required to add to other disease areas. There are a number of domains of PA to consider when assessing the target for meeting national recommendations; these include leisure time, household/gardening, active travel, and occupational activities. These domains are particularly pertinent when considering the effect of PA on lower limb OA due to the weight-bearing nature of many activities within each and the difficulty is that there is currently no index to combine the physiological measure of METs and joint load.
An increasingly popular alternative to meeting 150 min/week of moderate-equivalent activity is the daily accumulation of 10,000 steps. Experts agreed that this could be a useful method of assessing PA against OA in the future. Recommendations from the expert consensus study suggest that a guideline based on the personalised optimum number of steps per day to reduce the risk of OA would be a valuable public health message.
A limitation of this study was that decisions had to be based on already data that were already available, because due to the requirement to use existing population-based cohorts to investigate the association between PA and OA. There are also known limitations for using METs as a measure of PA, particularly when making comparisons among a number of studies or populations. Studies have previously measured METs based on a varying numbers of activities from the total available from the domains of PA [44]. As a MET is the total volume of a given activity, which combines frequency, intensity, and duration, the effect of duration or intensity alone cannot be deciphered. IPD meta-analysis allows for the use of original raw data, so that all aspects of PA can be included and where no available in certain circumstances imputation methods can be applied. Likewise, the access to original data allows for data driven thresholds to derived and provides potential for observing individual parameters of PA, be it intensity or duration.
A further limitation to this study was the use of PA data from more than one decade ago to calculate median duration for those cohorts missing this data. Although PA levels are likely to have changed, since these data were collected the committee felt, this was still a more appropriate representation of duration than using a standard 30 min, which is likely to over or underestimate activity levels.
Our study provides the first expert consensus on the limitations of and the methods for harmonising PA data in population-based OA cohort studies. The application of these recommendations in future individual patient meta-analysis on PA and OA will provide a homogeneous way to assess PA in cohorts from around the world. It will also allow for quantifying the volume of PA and examine the shape of the dose–response curve for PA and OA as well as the ability to apply new thresholds for future national PA guidelines. These findings will also be useful for any study investigating PA and other long-term health outcomes in existing cohort data. The recommendations arising from this consensus study for the collection of PA data in normal population-based cohort studies are: the need for all parameters of a given activity (duration, frequency, and type/intensity) within a specified timeframe; PA measured in all domains of daily life (sport/leisure, household/gardening, active travel, and occupation); an occupation measure which can be used to calculate accurate MET-min/week value in addition to a manual labour (occupational tasks) in terms of OA risk; and a measure of joint loading for each reported activity.
References
Brandt KD, Radin EL, Dieppe PA, van de Putte L (2006) Yet more evidence that osteoarthritis is not a cartilage disease. Ann Rheum Dis 65(10):1261–1264
Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J et al (2007) Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol 34(1):172–180
Pereira D, Peleteiro B, Araújo J, Branco J, Santos RA, Ramos E (2011) The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthr Cartil 19(11):1270–1285
Turkiewicz A, Gerhardsson de Verdier M, Engström G, Nilsson PM, Mellström C, Lohmander LS et al (2015) Prevalence of knee pain and knee OA in southern Sweden and the proportion that seeks medical care. Rheumatology 54(5):827–835
Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J et al (2009) Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and caucasians: the Johnston county osteoarthritis project. J Rheumatol 36(4):809–815
Kim C, Linsenmeyer KD, Vlad SC, Guermazi A, Clancy MM, Niu J et al (2014) Prevalence of radiographic and symptomatic hip osteoarthritis in an urban united states community: the framingham osteoarthritis study. Arthritis Rheumatol 66(11):3013–3017
Bauman A, Phongsavan P, Schoeppe S, Owen N (2006) Physical activity measurement—a primer for health promotion. Promot Educ 13(2):92–103
Richmond SA, Fukuchi RK, Ezzat A, Schneider K, Schneider G, Emery CA (2013) Are joint injury, sport activity, physical activity, obesity, or occupational activities predictors for osteoarthritis? A systematic review. J Orthopaed Sports Phys Ther 43(8):515–519
Riley RD, Lambert PC, Abo-Zaid G (2010) Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ 340:c221
Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP (1975) The Framingham Offspring Study. Design and preliminary data. Prevent Med (Baltimore) 4:518–525
Jordan JM, Linder GF, Renner JB, Fryer JG (1995) The impact of arthritis in rural populations. Arthritis Care Res 8(4):242–250
Cummings SR, Black DM, Nevitt MC et al (1990) APpendicular bone density and age predict hip fracture in women. JAMA 263(5):665–668
Felson DT, Nevitt MC (2004) Epidemiologic studies for osteoarthritis: new versus conventional study design approaches. Rheum Dis Clin N Am 30(4):783–797
Hart DJ, Mootoosamy I, Doyle DV, Spector TD (1994) The relationship between osteoarthritis and osteoporosis in the general population: the Chingford Study. Ann Rheum Dis 53(3):158–162
Syddall H, Aihie Sayer A, Dennison E, Martin H, Barker D, Cooper C et al (2005) Cohort profile: the Hertfordshire cohort study. Int J Epidemiol 34(6):1234–1242
Hofman A, Murad SD, Duijn CM, Franco OH, Goedegebure A, Arfan Ikram M et al (2013) The Rotterdam study: 2014 objectives and design update. Eur J Epidemiol 28(11):889–926
Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T (2010) Cohort profile: research on osteoarthritis/osteoporosis against disability study. Int J Epidemiol 39(4):988–995
Ding C, Parameswaran V, Cicuttini F, Burgess J, Zhai G, Quinn S et al (2008) Association between leptin, body composition, sex and knee cartilage morphology in older adults: the Tasmanian older adult cohort (TASOAC) study. Ann Rheum Dis 67(9):1256–1261
Stewart J (2001) Is the Delphi technique a qualitative method? Med Educ 35(10):922–923
Hunter DJ, Arden N, Conaghan PG, Eckstein F, Gold G, Grainger A et al (2011) Definition of osteoarthritis on MRI: results of a Delphi exercise. Osteoarthr Cartil 19(8):963–969
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C et al (2011) Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 43(8):1575–1581
Ainsworth B, Haskell W, Leon A, Jacobs D, Montoye H, Sallis J et al (1993) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25(1):71–80
Physical Activity Guidelines Advisory Committee (2008) Physical Activity guidelines advisory committee report, Washington, D.C
Strath SJ, Kaminsky LA, Ainsworth BE, Ekelund U, Freedson PS, Gary RA et al (2013) Guide to the assessment of physical activity: clinical and research applications: a scientific statement from the American heart association. Circulation 128(20):2259–2279
Kelly P, Kahlmeier S, Götschi T, Orsini N, Richards J, Roberts N et al (2014) Systematic review and meta-analysis of reduction in all-cause mortality from walking and cycling and shape of dose response relationship. Int J Behav Nutr Phys Act 11(1):1–15
Matthews CE, Jurj AL, Shu XO, Li HL, Yang G, Li Q et al (2007) Influence of exercise, walking, cycling, and overall nonexercise physical activity on mortality in Chinese women. Am J Epidemiol 165(12):1343–1350
Carlsson S, Andersson T, Wolk A, Ahlbom A (2006) Low physical activity and mortality in women: baseline lifestyle and health as alternative explanations. Scand J Public Health 34(5):480–487
World Health Organisation (2009) Global health risks: mortality and burden of disease attributable to selected major risks. WHO Press, Geneva
Ratzlaff CR, Koehoorn M, Cibere J, Kopec JA (2012) Is lifelong knee joint force from work, home, and sport related to knee osteoarthritis? Int J Rheumatol 2012:1–14
Palmer KT (2012) Occupational activities and osteoarthritis of the knee. Br Med Bull 102(1):147–170
Martin KR, Kuh D, Harris TB, Guralnik JM, Coggon D, Wills AK (2013) Body mass index, occupational activity, and leisure-time physical activity: an exploration of risk factors and modifiers for knee osteoarthritis in the 1946 British birth cohort. BMC Musculoskelet Disord 14(1):1–11
Washburn RA, Smith KW, Jette AM, Janney CA (1993) The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol 46(2):153–162
Felson DT (2013) Osteoarthritis as a disease of mechanics. Osteoarthr Cartil 21(1):10–15
Litwic A, Edwards MH, Dennison EM, Cooper C (2013) Epidemiology and burden of osteoarthritis. Br Med Bull 105(1):185–199
Buckwalter JA, Lane NE (1997) Does participation in sports cause osteoarthritis? Iowa Orthopaed J 17:80–89
Dolan S, Williams D, Ainsworth B, Shaw J (2006) Development and reproducibility of the bone loading history questionnaire. Med Sci Sports Exerc 38(6):1121–1131
Haskell W, Lee I, Pate R, Powell K, Blair S, Franklin B et al (2007) Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association Medicine. Circulation 116:1081–1093
Bull F, Groups. EW (2010) Technical report. Physical activity guidelines in the UK: Review and recommendations. Loughborough School of Sport, Exercise and Health Sciences. Loughborough University
Bravata DM, Smith-Spangler C, Sundaram V et al (2007) Using pedometers to increase physical activity and improve health: a systematic review. JAMA 298(19):2296–2304
Tudor-Locke C, Bassett DR Jr (2004) How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med 34(1):1–8
Tudor-Locke C, Craig CL, Aoyagi Y, Bell RC, Croteau KA, De Bourdeaudhuij I et al (2011) How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act 8(1):1–19
Dwyer T, Pezic A, Sun C, Cochrane J, Venn A, Srikanth V et al (2015) Objectively measured daily steps and subsequent long term all-cause mortality: the tasped prospective cohort study. PLoS One 10(11):e0141274
Marshall SJ, Levy SS, Tudor-Locke CE, Kolkhorst FW, Wooten KM, Ji M et al (2009) Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 min. Am J Prev Med 36(5):410–415
Autier P, Pizot C., Meaningless METS: studying the link between physical activity and health: BMJ. 2016 Aug 9;354:i4200. doi:10.1136/bmj.i4200
Acknowledgements
We gratefully thank Paramdeep Kaur and Maria Sanchez for their assistance with PA data. We also thank the Principal Investigators and staff of The Hertfordshire Cohort Study; Elaine Dennison and of The Johnston County Osteoarthritis Project; Joanne Jordan and Becki Cleveland for the provision of and assistance with data from their cohorts. Role of the sponsor: The funding organization had no role in the design or conduct of the study, the collection, management, analysis, or interpretation of data, the preparation, review or approval of the manuscript, or the decision to submit the manuscript for publication.
Author contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Gates, Leyland and Arden were involved in conception and design of the study and take responsibility for the integrity of the work as a whole, from inception to finished article. Gates, Leyland and Sheard were involved in the acquisition of data. Gates and Leyland were involved in the analysis and interpretation of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding source
This study was funded by Arthritis Research UK Centre for Sport, Exercise and Osteoarthritis (Grant Ref. 20194).
Conflict of interest
B Ainsworth receives royalties from Taylor & Francis. C Cooper has received consultancy from Servier, Amgen, Novartis, Eli Lilly, Medtronic. N. Arden has received consultancy from Bioventus, Flexion, Freshfields, Merck, Nicox and Smith & Nephew and honoraria from Flexion and Merck. E Roos reports on and is deputy editor of Osteoarthritis and Cartilage, is the developer of Knee injury and Osteoarthritis Outcome Score (KOOS), and is the founder of the Good Life with Osteoarthritis in Denmark (GLA:D) initiative to implement clinical guidelines in primary care. M. Batt, N. Arden, J Newton, K Jackson, L Gates, K Leylands institution has received a Centre of Excellence grant from Arthritis Research UK. L. Callahan, P. Kelly, R. Pate, S. Sheard, and C. Foster declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Gates, L.S., Leyland, K.M., Sheard, S. et al. Physical activity and osteoarthritis: a consensus study to harmonise self-reporting methods of physical activity across international cohorts. Rheumatol Int 37, 469–478 (2017). https://doi.org/10.1007/s00296-017-3672-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3672-y