Abstract
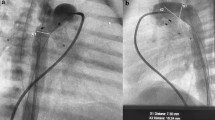
The outcome of patients with hypoplastic left heart (HLH) is determined by many factors, particularly by the first-step palliative procedure in newborns undergoing the Norwood procedure, its Sano modification, or, rarely, through challenging biventricular repairs. Duct stenting combined with bilateral pulmonary artery banding (PAB) is a new method employed as an alternative first-step approach in a number of centers worldwide. We describe this interventional–surgical “hybrid approach” as an additional strategy for the treatment of newborns with HLH syndrome and HLH complex. Between 1998 and April, 2006, 58 newborns underwent ductal stenting and bilateral PAB. These patients underwent surgical bilateral PAB initially, followed by percutaneous duct stenting; the only exception to this were patients in whom duct stenting was performed as a rescue procedure. Various balloon-expandable and self-expandable stents with different widths and lengths were used during the 8-year period of this study. Balloon dilatation of the atrial septum was performed when indicated. This included 5 patients in whom the atrial septum was stented. Aortic arch reconstruction (AAR) combined with a bidirectional cavopulmonary connection (BCPC) was performed at a median age of 4.8 months (range, 2.6–7.5), and total cavopulmonary connection (TCPC) was performed at a median age of 3.1 years (range, 2.5–4). Nine patients were listed for heart transplantation (HTX) and transplanted with AAR when a donor heart was available. Depending on growth of left ventricular structures, biventricular repair (BVR) was performed at a median age of 7.1 months (range, 3.5–10). Overall, 8 of 58 patients (13.8%) treated by the transcatheter–surgical hybrid approach died during the study period. The mortality rate for duct stenting was 1.7% (l/58), and it was 1.7% for bilateral PAB as well. Twenty-seven patients received an AAR/BCPC; 2 of them died (7.4%). Additionally, 1 of 2 patients with AAR/BCPC died while on the waiting list for HTX, resulting in a total mortality rate of 11% with an actuarial survival rate of 89%. One patient is still awaiting AAR + BCPC. Three patients died while on the waiting list for HTX despite successful bilateral PAB and duct stenting. The 30-day mortality rate for TCPC (n = 11), HTX (n = 8), and 18 patients with BVR was 0. The actuarial survival rate for patients with BVR is 93%. Postnatal transcatheter–surgical hybrid palliation expands the surgical options for newborns with HLH. Using hybrid palliation, Norwood stage I operation can be avoided in the neonatal period, the waiting period for children scheduled for cardiac transplantation can be extended, and observation for left ventricular growth suitable for biventricular repair as well.



Similar content being viewed by others
References
Akintuerk H, Michel-Behnke I, Valeske K, et al. (2002) Stenting of the arterial duct and banding of the pulmonary arteries. Basis for combined Norwood stage I and II repair in hypoplastic left heart. Circulation 105:1099–1103
Bacha EA, Daves S, Hardin J, et al. (2006) Single-ventricle palliation for high-risk neonates: the emergence of an alternative hybrid stage I strategy. J Thorac Cardio Vasc 131:163–171
Bauer J, Dapper F, Demirakca S, et al. (1997) Perioperative management of pulmonary hypertension after heart transplantation in childhood. J Heart Lung Transplant 16:1238–1247
Dapper F, Bauer J, Kroll J, et al. (1998) Clinical experience with heart transplantation in infants. Euro J Cardiothorac Surg 14:1–5
Galantowicz M, Cheatham JP (2005) Lessons learned from the development of a new hybrid strategy for the management of hypoplastic left heart syndrome. Pediatr Cardial 26:190–199
Gibbs JL, Wren C, Watterson KG, et al. (1993) Stenting of the arterial duct combined with banding of the pulmonary arteries and atrial septectomy or septostomy: a new approach to palliation for the hypoplastic left heart syndrome. Br Heart J 69:551–555
Griselli M, McGuirk S, Stümper O, et al. (2006) Influence of surgical strategies on outcome after the Norwood procedure. J Thorac Cardiovasc Surg 131:418–426
Hehrlein FW, Yamamoto T, Orime Y, Bauer J (1998) Hypoplastic left heart syndrome: which is the best operative strategy? Ann Thorac Cardiovasc Surg 4:125–132
Lim DS, Peeler BB, Matherne GP, Kron IL, Gutgesell HP (2006) Risk-stratified approach to hybrid transcatheter–surgical palliation of hypoplastic left heart syndrome. Pediatr Cardial 27:91–95
Mahle WT, Spray TL, Gaynor JW, Clark BJ 3rd (2001) Unexpected death after reconstructive surgery for hypoplastic left heart syndrome. Ann Thorac Surg 71:61–65
Michel-Behnke I, Akitürck H, Marquardt I, et al. (2003) Stenting of the ductus arteriosus and banding of the pulmonary arteries: basis for various surgical strategies in newborns with multiple left heart obstructive lesions. Heart 89:645–650
Muller M, Akinturk H, Schindler E, et al. (2003) A combined stage 1 and 2 repair for hypoplastic left heart-syndrome: anaesthetic considerations. Pediatr Anaesth 13:360–365
Nurozler F, Bradley SM (2000) Considerations in biventricular repair after the Norwood procedure. Eur J Cardiovasc Surg 18:540–544
Pearl JM, Cripe LW, Manning PB (2003) Biventricular repair after Norwood palliation. Ann Thorac Surg 75:132–137
Ruiz CE, Gamra H, Zhang HP, Garcia EJ, Boucek MM (1993) Brief report: stenting of the ductus arteriosus as a bridge to cardiac transplantation in infants with the hypoplastic left-heart syndrome. N Engl J Med 328:1605–1608
Stasik CN, Goldberg CS, Bove EL, Devaney EJ, Ohye RG (2006) Current outcomes and risk factors for the Norwood procedure. J Thorac Cardiovasc Surg 131:412–417
Tchervenkov CI, Tatha SA, Jutrus LC, Beland MJ (1998) Biventricular repair in neonates with hypoplastic left heart complex. Ann Thorac Surg 66:1350–1357
Tweddell JS, Hoffman GM, Mussatto KA, et al. (2002) Improved survival of patients undergoing palliation of hypoplastic left heart syndrome: lessons learned from 115 consecutive patients. Circulation 106:182–189
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akintürk, H., Michel-Behnke, I., Valeske, K. et al. Hybrid Transcatheter–Surgical Palliation. Pediatr Cardiol 28, 79–87 (2007). https://doi.org/10.1007/s00246-006-1444-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-006-1444-7