Abstract
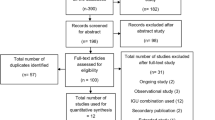
Evidence supports early use of non-biologic DMARDs to prevent irreversible damage in inflammatory arthritides, including rheumatoid arthritis (RA), psoriatic arthritis (PsA), and possibly ankylosing spondylitis (AS). However, there is a paucity of data exploring their effects on pain as a primary outcome in these conditions. This systematic literature review investigated the effect of non-biologic DMARDs on pain levels in IA and examined whether disease duration impacted efficacy. We searched Medline, Embase, Cochrane Central, and Cochrane Database of Systematic Reviews, abstracts from the 2008 to 2010 American College of Rheumatology annual congresses, and citation lists of retrieved publications. Only randomized, double-blind controlled trials were analyzed. Quality was assessed with the Risk of Bias tool. Descriptive statistics were used in meta-analysis. 9,860 articles were identified, with 33 eligible for inclusion: 8 in AS, 6 in PsA, 9 in early RA (ERA), and 10 in established RA. In ERA and established RA, all studies of DMARDs (monotherapy and combination therapies) consistently revealed statistically significant reductions in pain except three oral gold studies. In AS, sulfasalazine studies showed significant pain reduction, whereas use of other DMARDs did not. In PsA, 5 of 6 studies reported VAS-pain improvement. From the studies included, we were unable to assess the influence of disease duration on pain outcomes in these rheumatic conditions. DMARDs improve pain in early and established RA. Sulfasalazine may improve pain in AS and PsA. Further study is needed to assess the relationship between disease duration and DMARD efficacy in reducing pain in these conditions.



Similar content being viewed by others
References
Anderson JJ, Wells G, Verhoeven AC, Felson DT (2000) Factors predicting response to treatment in rheumatoid arthritis: the importance of disease duration. Arthr Rheum 43:22–29
Nell VPK, Machold KP, Eberl G, Stamm TA, Uffmann M, Smolen JS (2004) Benefit of very early referral and very early therapy with disease-modifying anti- rheumatic drugs in patients with early rheumatoid arthritis. Rheumatology (Oxford) 43:906–914
Bukhari MAS, Wiles NJ, Lunt BJ, Scott DGI, Symmons DPM, Silman AJ (2003) Influence of disease modifying therapy on radiographic progression in inflammatory polyarthritis at five years. Arthr Rheum 48:46–53
Wiles NJ, Lunt M, Barrett EM, Bukhari M, Silman AJ, Symmons DP et al (2001) Reduced disability at 5 years with early treatment of inflammatory polyarthritis: results from a large observational cohort, using propensity models to adjust for disease severity. Arthr Rheum 44:1033–1042
The diagnosis and treatment of early psoriatic arthritisAnandarajah (2009) Allen P and Ritchlin, Christopher T. Nature reviews. Rheumatology 5(11):634–641
Olivieri I, D’Angleo S, Palazzi C, Padula A (2010) Advantages in early recognition and treatment of psoriatic arthritis Int. J Clin Rheumatol 5(4):461–473
Salvarani C, Cantini F, Olivieri I (2002) Disease-modifyingantirheumatic drug therapy for psoriatic arthritis. Clin Exp Rheumatol 20(6):S71–S75
Whittle SL, Colebatch AN, Buchbinder R, Edwards CJ, Adams K, Englbrecht M, Hazlewood G, Marks JL, Radner H, Ramiro S, Richards BL, Tarner IH, Aletaha D, Bombardier C, Landewe RB, Mu¨ller-Ladner U, Bijlsma JWJ, Branco JC, Bykerk VP, da Rocha G, Pinheiro C, Catrina AI, Hannonen P, Kiely P, Leeb B, Lie E, Martinez-Osuna P, Montecucco C, Østergaard M, Westhovens R, Zochling J and van der Heijde D (2012) Multinational evidence-based recommendations for pain management by pharmacotherapy in inflammatory arthritis: integrating systematic literature research and expert opinion of a broad panel of rheumatologists in the 3e Initiative. Rheumatology. doi:10.1093/rheumatology/kes032
Higgins JPT, Altman DG (eds) (2008) Chapter 8: assessing risk of bias in included studies. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions. Version 5.0.1 [updated September 2008]. Cochrane Collab. Available from www.cochrane-handbook.org
Thiessen Philbrook H, Barrowman N, Garg AX (2007) Imputing variance estimates do not alter the conclusions of a meta-analysis with continuous outcomes: a case study of changes in renal function after living kidney donation. J Clin Epi 60:228–240
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Fink A, Kosecoff J, Chassin M, Brook RH (1984) Consensus methods: characteristics and guidelines for use. Am J Public Health 74:979–983
Altan L, Bingöl Ü, Karakoç Y et al (2001) Clinical investigation of methotrexate in the treatment of ankylosing spondylitis. Scand J Rheumatol 30:255–259
Clegg DO, Reda DJ, Weisman MH et al (1996) Comparison of sulfasalazine and placebo in the treatment of ankylosing spondylitis. Arthr Rheum 39:2004–2012
Corkill MM, Jobanputra P, Gibson T, Macfarlane DG (1990) A controlled trial of sulphasalazine treatment of chronic ankylosing spondylitis: failure to demonstrate a clinical effect. Br J Rheumatol 29:41–45
Dougados M, Boumier P, Amor B (1986) Sulphasalazine in ankylosing spondylitis: a double blind controlled study in 60 patients. Br Med J 293:911–914
Dougados M, van der Linden S, Leirisalo-Repo M et al (1995) Sulfasalazine in the treatment of spondylarthropathy. Arthr Rheum 38:618–627
Marzo-Ortega H, McGonangle D, Jarrett S et al (2005) Infliximab in combination with methorexate in active ankylosing spondylitis: a clinical and imaging study. Ann Rheum Dis 64:1568–1575
Nissilä M, Lehtinen K, Leirisalo-Repo M et al (1988) Sulfasalazine in the treatment of ankylosing spondylitis. Arthr Rheum 31:1111–1116
Taylor HG, Beswick EJ, Dawes PT (1991) Sulphasalazine in ankylosing spondylitis. A radiological, clinical and laboratory assessment. Clin Rheumatol 10:43–48
van Denderen JC, van der Paardt M, Nurmohamed MT et al (2005) Double blind, randomized, placebo controlled study of leflunomide in the treatment of active ankylosing spondylitis. Ann Rheum Dis 64:1761–1764
Carette S, Calin A, McCafferty JP, Wallin B (1989) A double-blind placebo-controlled study of auranofin in patients with psoriatic arthritis. Arthr Rheum 32:158–165
Combe B, Goupille P, Kuntz JL et al (1996) Sulphasalazine in psoriatic arthritis: a randomized, multicentre, placebo-controlled study. Br J Rheumatol 35:664–668
Farr M, Kitas GD, Waterhouse L et al (1990) Sulphasalazine in psoriatic arthritis: a double-blind placebo-controlled study. Br J Rheumatol 29:46–49
Fraser AD, van Kuijk WR, Westhovens R et al (2005) A randomized, double blind, placebo controlled, multicentre trial of combination therapy with methotrexate plus ciclosporin in patients with active psoriatic arthritis. Ann Rheum Dis 64:859–864
Fraser SM, Hopkins R, Hunter JA et al (1993) Sulphasalazine in the management of psoriatic arthritis. Br J Rheumatol 32:923–925
Palit J, Hill J, Capell HA et al (1990) A multicentre double-blind comparison of auranofin, intramuscular gold thiomalate and placebo in patients with psoriatic arthritis. Br J Rheumatol 29:280–283
Borg G, Allander E, Lund B et al (1988) Auranofin improves outcome in early rheumatoid arthritis. Results from a 2-year, double blind, placebo controlled study. J Rheumatol 15:1747–1754
Clark P, Casas E, Tugwell P et al (1993) Hydroxychloroquine compared to placebo in rheumatoid arthritis. Ann Intern Med 119:1067–1071
Esdaile JM, Suissa S, Shiroky JB et al (1995) A randomized trial of hydroxychloroquine in early rheumatoid arthritis: the HERA study. Am J Med 98:156–168
Gerards AH, Landewé RBM, Prins APA et al (2003) Cyclosporin A monotherapy versus cyclosporine A and methotrexate combination therapy in patients with early rheumatoid arthritis: a double blind randomized placebo controlled trial. Ann Rheum Dis 62:291–296
Haagsma CJ, van Riel PICM, De Jong AJL, Van de Putte LBA (1997) Combination of sulphasalazine and methotrexate versus the single components in early rheumatoid arthritis: a randomized controlled, double-blind, 52 week clinical trial. Br J Rheumatol 36:1082–1088
Hannonen P, Möttönen T, Hakola M, Oka M (1993) Sulfasalazine in early rheumatoid arthritis. A 48-week double-blind, prospective, placebo-controlled study. Arthr Rheum 36(11):1501–1509
Kekow J, Moots RJ, Emery P et al (2010) Patient-reported outcomes improve with etanercept plus methotrexate in active early rheumatoid arthritis and the improvement is strongly associated with remission: the COMET trial. Ann Rheum Dis 69:222–225
Lerndal T, Svensson B (2000) A clinical study of SPH 82 vs methotrexate in early rheumatoid arthritis. Rheumatology 39:316–320
Miranda JM, Alvarez-Nemegyei J, Saaverdra MA et al (2004) A randomized, double-blind, multicenter, controlled clinical trial of cyclosporine plus chloroquine vs. cyclosporine plus placebo in early-onset rheumatoid arthritis. Arch Med Res 35:36–42
Bombardier C, Ware J, Russell IJ et al (1986) Auranofin therapy and quality of life in patients with rheumatoid arthritis. Am J Med 81:565–578
Dougados M, Awada H, Amor B (1988) Cyclosporin in rheumatoid arthritis: a double blind, placebo controlled study in 52 patients. Ann Rheum Dis 47:127–133
Førre Ø et al (1994) Radiologic evidence of disease modification in rheumatoid arthritis patients treated with cyclosporine. Arthr Rheum 37:1506–1512
Glennas A, Kvien TK, Andrup O et al (1997) Auranofin is safe and superior to placebo in elderly-onset rheumatoid arthritis. Br J Rheumatol 36:870–877
Pullar T, Hunter JA, Capell HA (1983) Sulphasalazine in rheumatoid arthritis: a double blind comparison of sulphasalazine with placebo and sodium aurothiomalate. Br Med J 287:1102–1104
Smolen JS, Kalden JR, Scott DL et al (1999) Efficacy and safety of leflunomide compared with placebo and sulphasalazine in active rheumatoid arthritis: a double-blind, randomized, multicentre trial. Lancet 353:259–266
Strand V, Cohen S, Schiff M et al (1999) Treatment of active rheumatoid arthritis with leflunomide compared with placebo and methotrexate. Arch Intern Med 159:2542–2550
Tugwell P, Bombardier C, Gent M et al (1990) Low-dose cyclosporine versus placebo in patients with rheumatoid arthritis. Lancet 335:1051–1055
Ward JR, Williams HJ, Egger MJ et al (1983) Comparison of auranofin, gold sodium thiomalate and placebo in the treatment of rheumatoid arthritis. Arthr Rheum 26:1303–1313
Williams HJ, Willkens RF, Samuelson CO Jr et al (1985) Comparison of low-dose oral pulse methotrexate and placebo in the treatment of rheumatoid arthritis. Arthr Rheum 28:721–730
Williams HJ, Ward JR, Dahl SL et al (1988) A controlled trial comparing sulfasalazine, gold sodium thiomalate, and placebo in rheumatoid arthritis. Arthr Rheum 31:702–713
Salaffi F, Stancati A, Silvestri CA et al (2004) Minimal clinically important changes in chronic musculoskeletal pain intensity measure on a numerical pain rating scale. Eur J Pain 8:283–291
Pope JE, Khanna D, Norrie D, Ouimet JM (2009) The minimally important difference for the health assessment questionnaire in rheumatoid arthritis clinically practice is smaller than in randomized controlled trials. J Rheumatol 36:254–259
Kwok T, Pope JE (2010) Minimally important difference for patient-reported outcomes in psoriatic arthritis: health assessment questionnaire and pain, fatigue, and global visual analog scales. J Rheumatol 37:1024–1028
Wheaton L, Pope J (2009) The minimally important difference (MID) for patient centred outcomes in ankylosing spondylitis (AS) including pain, fatigue, sleep and health assessment questionnaire (HAQ). J Rheumatol 36:2579
Felson DT, Anderson JJ, Meenan RF (1990) The comparative efficacy and toxicity of second-line drugs in rheumatoid arthritis. Arthr Rheum 33:1449–1461
Anderson JJ, Baron G, van der Heijde D et al (2001) Ankylosing spondylitis assessment group preliminary definition of short-term improvement in ankylosing spondylitis. Arthr Rheum 44(8):1876–1886
Cunha-Miranda L, Costa L, Ribeiro JS (2010) NEAR study: needs and expectations in rheumatoid arthritis—do we know our patients’ needs? Acta Reumatologica Portuguesa 35:314–323
Kvamme MK, Kristiansen IS, Lie E, Kvien TK (2010) Identification of cutpoints for acceptable health status and important improvement in patient-reported outcomes, in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. J Rheumatol 37:26–31
Acknowledgments
Funded by 3e Initiative in Rheumatology (evidence, expertise, exchange) and from an unrestricted grant from Abbott Canada whereby no biologics were studied to avoid any perceived sponsor bias.
Conflict of interest
None of the authors declares a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix 1: Search strategy employed
Appendix 1: Search strategy employed
1. pain$.mp.
2. exp pain/
3. exp complex regional pain syndromes/
4. exp diabetic neuropathies/
5. failed back syndrome.mp.
6. diabetic neuropath$.mp.
7. reflex sympathetic dystrophy.ti,ab,kw.
8. sciatic$.mp.
9. headache*.mp.
10. head-ache$.mp.
11. colic*.mp.
12. arthralgi*.mp.
13. causalgi*.mp.
14. exp nociceptors/
15. nocicept*.mp.
16. cephalgi*.mp.
17. exp palliative care/
18. palliat*.mp.
19. exp Hyperalgesia/
20. exp Headache Disorders/
21. neuralgi$.mp.
22. migraine$.mp.
23. cephalalgi$.mp.
24. metatarsalgia$.mp.
25. bursitis.mp.
26. hyperalg$.mp.
27. or/1-26
28. chloroquin$.mp.
29. aral?n.mp.
30. amokin$.mp.
31. anoclor.mp.
32. Arechin.mp.
33. arechine.mp.
34. arequin$.mp.
35. artrichin$.mp.
36. Arthrabas.mp.
37. arthrochin$.mp.
38. arthroquin$.mp.
39. artriquin$.mp.
40. Av?oclor.mp.
41. bemaphat$.mp.
42. bemasulph.mp.
43. bipiquin.mp.
44. chemochin$.mp.
45. chingamin$.mp.
46. Chlorofoz.mp.
47. chlorochin$.mp.
48. clorichin$.mp.
49. choloquin$.mp.
50. Chlorquin$.mp.
51. cholo?quin$.mp.
52. choroquin$.mp.
53. cloriquin$.mp.
54. Cidanchin.mp.
55. Clopirim.mp.
56. Collagenan.mp.
57. Daraclor.mp.
58. Daramal.mp.
59. Delag?l.mp.
60. diquinalex.mp.
61. Dichinalex.mp.
62. Diclokin.mp.
63. Difosquin.mp.
64. Diroquine.mp.
65. Genocin.mp.
66. gontochin$.mp.
67. gontoquin$.mp.
68. Heliopar.mp.
69. imagon.mp.
70. iroquine.mp.
71. Klorokin$.mp.
72. khingamin.mp.
73. lagaquin.mp.
74. Maclorex.mp.
75. Malarex.mp.
76. Malarivon.mp.
77. Maliaquine.mp.
78. malaquin.mp.
79. mesylith.mp.
80. Mexaquin.mp.
81. Mirquin.mp.
82. nivachine.mp
83. Nivaquin$.mp.
84. Paluken.mp.
85. Palux.mp.
86. Pharmaquine.mp.
87. Plasmoquine.mp.
88. Promal.mp.
89. P-Roquine.mp.
90. Quinacris.mp.
91. quinachlor.mp.
92. quingamin$.mp.
93. Resoch?n$.mp.
94. resoquin$.mp.
95. reumachlor.mp.
96. Riboquin.mp.
97. roquine.mp.
98. rp 3377.mp.
99. rp3377.mp.
100. sanoquin$.mp.
101. Savarine.mp.
102. silbesan.mp.
103. sira?an.mp.
104. sn 7618.mp. [mp = title, original title, abstract, name of substance word, subject heading word, unique identifier]
105. sn7618.mp.
106. solprin$.mp.
107. Syncoquin.mp.
108. tresochin$.mp.
109. tresoquin$.mp.
110. trochin$.mp.
111. troquine.mp.
112. Weimerquin.mp.
113. w 7618.mp.
114. w7618.mp.
115. win 244.mp.
116. win244.mp.
117. 54-05-7.rn.
118. or/28-117
119. leflunomide.mp.
120. arava.mp.
121. arabloc.mp.
122. artrimod.mp.
123. hwa 486.mp.
124. Leflucross.mp.
125. rs 34821.mp.
126. hwa486.mp.
127. rs34821.mp.
128. su 101.mp.
129. su101.mp.
130. 75706-12-6.rn.
131. or/119-130
132. azathiop$.mp.
133. arathioprin$.mp.
134. azathrop$.mp.
135. azatioprina.mp.
136. azatox.mp.
137. azothioprin$.mp.
138. bw 57 322.mp.
139. bw 57322.mp.
140. bw57322.mp.
141. immur$.mp.
142. imuran$.mp.
143. imure$.mp.
144. nsc 39084.mp.
145. nsc39084.mp.
146. thioazeprine.mp.
147. Aseropri$.mp.
148. Azaallen.mp.
149. Azafalk.mp.
150. Azafor.mp.
151. Azaglax.mp.
152. Azahexal.mp.
153. Azaimun.mp.
154. Azamedac.mp.
155. Azamun$.mp.
156. Azapin.mp.
157. Azapress.mp.
158. Azaprin$.mp.
159. Aza-Q.mp.
160. Azarek.mp.
161. Azasan.mp.
162. Azathiodura.mp.
163. Azatrilem.mp.
164. Azopi$.mp.
165. Azoran.mp.
166. Berkaprine.mp.
167. Colinsan.mp.
168. Glaxoprin.mp.
169. Immunoprin.mp.
170. Imuger.mp.
171. Imunen.mp.
172. Imuprin.mp.
173. Oprisine.mp.
174. Satedon.mp.
175. Thioprine.mp.
176. Tiosalprin.mp.
177. Zaprine.mp.
178. Zytrim.mp.
179. 446-86-6.rn.
180. or/132-179
181. hydroxychloroquin$.mp.
182. Hydroxyquin$.mp.
183. Dolquine.mp.
184. Ercoquin.mp.
185. Hydroquin.mp.
186. Oxiklorin.mp.
187. Plaquenil.mp.
188. Plaquinol.mp.
189. Quensyl.mp.
190. Quineprox.mp.
191. Reuquinol.mp.
192. hydrochloroquine.mp.
193. oxychloroquine.mp.
194. oxychlorochin.mp.
195. sn 8137.mp.
196. hydroxychlorochin$.mp.
197. 118-42-3.rn.
198. or/181-197
199. sulfasal?zine$.mp.
200. salazosulfapyridine.mp.
201. azopyrin$.mp.
202. azosulfidine.mp.
203. azulf?d$.mp.
204. benzosulfa.mp.
205. colo pleon.mp.
206. colopleon.mp.
207. rorasul.mp.
208. salazo sulfapyridine.mp.
209. salazopyr$.mp.
210. salazosulfa pyridine.mp.
211. salazosulfpyridine.mp.
212. salicyl azo sulfapyridine.mp.
213. salicylazosulfapyridin$.mp.
214. salisulf.mp.
215. sulfosalazine.mp.
216. sulphasalazine.mp.
217. Aculfin.mp.
218. Azaline.mp.
219. Azulfin.mp.
220. Lazafin.mp.
221. Pyralin.mp.
222. Salazine.mp.
223. Salazopirin$.mp.
224. Salisulf Gastroprotetto.mp.
225. Salopyrine.mp.
226. Saridine.mp.
227. sas.mp.
228. Sulazine.mp.
229. Sulcolon.mp.
230. Sulfasalazin$.mp.
231. Sulfazine.mp.
232. Ucine.mp.
233. Ulcol.mp.
234. sulfasalazine.mp.
235. pleon.mp.
236. asulfidine.mp.
237. Arabloc.mp.
238. Arava.mp.
239. Artrimod.mp.
240. Leflucross.mp.
241. hwa 486.mp.
242. hwa486.mp.
243. rs 34821.mp.
244. rs34821.mp.
245. su 101.mp.
246. su101.mp.
247. 599-79-1.rn.
248. or/199-247
249. Cyclosporin$.mp.
250. Immunosuppressive Agents/
251. Peptides, Cyclic/
252. limit 251 to yr = ”1971–1981”
253. Peptides/
254. limit 253 to yr = ”1966–1970”
255. 252 or 254
256. 250 and 255 (112)
257. Gengraf.mp.
258. Neoral.mp.
259. Sandimmun$.mp.
260. Sangcya.mp.
261. adi 628.mp.
262. adi628.mp.
263. cicloral.mp.
264. ciclosporin$.mp.
265. consupren.mp.
266. ol 27400.mp.
267. ol27400.mp.
268. pulminiq.mp.
269. sang 35.mp.
270. sang35.mp.
271. neoral.mp.
272. restasis.mp.
273. cya-nof.mp.
274. csa-neoral.mp.
275. ol 27-400.mp.
276. 59865-13-3.rn.
277. or/249,256-276
278. gold.mp.
279. sodium aurothiomalate.mp.
280. mercaptobutanedioic acid monogold.mp.
281. sodium thiomalatoaurate.mp.
282. aurolate.mp.
283. disodium thiomalate.mp.
284. myocrysine.mp.
285. miocrisin.mp.
286. myocrisin.mp.
287. aurothiomalate.mp.
288. miocrin.mp.
289. myochrisin$.mp.
290. myochrysin$.mp.
291. shiosol.mp.
292. tauredon$.mp.
293. aurothioglucose.mp.
294. thioglucosoaurate.mp.
295. aureotan.mp.
296. solganal.mp.
297. gold50.mp.
298. auromyose.mp.
299. aurumin$.mp.
300. goldthioglucose.mp.
301. goldtioglucose.mp.
302. oronol.mp.
303. solganol.mp.
304. Organogold.mp.
305. Auranofin.mp.
306. sk&f d 39162.mp.
307. sk&f-39162.mp.
308. sk&f39162.mp.
309. ridauran.mp.
310. crisinor.mp.
311. ridaura.mp.
312. 12244-57-4.rn.
313. or/278-312
314. methotrexat$.mp.
315. mexate.mp.
316. a methopterine.mp.
317. abitrexate.mp.
318. amethopterin$.mp.
319. ametopterine.mp.
320. antifolan.mp.
321. cl 14377.mp.
322. cl14377.mp.
323. emt?exat$.mp.
324. enthexate.mp.
325. folex.mp.
326. mtx.mp.
327. ledertrexate.mp.
328. methohexate.mp.
329. methotrate.mp.
330. methotrexat$.mp.
331. methrotrexate.mp.
332. methylaminopterin.mp.
333. methylaminopterine.mp.
334. metothrexate.mp.
335. metotrexat.mp.
336. metotrexate.mp.
337. mpi 5004.mp.
338. mpi5004.mp.
339. novatrex.mp.
340. nsc 740.mp.
341. nsc740.mp.
342. rheumatrex.mp.
343. trexall.mp.
344. Atrexel.mp.
345. Biometrox.mp.
346. Brimexate.mp.
347. emt?exat$.mp.
348. Ebetrexat.mp.
349. Farmitrexat.mp.
350. Fauldexato.mp.
351. Hextrate.mp.
352. ifamet.mp.
353. lantarel.mp.
354. leulin.mp.
355. lumexon.mp.
356. maxtrex.mp.
357. medsatrexate.mp.
358. metex.mp.
359. methobax.mp.
360. methobion.mp.
361. methoblastin$.mp.
362. metoject.mp.
363. Metolate.mp.
364. Metotab.mp.
365. Metrexato.mp.
366. Metrotex.mp.
367. mexate.mp.
368. miantrex.mp.
369. Neotrexat.mp.
370. otamex.mp.
371. O-trexat.mp.
372. Pterin.mp.
373. Reutrexato.mp.
374. Rhodamer.mp.
375. tecnomet.mp.
376. texate.mp.
377. tremetex.mp.
378. trexan.mp.
379. trexeron.mp.
380. trixilem.mp.
381. unitrexate.mp.
382. xaken.mp.
383. zexate.mp.
384. 59-05-2.rn.
385. or/314-384 (37575)
386. dmard$.mp.
387. (disease modif$ adj2 agent$).mp.
388. Antirheumatic Agents/
389. ANTI-INFLAMMATORY AGENTS/
390. limit 389 to yr = ”1987-1994”
391. (disease modify$ adj3 anti$ drug$).mp.
392. or/386-388, 390-391
393. 118 or 131 or 180 or 198 or 248 or 277 or 313 or 385 or 392
394. (inflam$ adj2 joint$ adj2 disease$).mp.
395. (rheum$ adj2 arthr$).mp.
396. (caplan$ adj2 syndrome$).mp.
397. (caplan$ adj2 disease$).mp.
398. (felty$ adj2 syndrome$).mp.
399. (felty$ adj2 disease$).mp.
400. rheumatoid$.mp.
401. (rheumat$ adj2 nodule$).mp.
402. still$ disease$.mp.
403. still$ syndrome$.mp.
404. (sicca adj2 syndrome$).mp.
405. sicca adj2disease$.mp.
406. rheumatism.mp.
407. (psori$ adj2 arthri$).mp.
408. (psori$ adj2 arthrop$).mp.
409. (psori$ adj2 polyarthr$).mp.
410. (psori$ adj2 rheumat$).mp.
411. (reactive adj2 arthrit$).mp.
412. (arthrit$ adj2 postinfect$).mp.
413. (reiter$ adj2 syndrome$).mp.
414. (reiter$ adj2 disease$).mp.
415. (ankyl$ adj2 spond$).mp.
416. (marie$ strumpell$ adj2 disease$).mp.
417. (marie$ strumpell$ adj2 syndrome$).mp.
418. (marie$ struempell$ adj2 disease$).mp.
419. (marie$ struempell$ adj2 syndrome$).mp.
420. (bechterew$ adj2 disease$).mp.
421. (bechterew$ adj2 syndrome$).mp.
422. (bekhterev$ adj2 disease$).mp.
423. (bekhterev$ adj2 syndrome$).mp.
424. morbus bechterew$.mp.
425. spondylarthr$.mp.
426. (spondy$ adj2 rheum$).mp.
427. (spin$ adj2 ankylosis).mp.
428. (spin$ adj2 arthrit$).mp.
429. vertebral ankyl$.mp.
430. inflammatory arthrit$.mp.
431. exp rheumatoid arthritis/
432. ((rheumatoid or reumatoid or revmatoid or rheumatic or reumatic or revmatic or rheumat$ or reumat$ or revmarthrit$) adj3 (arthrit$ or artrit$ or diseas$ or condition$ or nodule$)).tw.
433. (sjogren$ adj2 syndrome).mp.
434. exp Spondylitis, Ankylosing/
435. (ankylos$ or spondyl$).tw.
436. (bekhterev$ or bechterew$).tw.
437. (Marie adj struempell$).tw.
438. exp Arthritis, Psoriatic/
439. (psoria$ adj (arthriti$ or arthropath$)).tw.
440. ((arthriti$ or arthropath$) adj psoria$).tw.
441. (arthrit$ and psoriasis).tw.
442. (arthrit$ and psoriatic).tw.
443. (arthropath$ and psoriasis).tw.
444. exp Spondylarthropathies/
445. exp Arthritis, Infectious/
446. ((sexual$ or chlamydia or yersinia or postyersinia or postdysenteric or salmonella or shigella or b27 or postinfectious or post infectious) adj5 arthrit$).tw.
447. undifferentiated oligoarthritis.tw.
448. ((enteropath$ or crohn$ or colitis or inflammatory bowel) adj5 arthrit$).tw.
449. Reiter$.tw.
450. enthesitis.tw.
451. exp Reiter Disease/
452. exp arthritis, reactive/
453. (arthritis adj2 reactive).tw.
454. undifferentiated oligoarthritis.tw.
455. exp Inflammatory Bowel Diseases/
456. (inflamm$ adj5 (arthriti$ or arthropath$)).tw.
457. Inflammatory bowel disease$.tw.
458. ibd.tw.
459. (Crohn$ adj disease).tw.
460. Ileocolitis.tw.
461. ((terminal or regional) adj ileitis).tw.
462. ((granulomatous or regional) adj enteritis).tw.
463. ((granulomatous or ulcerative) adj colitis).tw.
464. or/394-463
465. 27 and 393 and 464
466. from 465 keep 1-500
467. from 465 keep 501-1000
468. from 465 keep 1001-1500
469. from 465 keep 1501-1760 (260)
Rights and permissions
About this article
Cite this article
Steiman, A.J., Pope, J.E., Thiessen-Philbrook, H. et al. Non-biologic disease-modifying antirheumatic drugs (DMARDs) improve pain in inflammatory arthritis (IA): a systematic literature review of randomized controlled trials. Rheumatol Int 33, 1105–1120 (2013). https://doi.org/10.1007/s00296-012-2619-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-012-2619-6