Abstract
Objective
To evaluate organ dose and total effective dose of whole-body low-dose CT (WBLDCT) performed on different CT-scanner models in patients with multiple myeloma (MM) and to compare it to the effective dose of radiographic skeletal survey and representative diagnostic CTs.
Material and methods
We retrospectively analyzed data from 228 patients (47.4% females, mean age 67.9 ± 10.4 years, mean weight 81.8 ± 22.4 kg) who underwent WBLDCT for the work-up or surveillance of MM. Patients were scanned using one of six multi-detector CT-scanners. Organ doses and total effective doses per scan were calculated using a commercially available dose-management platform (Radimetrics, Bayer Healthcare, Leverkusen, Germany). The median effective dose was compared to radiographic skeletal survey and representative diagnostic CTs.
Results
The mean effective dose of our WBLDCT-protocol was 4.82 mSv. A significantly higher effective dose was observed in females compared to males (4.95 vs. 4.70 mSv, P = 0.002). Mean organ dose ranged from 3.72 mSv (esophagus) to 13.09 mSv (skeleton). Mean effective dose varied amongst different CT-scanners (range 4.34–8.37 mSv). The median effective dose of WBLDCT was more than twice the dose of a skeletal survey (4.82 vs. 2.04 mSv), 23% higher than a diagnostic contrast-enhanced chest CT (3.9 mSv), 46% lower than a diagnostic contrast-enhanced abdomen/pelvis CT (9.0 mSv), and 45% lower than a lumbar spine CT (8.7 mSv).
Conclusions
WBLDCT in MM has a higher effective dose than a radiographic skeletal survey, but a lower effective dose than diagnostic CTs of lumbar spine, abdomen and pelvis. This underlines the broad applicability of WBLDCT in the management of MM patients.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is the second most common hematological malignancy with an incidence that has risen over the past decades [1, 2]. It is characterized by the abnormal proliferation of monoclonal plasma cells in the bone marrow, which can lead to replacement of normal myelopoiesis, bone destruction and bone marrow failure [3]. Diagnosis of active MM as defined by the International Myeloma Working Group (IMWG) originally relied on histological confirmation of bone marrow plasma cell infiltration with clonal bone marrow plasma cells ≥10% (or extramedullary plasmacytoma) and one of the following features: hypercalcemia, renal insufficiency, anemia and bone lesions [4]. According to the IMWG, the presence of lytic bone lesions is considered one of the criteria to define active disease that requires treatment, even in the absence of clinical symptoms [4]. Consequently, imaging plays an important role in staging and in the follow-up of the disease [3, 5], as well as for the initial work-up of patients with smoldering MM [6].
Skeletal survey using approximately 20 regional radiographs has been used to determine osteolytic lesions or pathological fractures from MM. However, the value of conventional radiographs in detecting osteolytic lesions is limited since at least 30% of trabecular bone must be destroyed to be visible by radiograph [7]. Cross-sectional imaging techniques such as computed tomography (CT), magnetic resonance imaging (MRI) and integrated positron emission tomography/CT (PET/CT), have proven to be more accurate in detecting osteolytic and marrow replacing lesions as compared to skeletal surveys using radiographs [8,9,10,11,12,13,14]. As a result, more accurate diagnosis, staging and follow-up of MM is possible [8, 9].
Whole body low-dose CT (WBLDCT) was found to be the most sensitive modality for detecting small osteolytic lesions (<5 mm) [15]. Moreover, WBLDCT provides information for disease monitoring and detection of incidental findings in MM patients, underlining its importance in the management of this patient group [16]. Although advances in CT technology enable low-dose whole-body evaluation, CT is limited by ionizing radiation exposure. While some literature on WBLDCT in MM report radiation dose information [17], current literature lacks dedicated data in larger patient cohorts on the organ dose exposure and effective radiation exposure in the clinical practice of WBLDCT’s in MM patients. Therefore, the objective of our study was primarily to evaluate the organ-specific-radiation dose levels and total effective dose of WBLDCT in a MM patient cohort and to compare them to calculated effective doses of a skeletal survey and representative diagnostic CT scans. We hypothesized that the effective dose of WBLDCT would be lower than that of diagnostic CTs and higher than that of a skeletal survey.
Materials and methods
Our study was IRB-approved and complied with HIPAA guidelines with exemption status for individual informed consent. A retrospective search was performed of all WBLDCT’s acquired from July 2017 to February 2019.
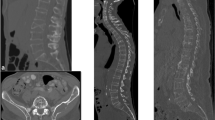
Whole-body low-dose CT protocols
CT examinations were performed without administration of intravenous or oral contrast medium on one of our six multidetector CT scanners (SOMATOM Force, SOMATOM Definition Flash, SOMATOM Definition Edge; Siemens, Forchheim, Germany; GE Discovery, GE Revolution; VCT, Boston, MA, USA; IQon Spectral, Philips, Best, the Netherlands). Patients were scanned in supine position, with head first and the arms straight beside the body and hands placed over the upper thighs. The field of view was adapted to the patient’s circumference.
WBLDCT imaging parameters per used device are depicted in Table 1.
Radiation dose assessment of whole-body low-dose CT
We assessed the radiation dose in terms of organ dose and whole-body effective dose using a commercial dose monitoring and tracking software platform (Radimetrics, Bayer Healthcare, Leverkusen, Germany). Based on anthropomorphic phantoms and Monte Carlo simulations, this software extracts volume computed tomography dose index (CTDIvol), dose-length product (DLP) from each scan and provides organ dose values (mSv) and total effective dose (mSv) per CT scan according to the weighting factors published in the International Commission on Radiation Protection 103 report [18]. Regarding the organ dose, values for the following organs were recorded: adrenals, brain, colon, esophagus, eye lenses, gall bladder, heart, kidneys, liver, lungs, muscle, pancreas, red marrow, salivary glands, skeleton, skin, small intestine, spleen, stomach, thyroid, thymus and urinary bladder. Furthermore, the organ dose of breasts, ovaries and the uterus were recorded in female subjects as well as the testis dose in males.
Radiation dose calculation of a skeletal survey and representative diagnostic CT scans
At our institution, the radiographic skeletal survey includes the following 22 different images; skull (two directions), cervical spine (two directions), thoracic spine (two directions), lumbar spine (two directions), chest (PA), pelvis (AP), humerus (AP, bilateral), forearm (AP, bilateral), hip (AP, bilateral), femur (AP, bilateral), knee (AP, bilateral), and tibia/fibula (AP, bilateral). The median effective dose (mSv) per exam was calculated using our institution’s median data of dose-area-product (DAP) and conversion factors as described by Wall et al. [19]. The sum of the effective dose per exam resulted in the total effective dose of the skeletal survey used in our institution.
In order to put the total effective dose of the MM WBLDCT protocols into perspective, the median effective dose of the following commonly used diagnostic CT protocols without the use of intravenous contrast was calculated with DLP, using our institution’s median data from 1/1/2017 to 9/14/2018 from the ACR dose index registry (DIR) and conversion factors from AAPM report 96 [20]—brain, cervical spine, thoracic spine, lumbar spine, chest (low dose/screening protocol), and abdomen/pelvis. Similarly, the median effective dose of diagnostic chest and abdomen/pelvis CT protocols with the use of intravenous contrast was calculated.
Statistical analysis
Descriptive statistics were reported in terms of percentages, means, standard deviations (SD), medians and interquartile ranges (IQR). The independent samples T test was used to analyze differences in effective dose and organ dose between male and female patients. The test assumed a two-tailed probability and a P-value of less than 0.05 indicated a significant difference.
Results
In this retrospective study, we analyzed data of 228 patients—108/228 (47.4%) females, mean age 67.9 (SD 10.4) years, mean weight 81.8 (SD 22.4) kg. An overview of the total organ dose and differences between organ dose in males and females is depicted in Table 2. In the total group, the mean organ dose ranged from 3.72 (SD 1.01) mSv for the esophagus up to 13.09 (SD 2.84) mSv for the skeleton. As shown in Table 2, differences were observed between males and females regarding the mean organ dose of the thyroid (10.25 (SD 1.55) mSv vs. 8.27 (SD 1.42) mSv, P < 0.001, respectively), the esophagus (3.58 (SD 0.52) mSv vs. 3.75 (SD 0.58) mSv, P = 0.019, respectively), and the colon (4.06 (SD 0.45) mSv vs. 4.21 (SD 0.63) mSv, P < 0.001, respectively).
The mean total effective dose of our WBLDCT protocol was 4.82 (SD 0.62) mSv. A significant higher effective dose was observed in females compared to males; 4.95 (SD 0.70) mSv vs. 4.70 (SD 0.51) mSv, respectively, P = 0.002.
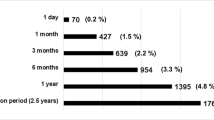
The majority of the WBLDCT scans were obtained using the Revolution CT, GE Medical Systems (198 [86.8%)], followed by the SOMATOM Definition Edge, Siemens [12 (5.3%)], SOMATOM Definition Flash, Siemens [7 (3.1%)], IQon - Spectral CT, Philips [7 (3.1%)], Discovery CT750 HD, GE Medical Systems [3 (1.3%)), and the SOMATOM Force, Siemens [1 (0.4%)]. The effective dose, CTDIvol and DLP per used device are depicted in Table 3. The mean effective dose ranged from 4.34 mSv (SOMATOM Force, Siemens) up to 8.37 mSv (Discovery CT750 HD, GE Medical Systems).
Table 4 shows the calculated effective doses of a skeletal survey and representative commonly used diagnostic CT scans at our institution. The median effective dose of our skeletal survey (including 22 radiographs) was 2.04 mSv. The calculated median effective dose of representative diagnostic CT scans at our institution ranged from 1.2 mSv for a low-dose chest CT up to 9.0 mSv for a contrast-enhanced CT of the abdomen/pelvis.
Discussion
Our study showed that WBLDCT in MM patients has a higher effective dose than that of a radiographic skeletal survey, but a lower effective dose than that of diagnostic CTs of the lumbar spine, abdomen and pelvis. Within the past decades the survival of MM patients has improved because of the availability of novel treatment options [21,22,23]. The presence of these treatment options had underlined the importance of early diagnosis and accurate staging [8]. According to the most recent IMWG diagnostic criteria, lesions measuring 5 mm on CT or MRI are now included in the diagnostic criteria of MM [4], and it is of clinical importance to detect bone involvement in MM and its precursors. Moreover, in MM patients, bone involvement is an important cause of morbidity and mortality and a key indicator of prognosis [4].
Although skeletal surveys using radiographs have been traditionally used to assess for bone involvement in MM patients, its limitations are well known and have been documented previously [8]. Therefore, more sensitive imaging techniques for the diagnosis and follow-up of MM have been described, such as WBLDCT, MRI and PET/CT. Whole-body MRI and 18F-fluorodeoxyglucose-PET/CT have been described to be more accurate in detecting bone lesions in MM as compared to skeletal surveys [8,9,10,11,12,13,14], and whole-body MRI have been found to detect significantly more MM bone involvement compared to PET/CT [12]. Whole-body MRI and PET/CT are, however, limited in their availability and are relatively costly. Additionally, FDG-PET/CT results in a relatively high radiation dose to the patient.
The widespread availability of multi-detector CT scanners has contributed to the increased use of WBLDCT for the diagnosis and follow-up of MM. The total effective dose of the WBLDCT in our study is comparable to those reported in recent literature [24,25,26,27]. Moreover, our measured organ specific dose is comparable to the organ dose described by Kröpil et al. [28]. In our study, the effective dose of WBLDCT was, as expected, higher than that of a radiographic skeletal survey; however, the total effective dose of WBLDCT proved to be lower than that of commonly used diagnostic CTs of the lumbar spine, abdomen and pelvis. Moreover, WBLDCT has been shown to provide important information for disease monitoring and detection of incidental findings [16], thereby improving the management of MM patients.
In recent literature, WBLDCT protocols with estimated effective doses comparable to or lower than radiographic skeletal surveys have been described, using for instance hybrid iterative reconstruction techniques [10] or spectral shaping [24]. Although these studies show the potential for further decreasing radiation exposure of WBLDCT in MM, the radiation doses in our study reflect those that result from current daily practice.
Our study was limited by the retrospective study design. Secondly, over 85% of our WBLDCT scans were performed using one scanner, the Revolution CT, GE Medical Systems. This resulted in a relative underrepresentation of the other systems used. Strengths of our study include the large number of patients scanned using a uniform clinical protocol and the detailed assessment of radiation dose.
In conclusion, WBLDCT in MM has a higher effective dose than a radiographic skeletal survey, but a lower effective dose than diagnostic CTs of the lumbar spine, abdomen and pelvis. This underlines the broad applicability of WBLDCT in the management of MM patients. The additional diagnostic value of WBLDCT in the management of MM patients outweighs the relatively limited additional radiation dose as compared to a radiographic skeletal survey.
References
Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Heal; 2019.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30.
Bird JM, Owen RG, D’Sa S, et al. Guidelines for the diagnosis and management of multiple myeloma 2011. Br J Haematol. 2011;154:32–75.
Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International myeloma working group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15:e538–48.
Terpos E, Kleber M, Engelhardt M, et al. European myeloma network guidelines for the management of multiple myeloma-related complications. Haematologica. 2015;100:1254–66.
Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised international staging system for multiple myeloma: a report from international myeloma working group. J Clin Oncol. 2015.
Edelstyn GA, Gillespie PJ, Grebbell FS. The radiological demonstration of osseous metastases: experimental observations. Clin Radiol. 1967;18:158–62.
Regelink JC, Minnema MC, Terpos E, et al. Comparison of modern and conventional imaging techniques in establishing multiple myeloma-related bone disease: a systematic review. Br J Haematol. 2013;162:50–61.
Gariani J, Westerland O, Natas S, et al. Comparison of whole body magnetic resonance imaging (WBMRI) to whole body computed tomography (WBCT) or 18F-fluorodeoxyglucose positron emission tomography/CT (18F-FDG PET/CT) in patients with myeloma: systematic review of diagnostic performance. Crit Rev Oncol Hematol. 2018;124:66–72.
Lambert L, Ourednicek P, Meckova Z, et al. Whole-body low-dose computed tomography in multiple myeloma staging: superior diagnostic performance in the detection of bone lesions, vertebral compression fractures, rib fractures and extraskeletal findings compared to radiography with similar radiation. Oncol Lett. 2017;13:2490–4.
Plesner T, Hielscher T, Suehara Y, et al. Whole-body computed tomography versus conventional skeletal survey in patients with multiple myeloma: a study of the international myeloma working group. Blood Cancer J. 2017;7:e599.
Dyrberg E, Al-Farra G, Balding L, et al. A prospective study comparing whole-body skeletal X-ray survey with 18F-FDG-PET/CT, 18F-NaF-PET/CT and whole-body MRI in the detection of bone lesions in multiple myeloma patients. Acta Radiol Open. 2017;6:205846011773880.
Bredella MA, Steinbach L, Caputo G, et al. Value of FDG PET in the assessment of patients with multiple myeloma. AJR Am J Roentgenol. 2005;184:1199–204.
Walker R, Barlogie B, Haessler J, et al. Magnetic resonance imaging in multiple myeloma: diagnostic and clinical implications. J Clin Oncol. 2007;25:1121–8.
Hur J, Yoon CS, Ryu YH, et al. Efficacy of multidetector row computed tomography of the spine in patients with multiple myeloma: comparison with magnetic resonance imaging and fluorodeoxyglucose-positron emission tomography. J Comput Assist Tomogr. 2007;31:342–7.
Simeone FJ, Harvey JP, Yee AJ, et al. Value of low-dose whole-body CT in the management of patients with multiple myeloma and precursor states. Skelet Radiol. 2018.
Horger M, Claussen CD, Bross-Bach U, et al. Whole-body low-dose multidetector row-CT in the diagnosis of multiple myeloma: an alternative to conventional radiography. Eur J; 2005.
ICRP Task Group. The 2007 recommendations of the international commission on radiological protection. Elsevier; 2007.
Wall BF, Jansen JTM, Hillier MC, et al. Radiation risks from medical X-ray examinations as a function of the age and sex of the patient. In: HPA-CRCE-028;2011.
AAPM Task Group 23. The measurement, reporting, and management of radiation ddose in CT. American Association of Physicists in Medicine; 2008.
Kumar SK, Dingli D, Lacy MQ, et al. Autologous stem cell transplantation in patients of 70 years and older with multiple myeloma: results from a matched pair analysis. Am J; 2008.
Kumar SK, Dingli D, Lacy MQ, et al. Outcome after autologous stem cell transplantation for multiple myeloma in patients with preceding plasma cell disorders. Br J Haematol. 2008;141:205–11.
Kumar SK, Rajkumar SV, Dispenzieri A, et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood. 2008;111:2516–20.
Suntharalingam S, Mikat C, Wetter A, et al. Whole-body ultra-low dose CT using spectral shaping for detection of osteolytic lesion in multiple myeloma. Eur Radiol. 2018;28:2273–80.
Ippolito D, Talei Franzesi C, Spiga S, et al. Diagnostic value of whole-body ultra-low dose computed tomography in comparison with spinal magnetic resonance imaging in the assessment of disease in multiple myeloma. Br J Haematol. 2017;177:395–403.
Moulopoulos LA, Koutoulidis V, Hillengass J, et al. Recommendations for acquisition, interpretation and reporting of whole body low dose CT in patients with multiple myeloma and other plasma cell disorders: a report of the IMWG Bone WWorking Group. Blood Cancer J. 2018;8:95.
Gleeson TG, Byrne B, Kenny P, et al. Image quality in low-dose multidetector computed tomography: a pilot study to assess feasibility and dose optimization in whole-body bone imaging. Can Assoc Radiol J. 2010;61:258–64.
Kröpil P, Fenk R, Fritz LB, et al. Comparison of whole-body 64-slice multidetector computed tomography and conventional radiography in staging of multiple myeloma. Eur Radiol. 2008;18:51–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were carried out in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived for individual participants included in the study. The study was approved by the local Institutional Review Board (IRB) and HIPAA compliant.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hemke, R., Yang, K., Husseini, J. et al. Organ dose and total effective dose of whole-body CT in multiple myeloma patients. Skeletal Radiol 49, 549–554 (2020). https://doi.org/10.1007/s00256-019-03292-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03292-z